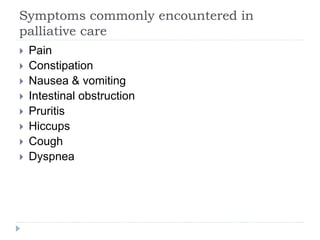
Palliative care aims to promote quality of life and comfort for patients facing serious illnesses. It provides relief from pain and other distressing symptoms, and addresses patients' physical, psychological, social, and spiritual needs. A multidisciplinary team works to help patients live as actively as possible until death, and also supports families during illness and bereavement. Key members include physicians, nurses, social workers, chaplains, and dietitians. The goals are to assess symptoms, discuss prognosis, understand patient values and goals, and ensure support systems are in place.