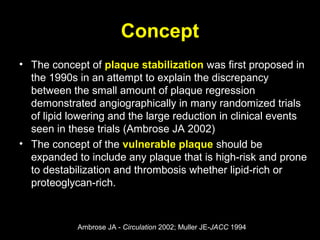
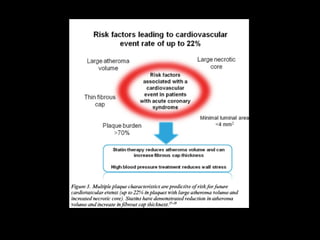
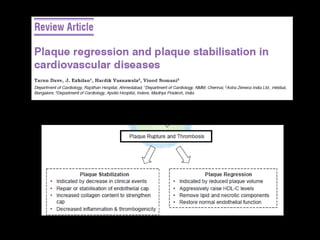
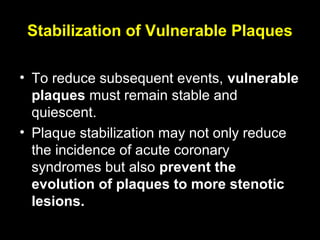
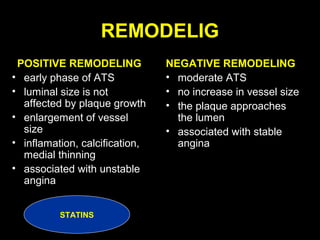
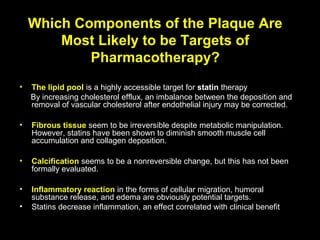
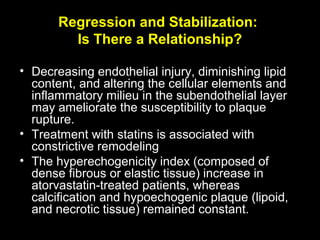
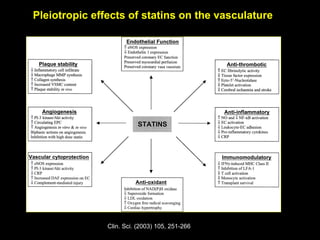
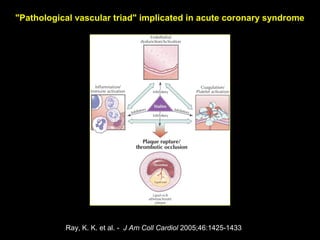
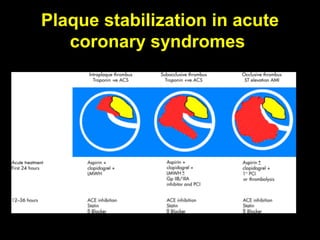
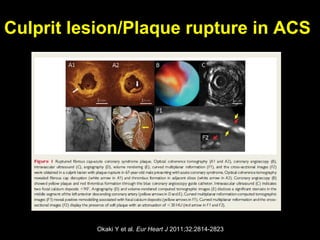
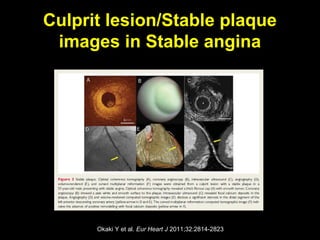
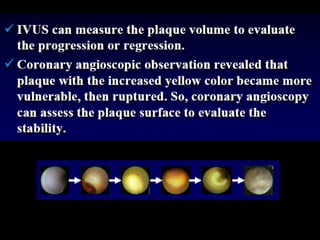
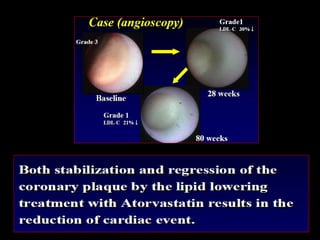
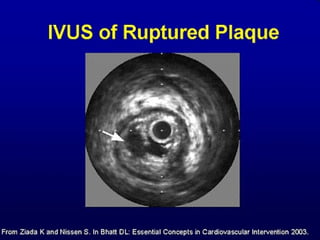
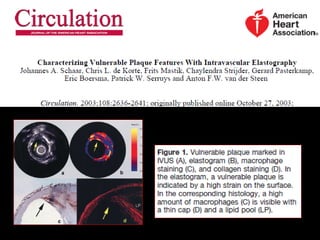
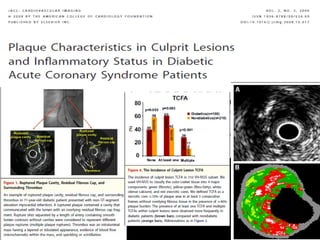
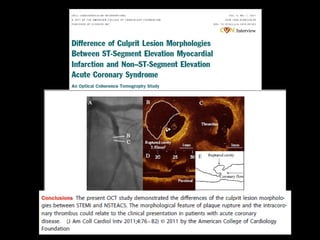
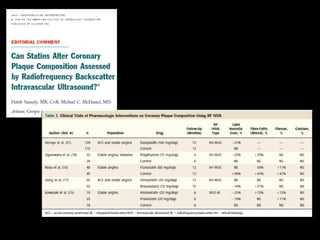
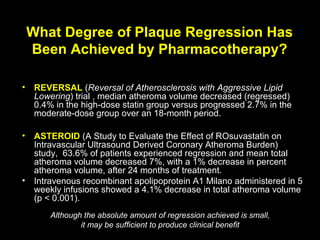
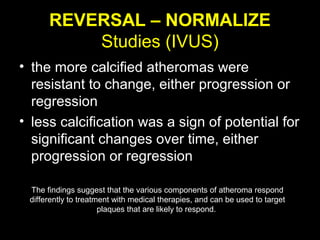
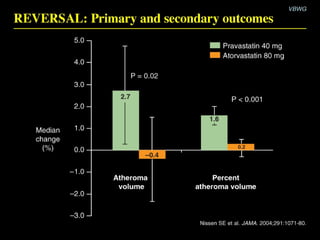
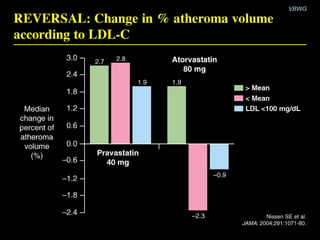
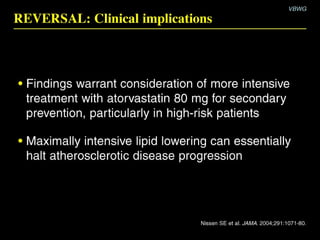
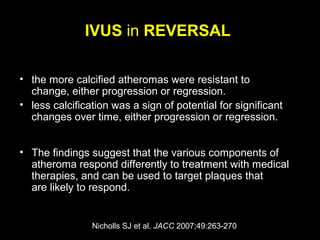
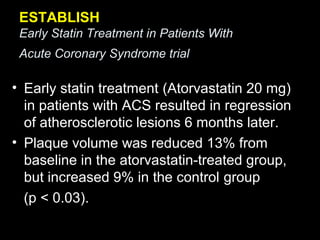
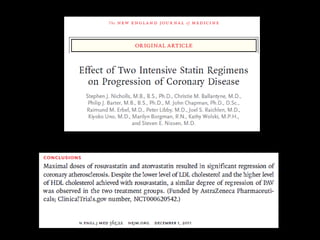
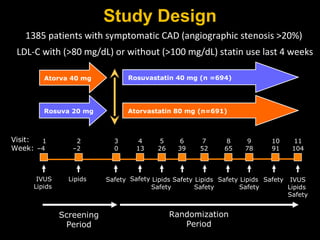
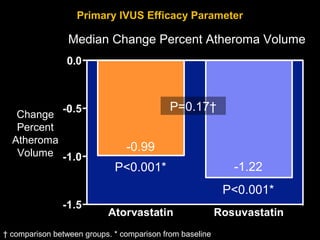
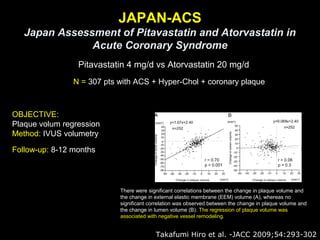
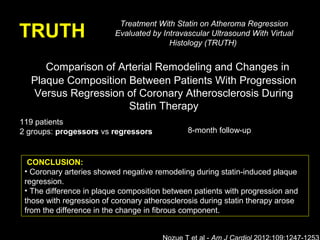
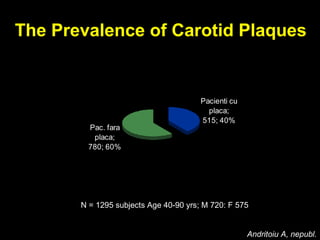
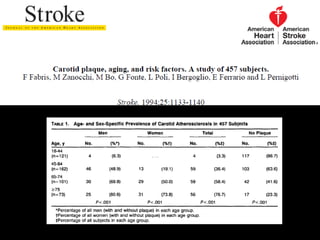
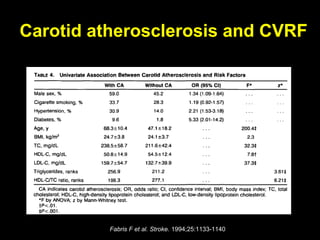
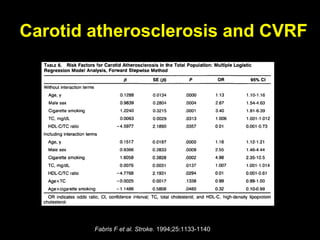
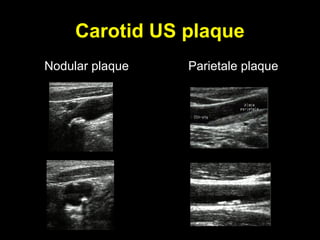
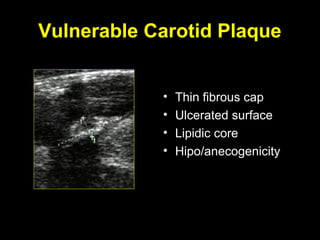
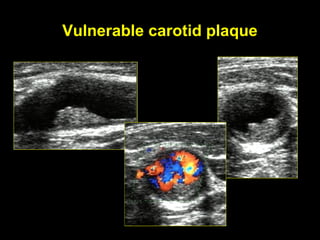
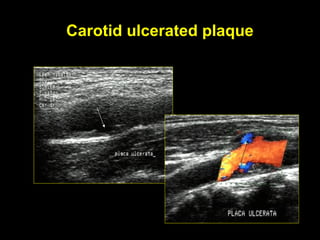
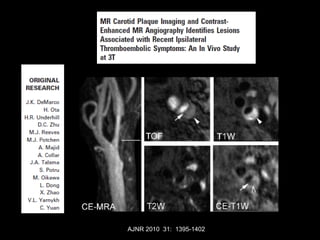
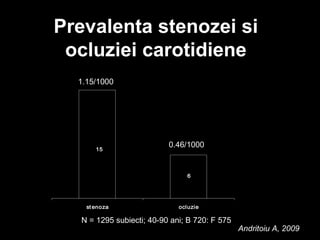
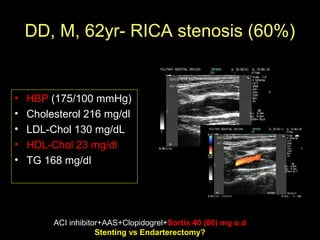
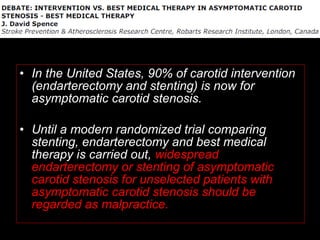
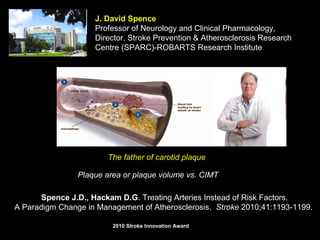
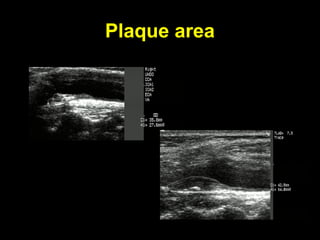
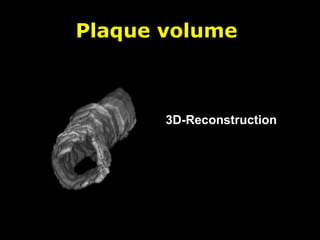
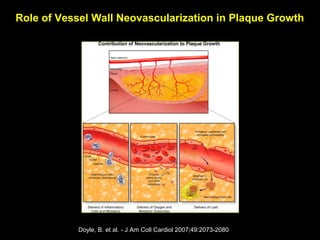
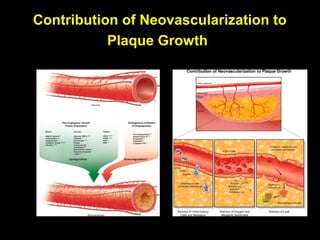
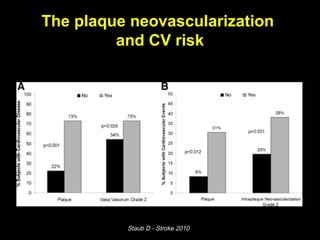
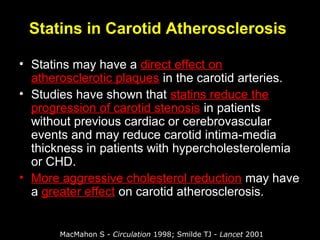
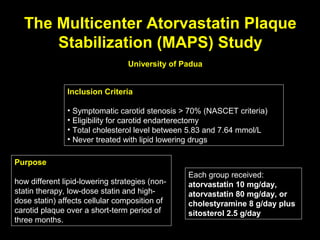
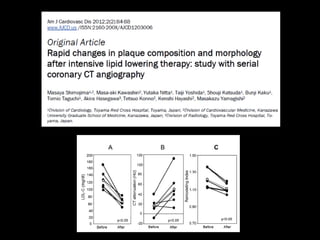
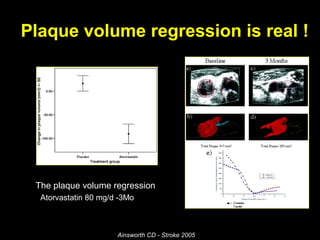
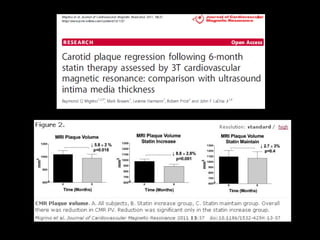
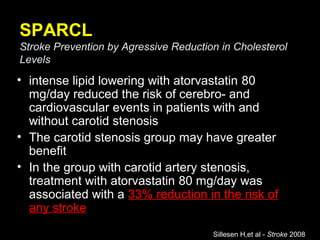
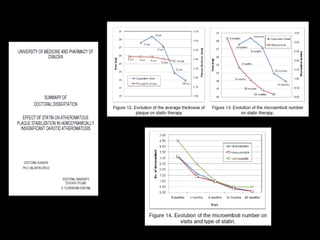
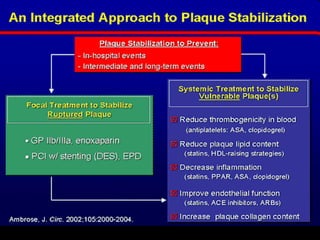
This document discusses plaque stabilization and regression as a new therapeutic target for treating atherosclerosis. It provides background on the concepts of plaque stabilization and vulnerable plaques. Statins, particularly high-dose statin regimens, may promote plaque stabilization and regression through several mechanisms, including reducing inflammation and lipid content within plaques. Studies using techniques like intravascular ultrasound and carotid ultrasound have shown that high-intensity statin therapy can lead to regression in plaque volume and composition changes associated with stabilization. Aggressive lipid lowering may help reduce cardiovascular events, especially in patients with carotid stenosis.