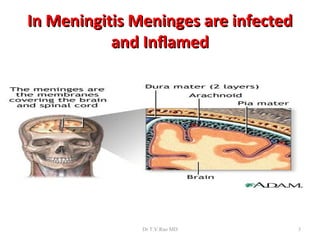
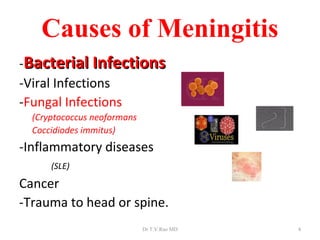
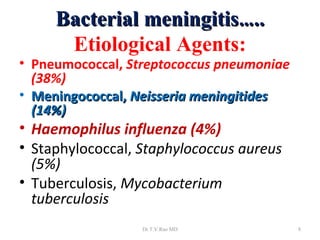
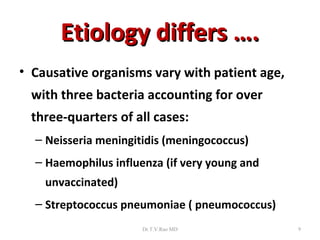
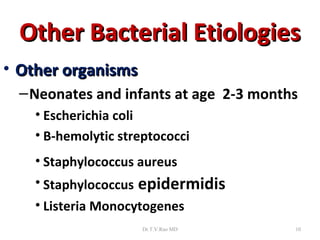
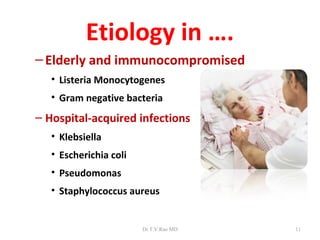
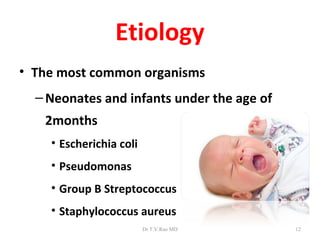
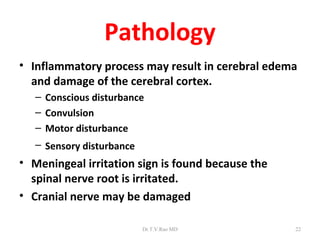
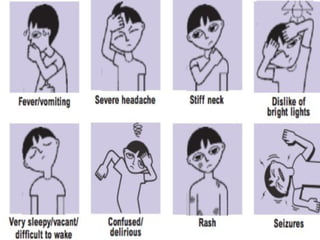
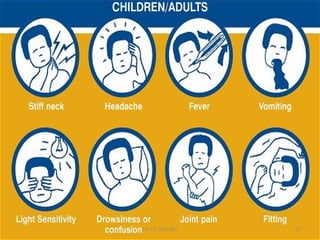
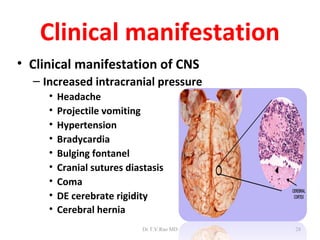
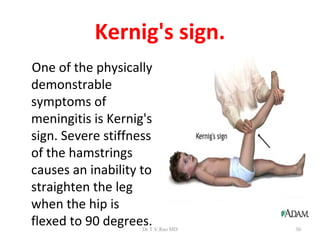
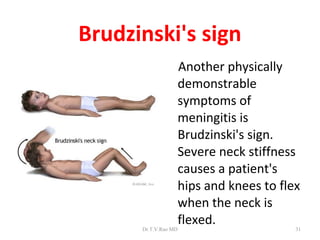
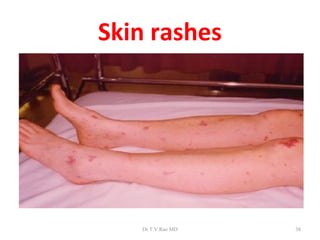
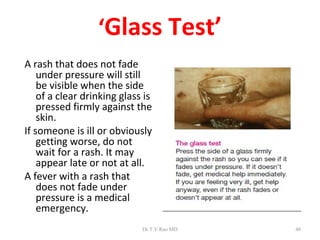
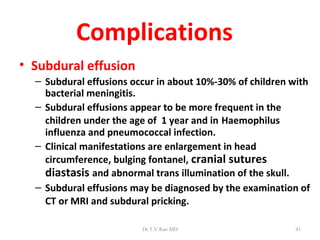
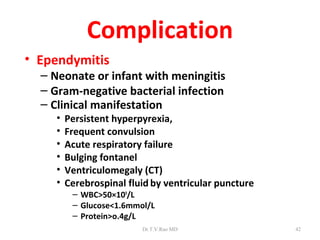
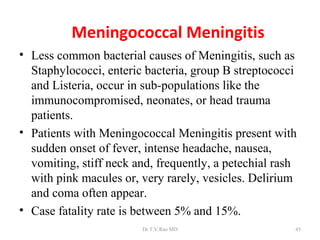
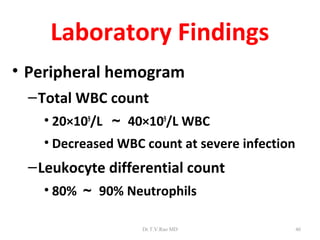
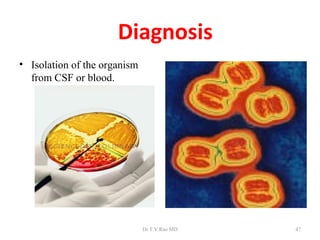
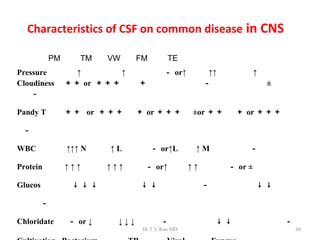
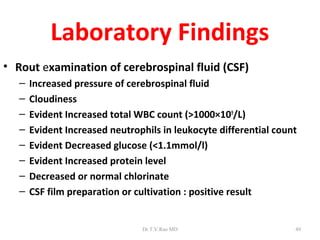
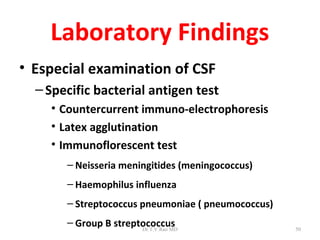
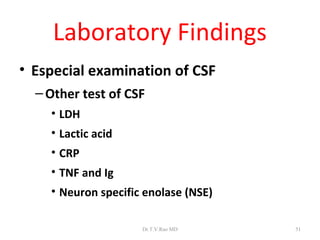
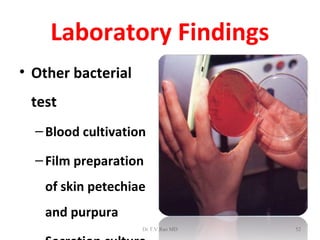
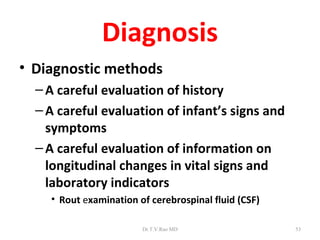
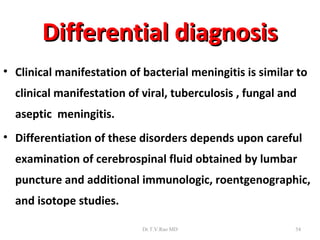
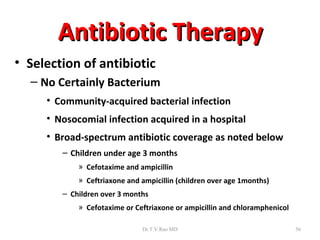
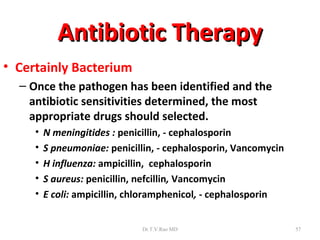
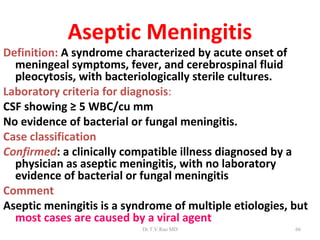
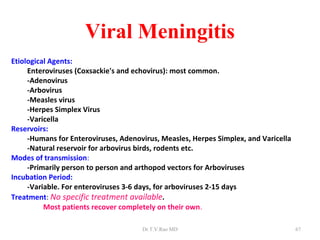
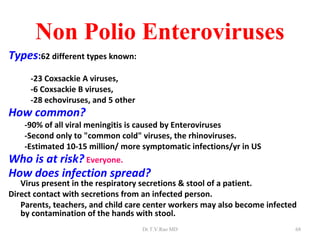
The document discusses bacterial meningitis, providing information on the anatomy of the meninges, causes of meningitis including bacterial, viral and fungal infections. It describes the typical presentation of bacterial meningitis including symptoms like headache, fever and neck stiffness. Complications are outlined such as subdural effusions, ependymitis and hydrocephalus. Causative organisms and their prevalence are summarized for different age groups.