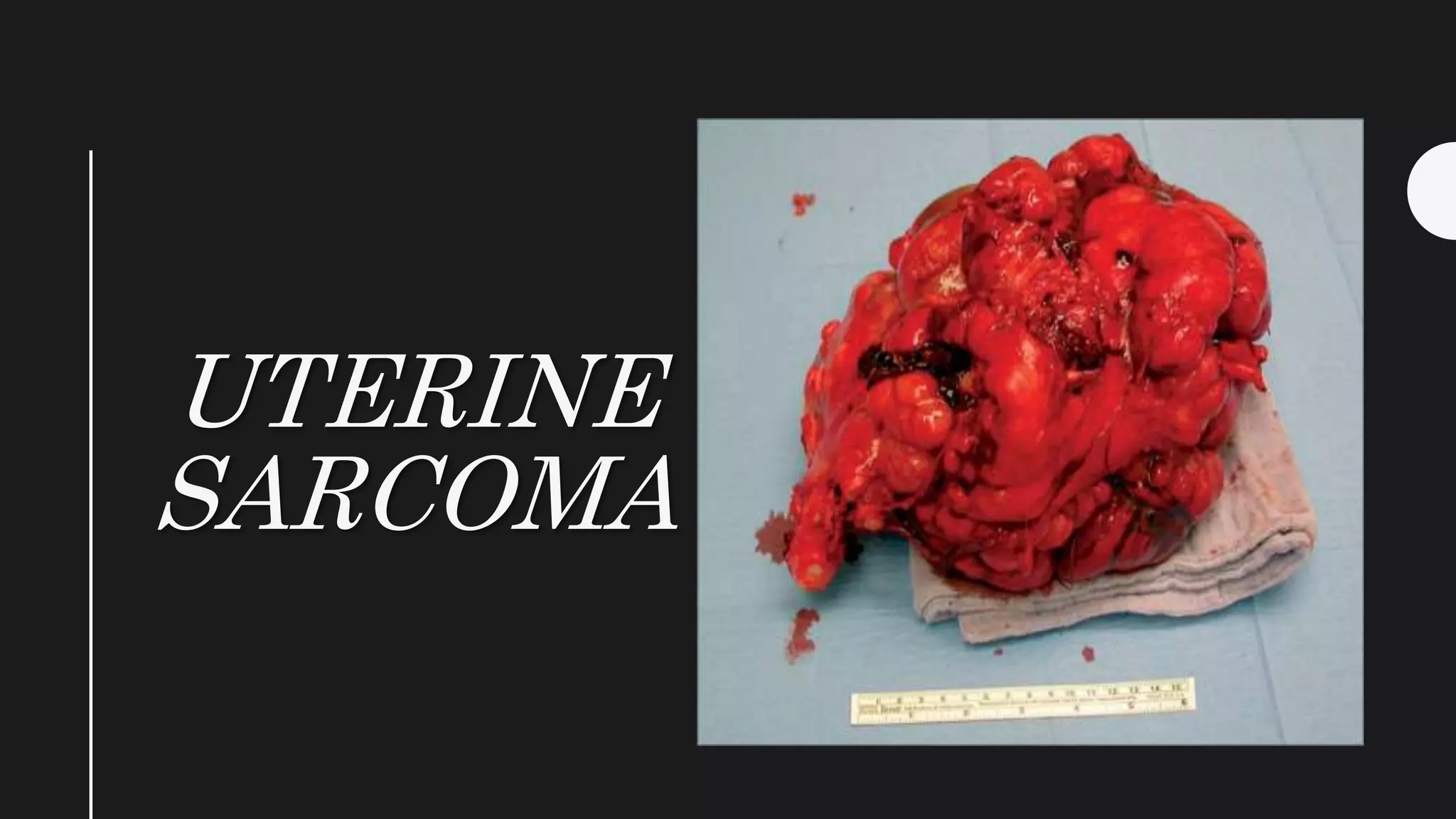
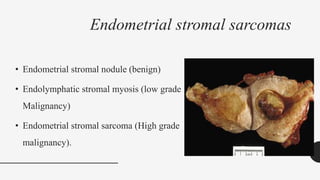
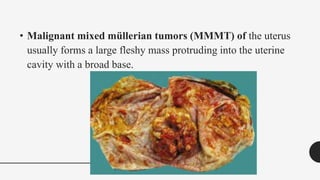
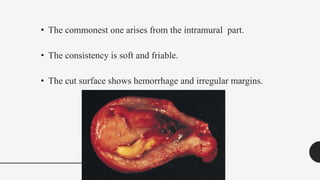
Uterine sarcomas are rare, aggressive cancers that arise from the muscular or connective tissues of the uterus. The main types are leiomyosarcomas, endometrial stromal sarcomas, and malignant mixed müllerian tumors. Uterine sarcomas commonly spread through the bloodstream to vital organs like the lungs and liver. Patients typically present with abnormal vaginal bleeding and abdominal pain. Diagnosis is made through histological examination of tissue samples obtained through procedures like uterine curettage.