Here are the key points from the question:
- 14-year-old girl presented with 3 weeks of high grade fever, progressive breathlessness, swelling of feet and abdomen
- No associated symptoms like chills, rigors, dysuria, coryza, jaundice or alteration in bowel habits
- Had a generalized seizure today
- Clinically pale, oral ulcers, arthritis of both knees, left sided pleural effusion, distant heart sounds, liver palpable 4cm below costal margin, free fluid
My diagnosis would be Rheumatic fever based on the following:
- History of preceding sore throat
- Fever for 3 weeks
- Arthritis of both knees
- Carditis
















































































![74 OSCE in Pediatrics
A 16:
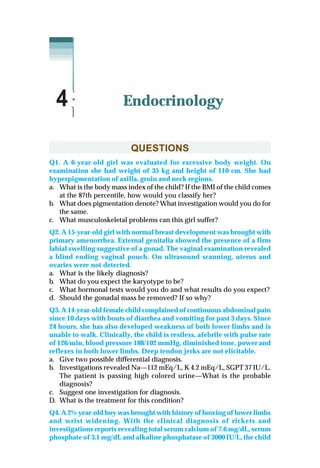
a. Secretory diarrhea Cholera
b. Osmotic diarrhea Laxative abuse
c. Increased motility Irritable bowel disease
d. Altered mucosal surface area Celiac disease
e. Invasiveness Amebiasis
A 17:
a. • Stool frequency > 10/day after 48 hrs of starting particular diet.
• Return of signs of dehydration anytime after starting diet.
• Failure to establish weight gain by 7th day.
b. • High purge rate ( >5 ml/kg/hr).
• Persistent vomiting >3 vomiting/hr
• Ileus or abdominal distension.
• Incorrect preparation.
• Glucose malabsorption.
A 18:
a. Indications:
– Stool frequency >10 watery stool/day even after 48 hrs of starting
diet.
– Return of the signs of dehydration any time after staring diet.
– Failure to establish weight, gain by 7th day of dietary management.
b. Types of diet:
– Diet A (reduced lactose).
– Diet B (lactose free).
– Diet C (Monosaccharide based diet).
A 19:
a. Chronic diarrhea (secondary lactose intolerance—Osmotic diarrhea).
b. Osmotic gap: 290 – (2 × Stool Na+
+ K+
) = 290 – [2 × (42 + 3.8)] = 198.4
If Gap >100 its osmotic diarrhoea.
c. Remove the osmotic load from the diet and stop feeding for 24 hrs and
then restart with lactose free diet.
A 20:
a. Celiac crises.
b. Systemic steroids.
c. IgA deficiency, Down’s syndrome, Turner’s syndrome, William
syndrome, thyroiditis.
A 21:
a. F75: Dried skim milk 25 g, sugar 70 g, cereal flour 35 g, vegetable oil
27 g, mineral mix 20 ml,vitamin mix 140 mg, water to make 1000 ml.
Calories 75 kcal, protein 0.9 g.
F 100: Dried skim milk 80 g, sugar 50 g, vegetable oil 60 g, mineral
mix 20 ml, vitamin mix 140 mg, water to make 1000 ml. Calories
100 kcal, protein 2.9 g.
b. Day1-7 for initial treatment; week 2-6 for rehabilitation and week 7 to
26 for follow-up.](https://image.slidesharecdn.com/osceinpediatrics-151202232408-lva1-app6891/85/Osce-in-pediatrics-88-320.jpg)













![88 OSCE in Pediatrics
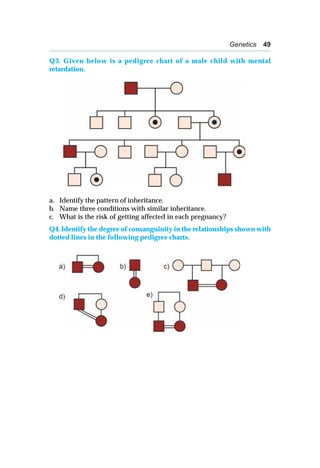
A 8:
a. ANA, ds DNA, HIV, serum immunoglobulin.
b. • Platelet transfusion.
• Methyl prednisolone—500 mg/m2 IV /day × 3 days.
• IV IG 0.8-1.0 gm/kg.
• Anti-D therapy for Rh positive patients.
• Emergency splenectomy.
c. Indications for bone marrow aspirations include an abnormal WBC
count or differential or unexplained anemia as well as finding
suggestive of bone marrow disease on history and physical examination.
d. When thrombocytopenia persists for more than 6 months.
e. Valproic acid, phenytoin, sulfonamides, cotrimoxazole.
A 9:
a. Hemophilia A or B.
b. PTT increased.
c. X- linked recessive.
d. Moderate:
• Severe: <1% activity of specific clotting factor and spontaneous
bleeding
• Moderate: 1-5%; require mild trauma to induce bleeding
• Mild: >5%; require significant trauma to cause bleeding.
A 10:
a. Sickle cell beta + thalassemia.
b. Beta + thalassemia.
c. Streptococcus pneumoniae, H. inf type B.
A 11:
a. Kawasaki disease 1. Thrombocytosis
b. Alpha thalassemia major 2. Hydrops fetalis
c. Beta thalassemia major 3. Increased fetal Hb
d. Sickle cell disease 4. Hyposplenism in a 6-year-old
e. G6PD deficiency 5. Oxidant induced red cell damage
f. Hereditary spherocytosis 6. Splenomegaly in a 6-year-old
A 12:
a. Acute lymphoblastic leukemia.
b. 2-6 years; more common in boys than girls at all ages.
c. ALL is diagnosed by a bone marrow evaluation that demonstrates
>25% of the bone marrow cells as a homogeneous population of
lymphoblasts.
d. • Age <1 year or >10 years at diagnosis
• Leukocyte count of >100,000/mm3
at diagnosis
• Slow response to initial therapy
• Chromosomal abnormalities, including hypodiploidy, the
philadelphia chromosome, and MLL gene rearrangements and
translocations [t(1:19) or t(4;11)]
• CNS involvement at presentation.](https://image.slidesharecdn.com/osceinpediatrics-151202232408-lva1-app6891/85/Osce-in-pediatrics-102-320.jpg)




















































![148 OSCE in Pediatrics
A 15:
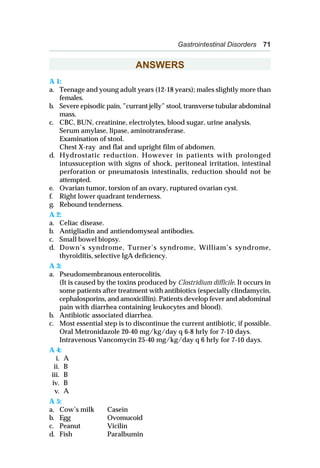
a. Peak flow meter.
b. 200 liters/min.
Formula for approximate normal PEFR for a given height:
PEFR ( L/min) = [ ht. ( in cm) – 80] × 5.
c. Vital capacity and its subdivisions and expiratory (or inspiratory) flow
rate.
A 16:
a. Penicillin binding proteins with altered affinity for penicillin.
b. Hypoxemia (i.e., PaO2 < 80 mm of Hg in room air).
c. Interstitial infiltrates beginning in the perihilar region and spreading
to the periphery. Apices spared until later in the disease.
A 17:
a. Acute epiglottitis.
b. Tripod position—sitting upright and leaning forwards with chin up
and mouth open while bracing on the arms.
c. Direct visualization of large, ‘cherry red’ swollen epiglottis. Ensure
availability of resuscitation or tracheostomy equipments.
d. Lateral neck X-ray shows ‘thumb sign’.
e. Establishing an airway by nasotracheal intubation or less often by
tracheostomy, regardless of the degree of apparent respiratory distress.
A 18:
a. Acute bronchiolitis.
b. RSV is responsible for > 50% cases. Other viruses include para-
influenza, adenovirus, mycoplasma and human meta pneumovirus.
c. Cool humidified oxygen to prevent hypoxemia.
d. Premature babies, CLD, congenital heart disease, immunodeficient
babies.
Administration of pooled hyperimmune RSV IVIG; and Palivizumab,
intramuscular monoclonal antibody to RSV F protein before and during
RSV season in infants < 2 years.
A 19:
a. Cystic fibrosis. The presenting history might at first suggest
bronchiolitis (age, season, clinical presentation but the weight loss is
out of proportion with the short history of reduced feeds). Ongoing
diarrhoea, weight loss and chest signs/symptoms should alert you to
a possible diagnosis of cystic fibrosis.
b. Bronchiectasis, sinusitis, nasal polyps, hemoptysis, pneumothorax, cor
pulmonale, mucoid impaction of bronchi.
c. Delayed puberty, infertility, diabetes mellitus, gynecomastia.
d. Staph aureus, Pseudomonas aeruginosa, Burkholderia cepacia.
e. Quantitative sweat test using pilocarpine electrophoresis (Cl–
< 60 mEq/L) in conjunction with 1 or more of the following: typical
chronic obstructive pulmonary disease, documented exocrine
pancreatic insufficiency or a positive family history.](https://image.slidesharecdn.com/osceinpediatrics-151202232408-lva1-app6891/85/Osce-in-pediatrics-162-320.jpg)