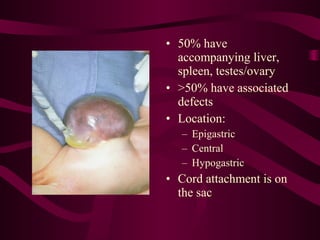
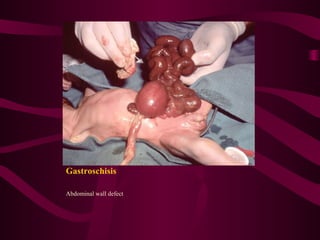
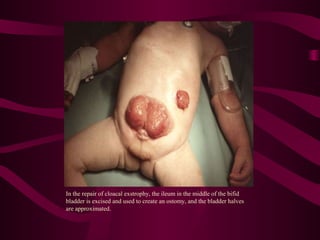
This document discusses various abdominal wall defects in infants. It describes omphalocele, where abdominal organs protrude into a sac through a defect in the abdominal wall near the umbilicus. Gastroschisis is defined as a defect to the right of the umbilicus where intestines directly eviscerate. Incidence, pathophysiology, clinical findings, associated anomalies, and treatment approaches like primary closure or staged closure using a silo are reviewed for each condition. Other rare defects discussed include umbilical hernia, prune belly syndrome, bladder exstrophy, pentalogy of Cantrell, and Beckwith-Wiedemann syndrome. Key differences between omphalocele and gastroschis