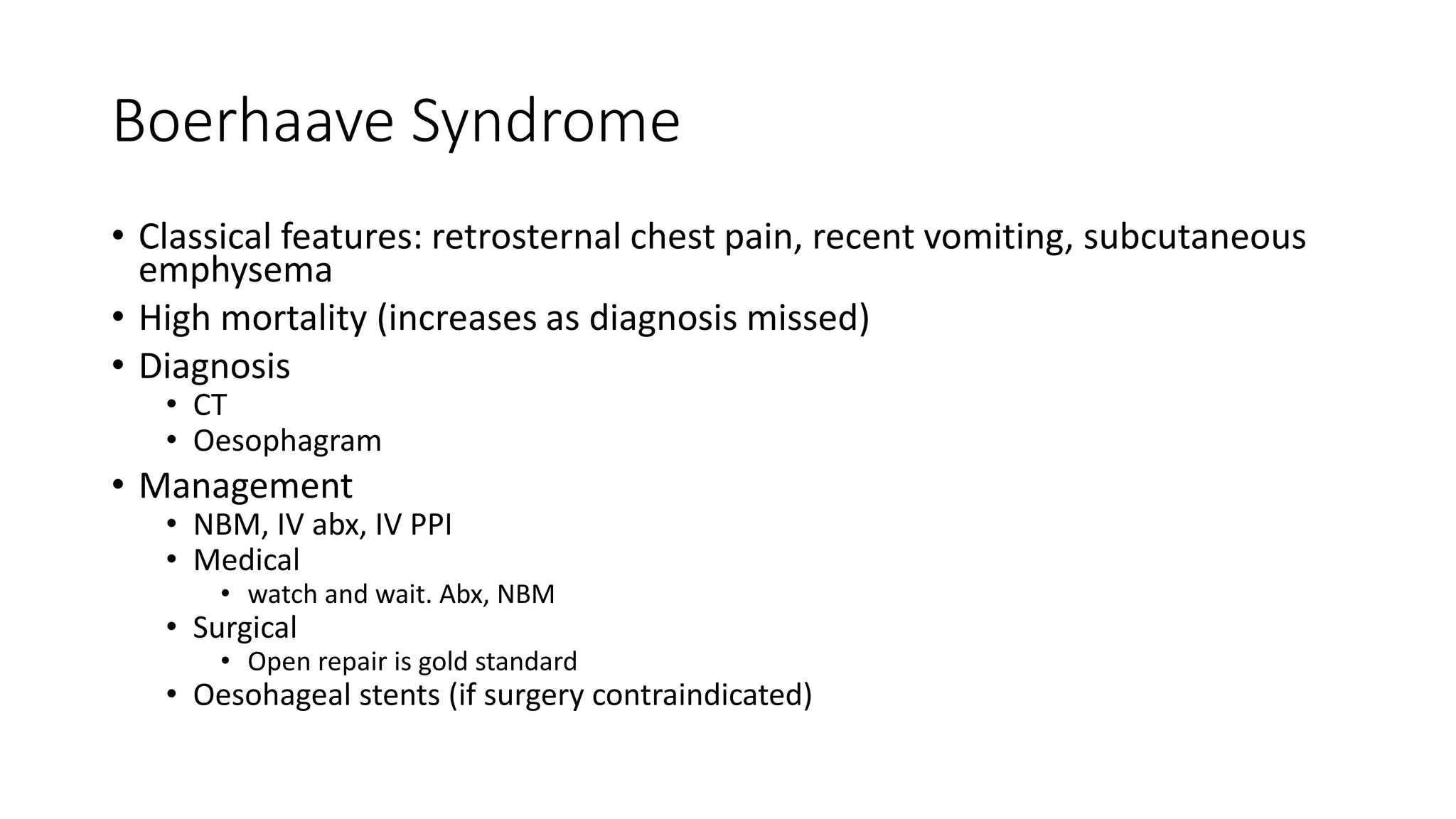
1. Boerhaave syndrome is a spontaneous rupture of the esophagus, classically presenting with retrosternal chest pain, recent vomiting, and subcutaneous emphysema.
2. CT and oesophagram are used to diagnose this condition, which has a high mortality if diagnosis is missed.
3. Management involves nothing by mouth, IV antibiotics, IV PPI, and either open surgical repair (gold standard) or esophageal stents if surgery is contraindicated.