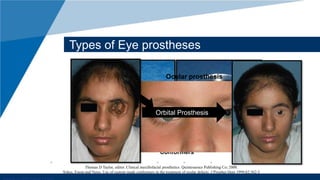
The document provides a comprehensive overview of ocular prosthesis, including its history, types, patient evaluation, and treatment planning. It discusses various techniques for impression, fabrication, retention methods, maintenance issues, and potential complications. The conclusion emphasizes the importance of meeting challenges in the pursuit of effective prosthetic solutions.