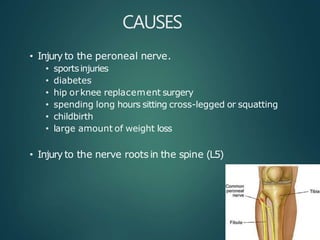
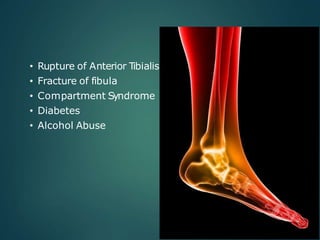
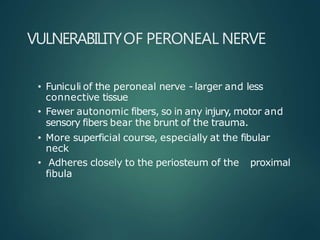
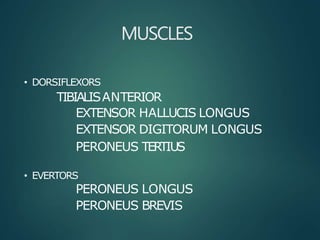
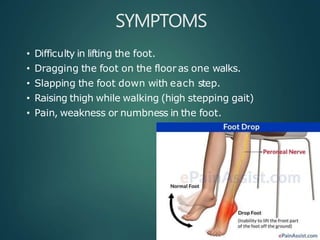
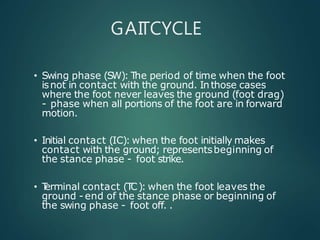
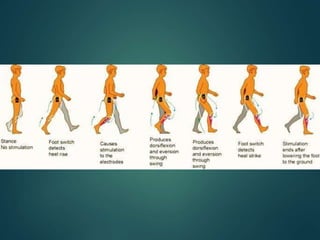
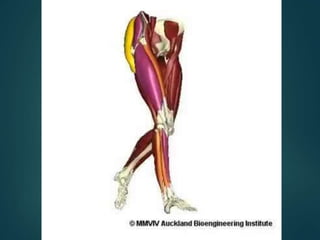
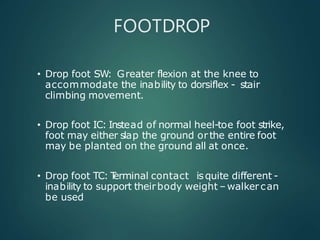
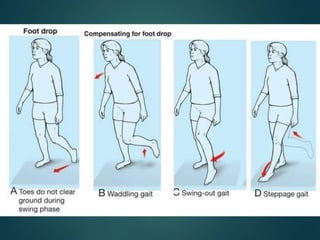
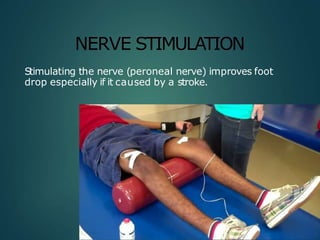
Foot drop is a condition characterized by the inability to lift the front of the foot. It can be caused by injury or disease affecting the peroneal nerve or muscles in the lower leg. Symptoms include difficulty lifting the foot, dragging the toes, and slapping the foot down when walking. Treatment depends on the underlying cause but may include bracing, physical therapy, nerve stimulation, or tendon transfer surgery. The goal is to strengthen muscles and restore function to allow normal walking.