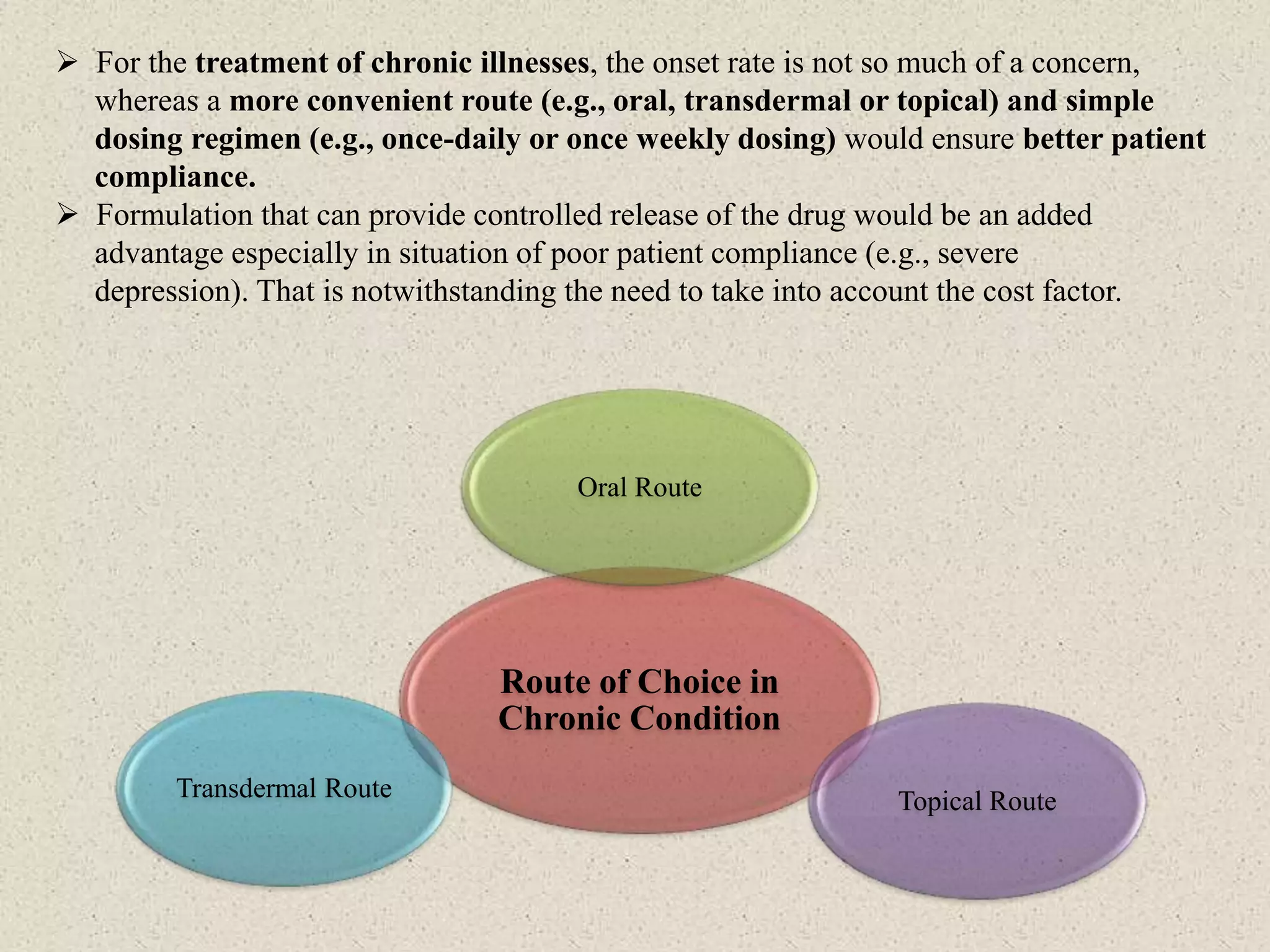
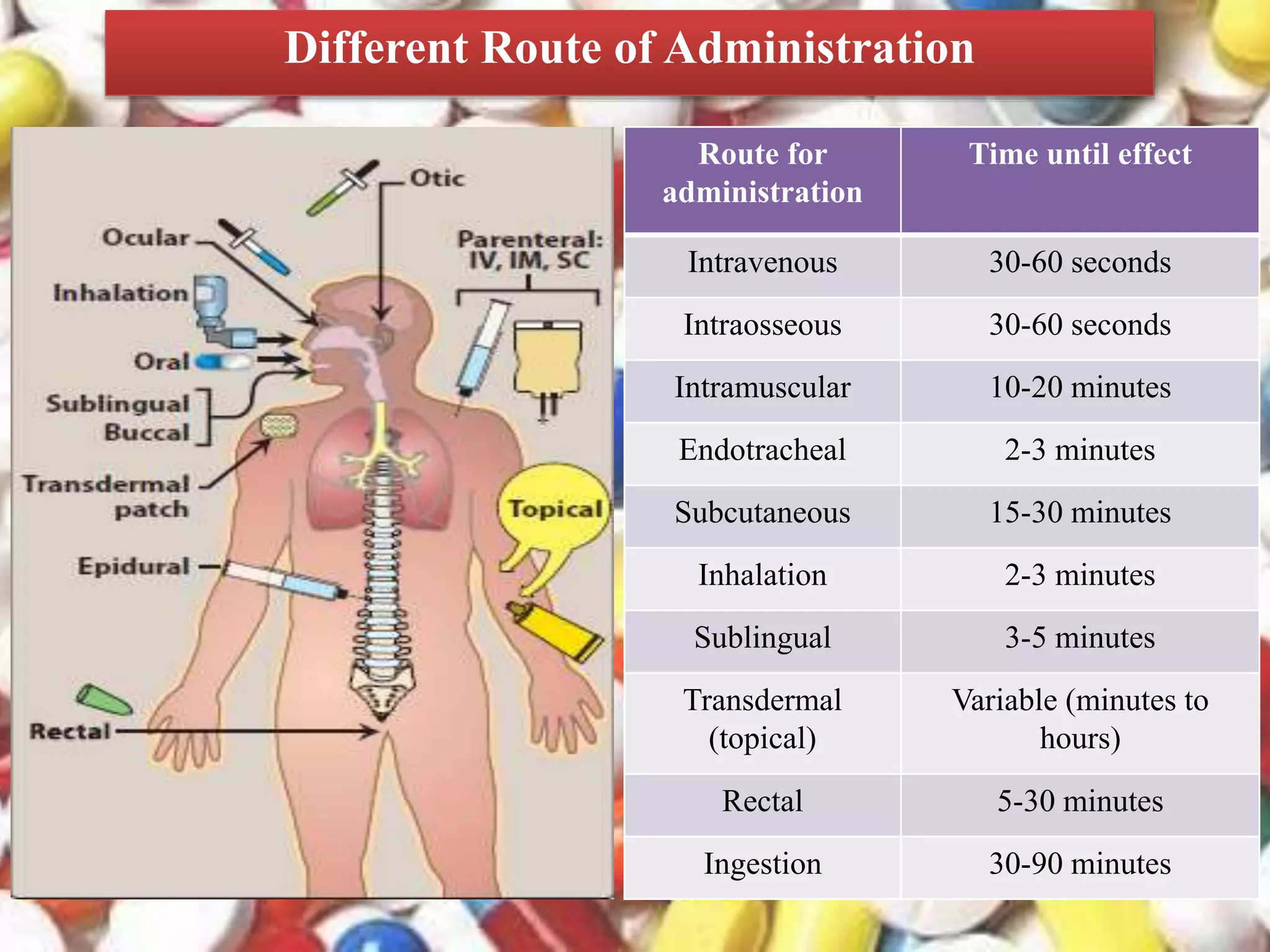
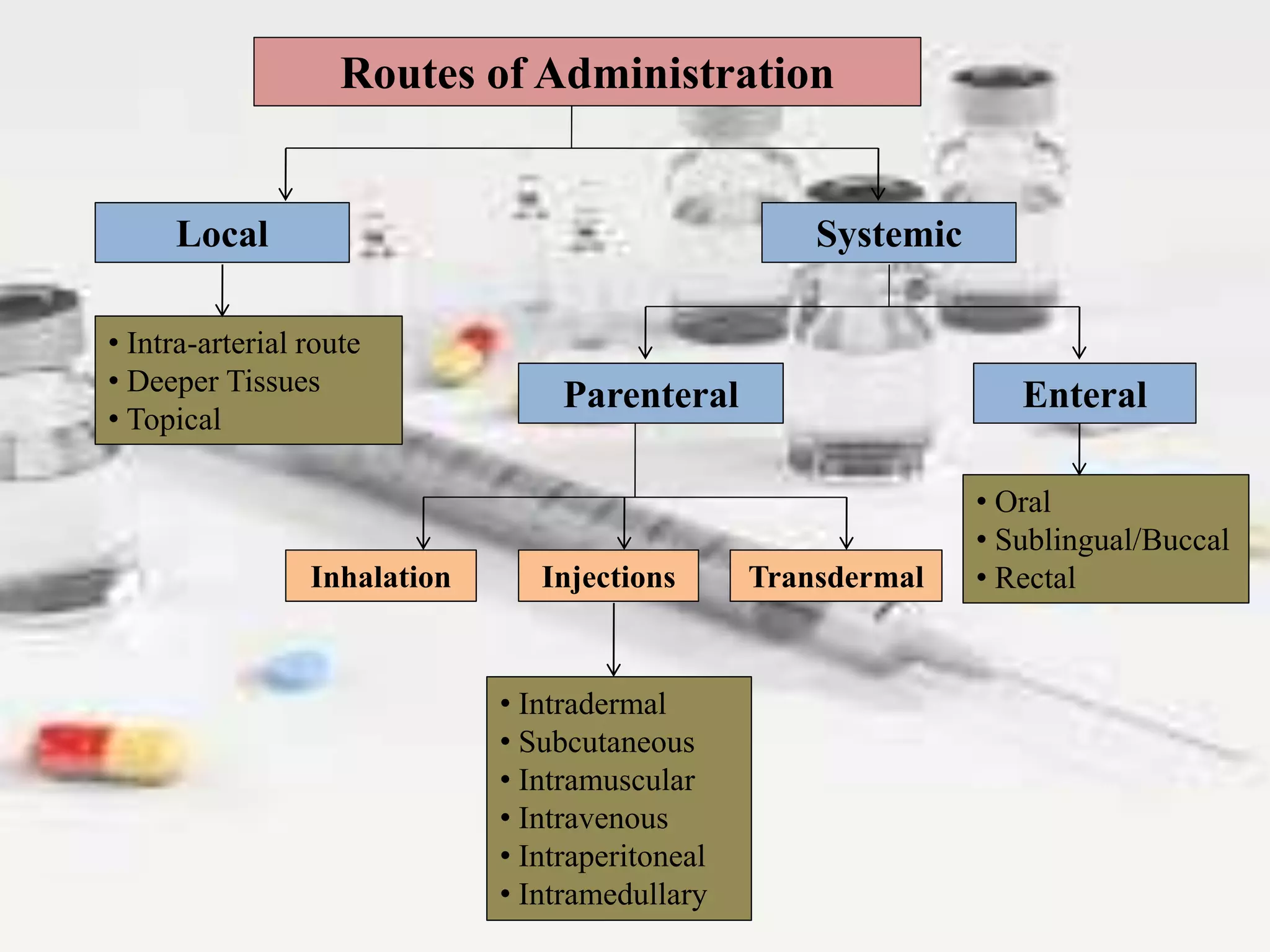
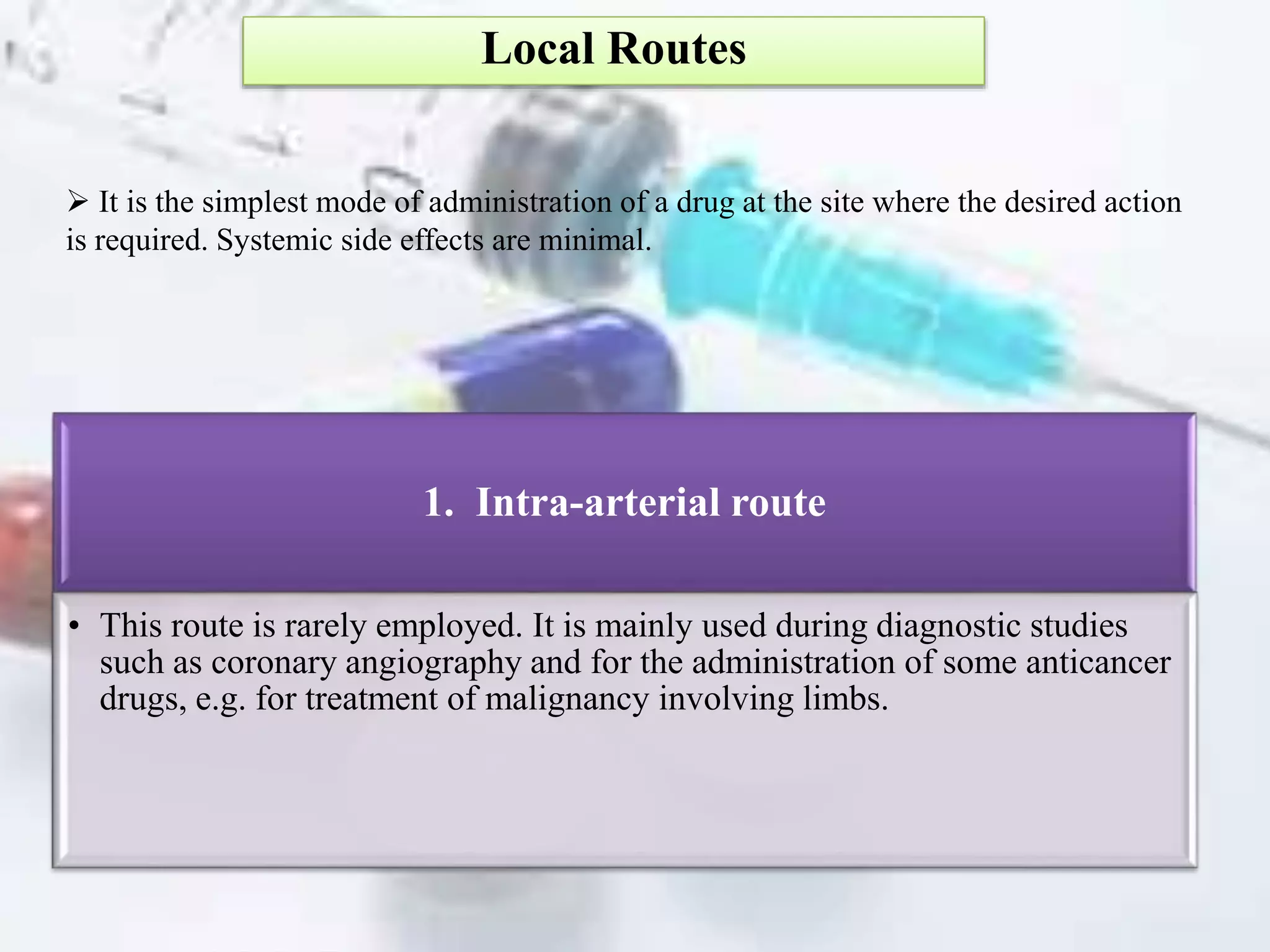
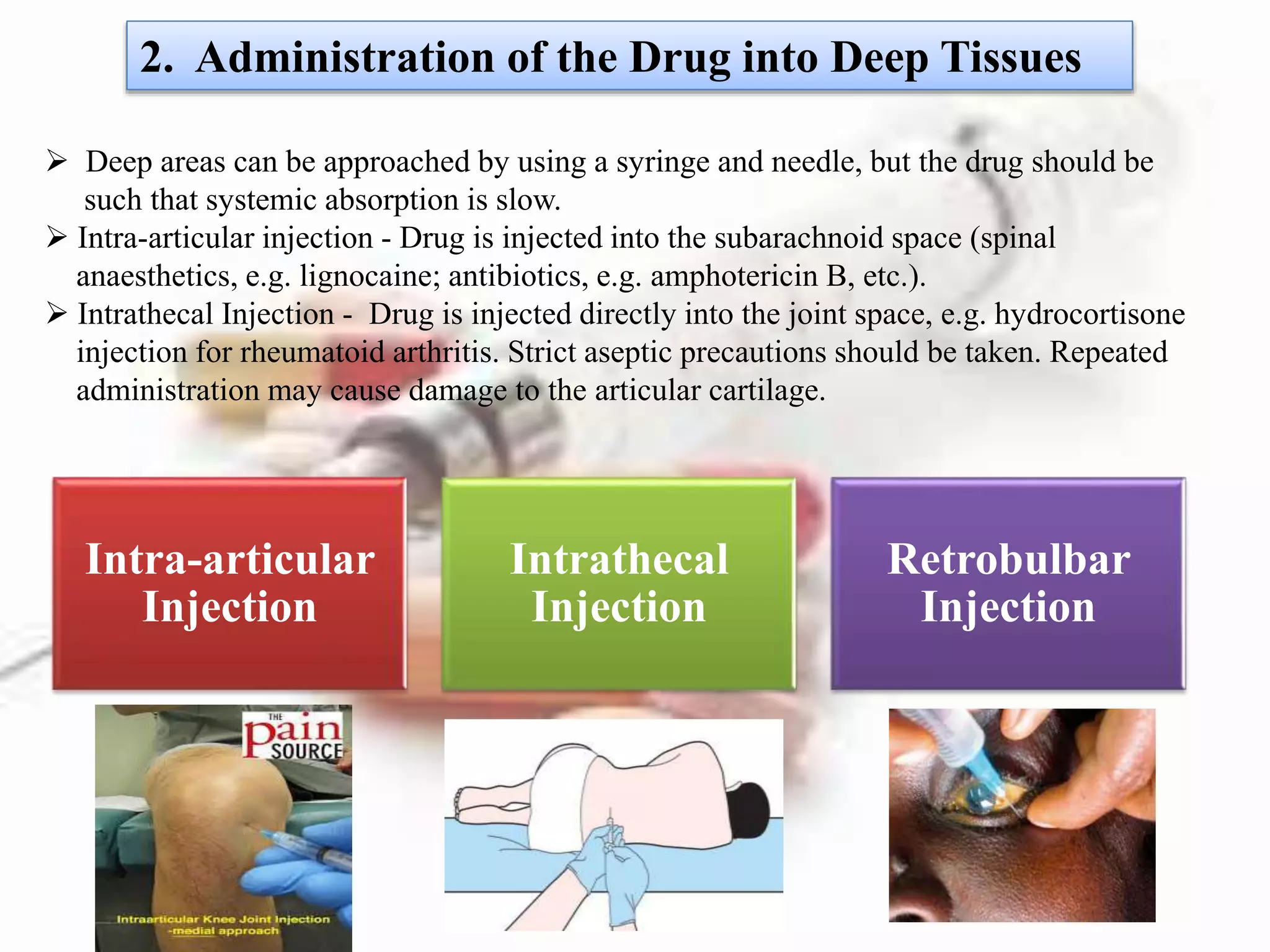
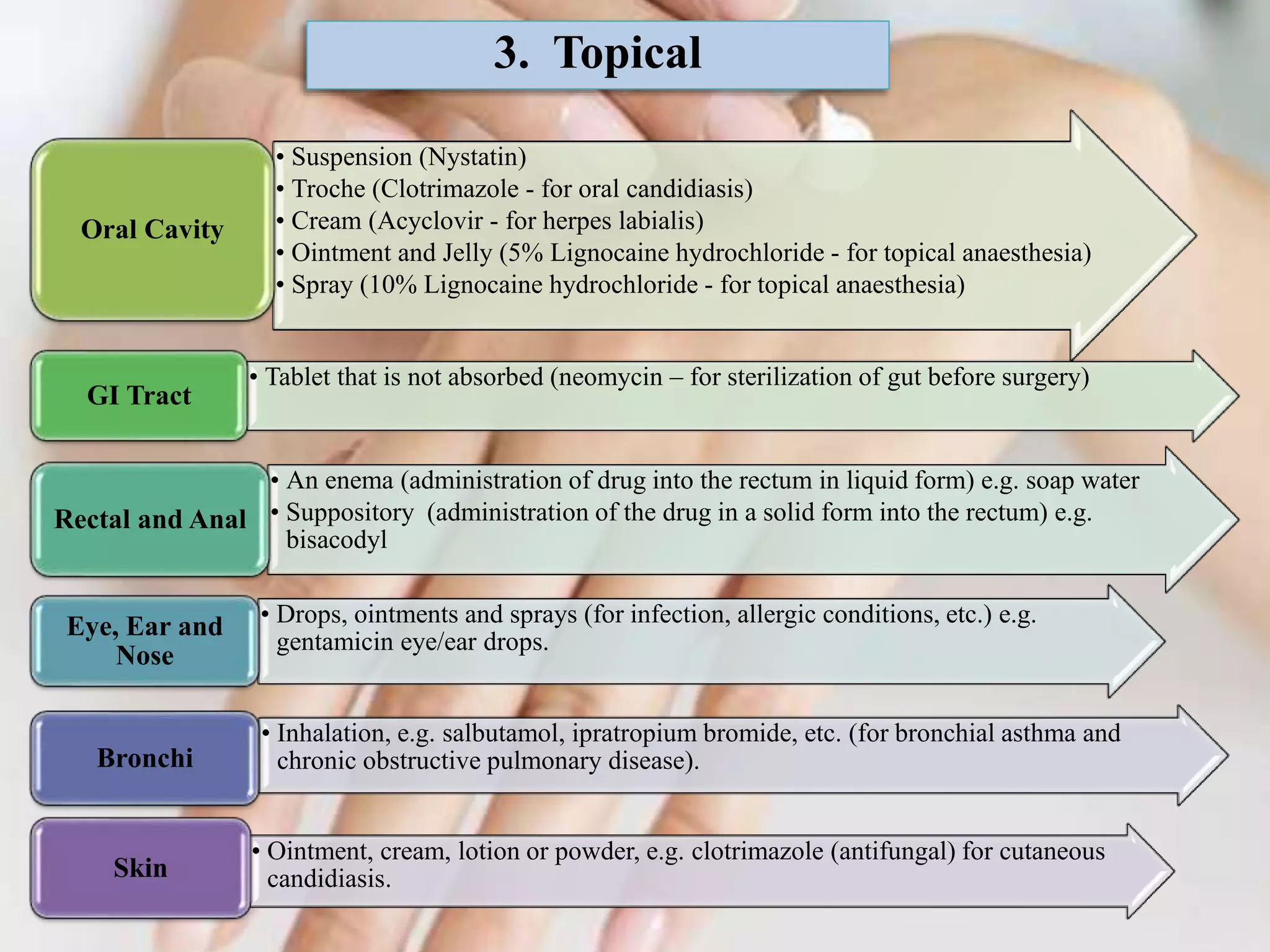
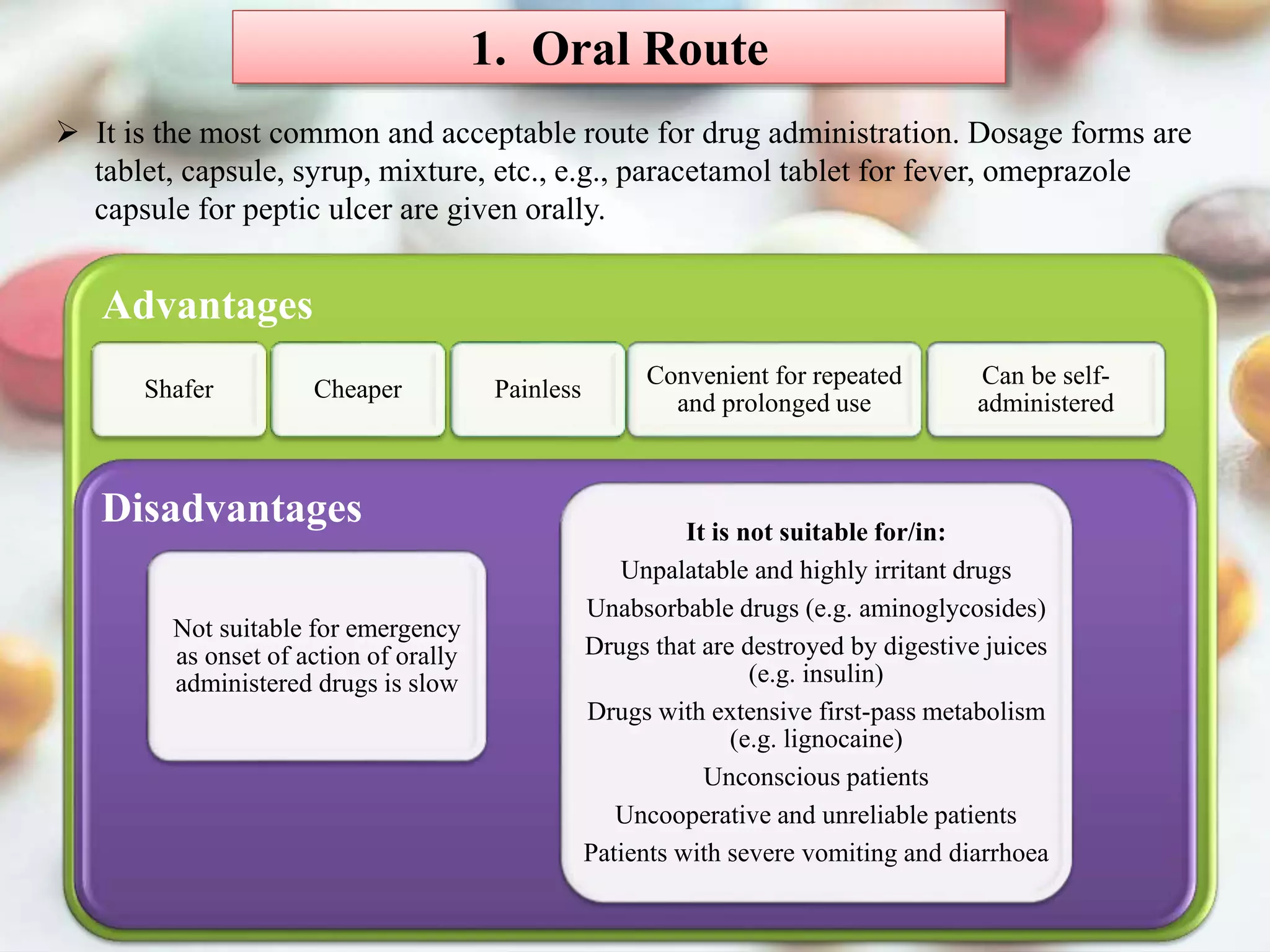
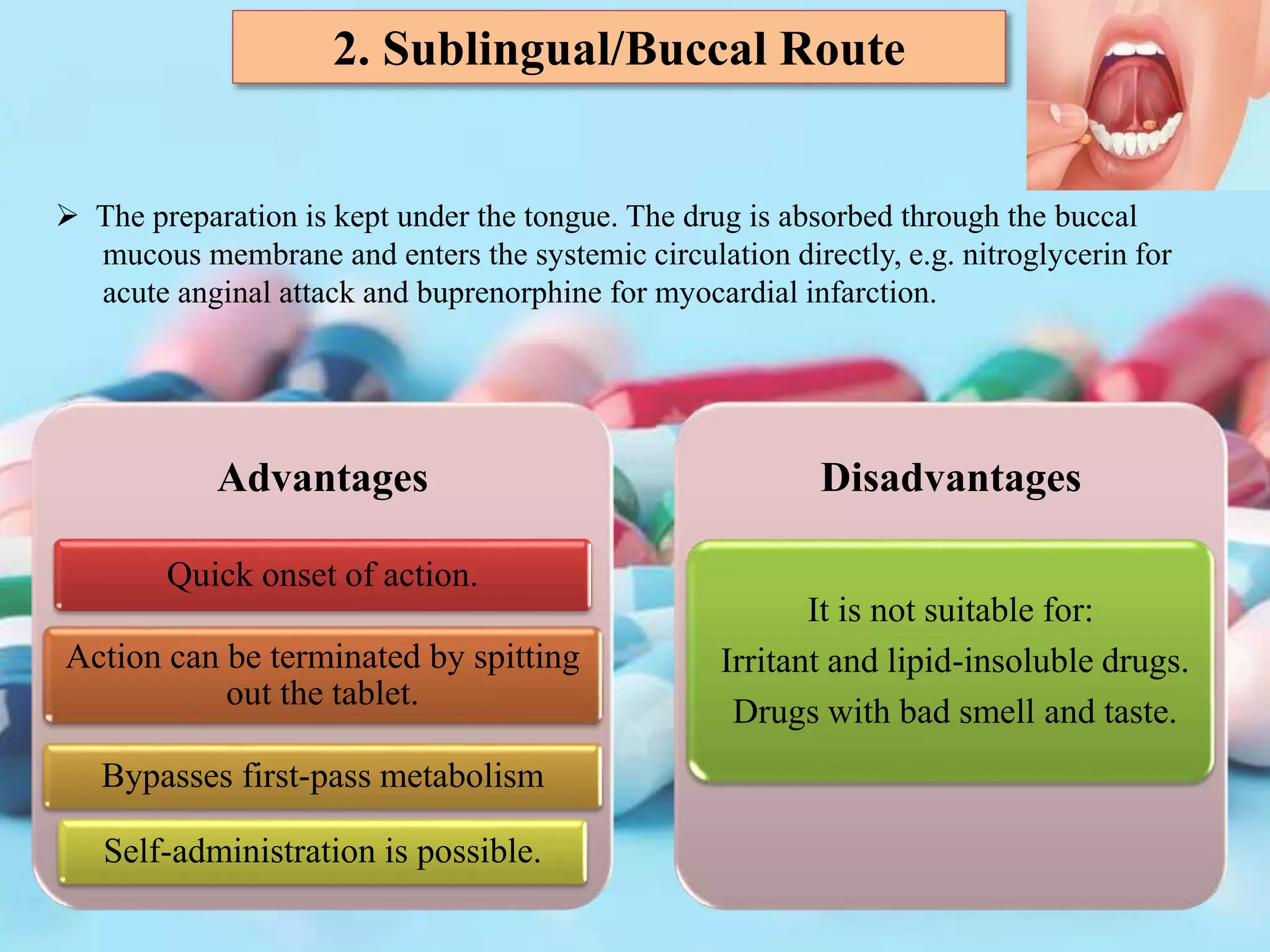
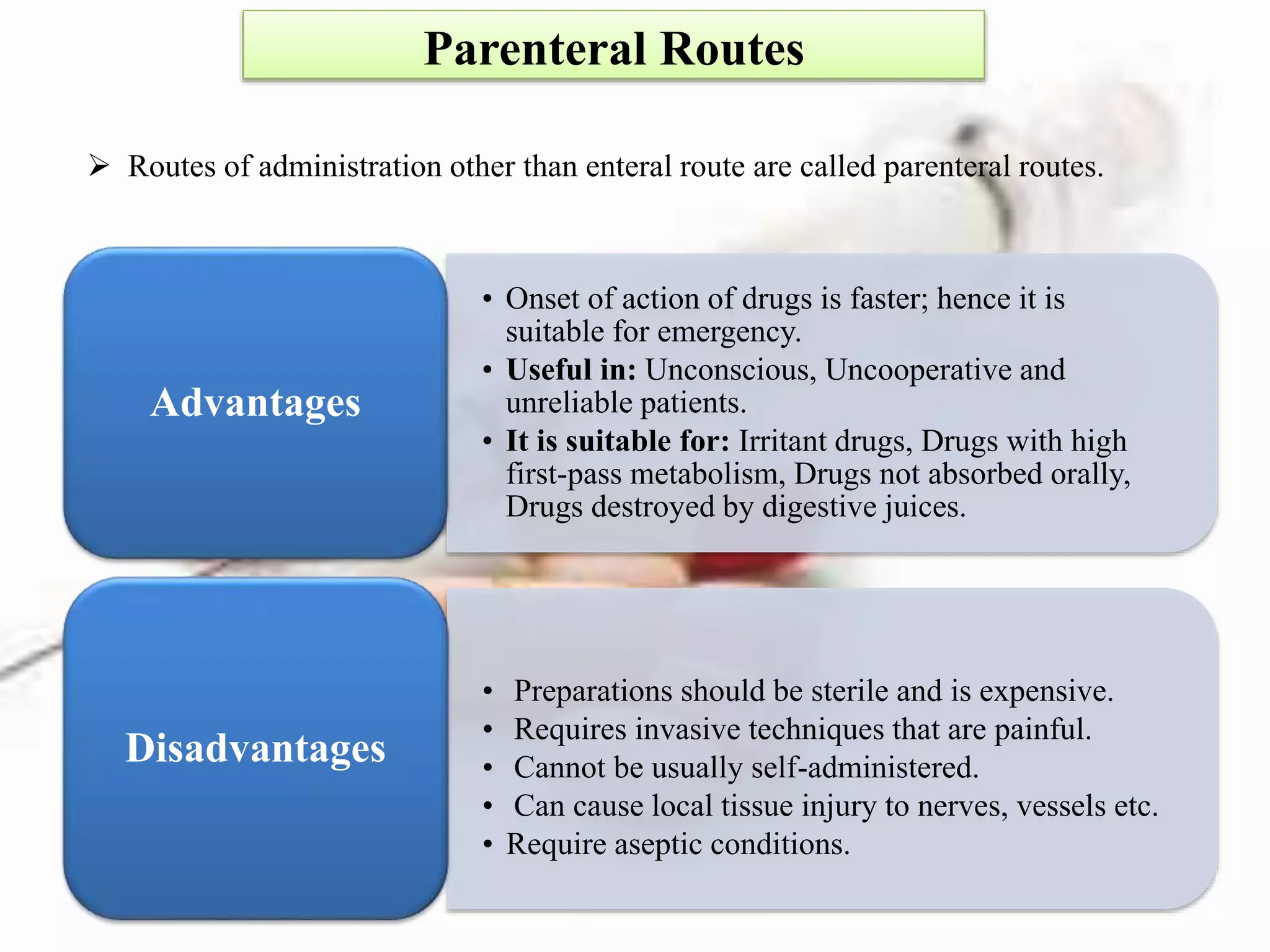
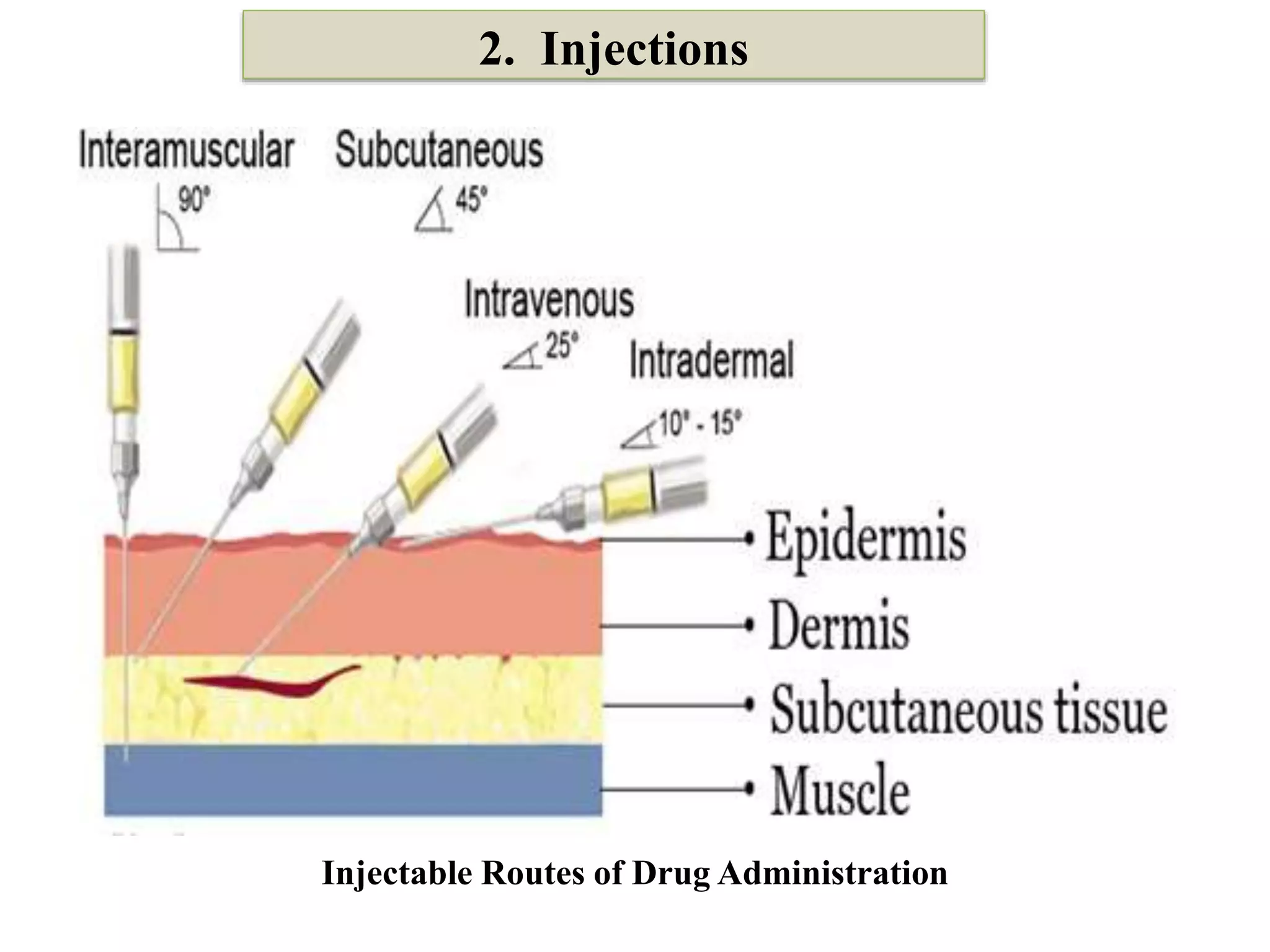
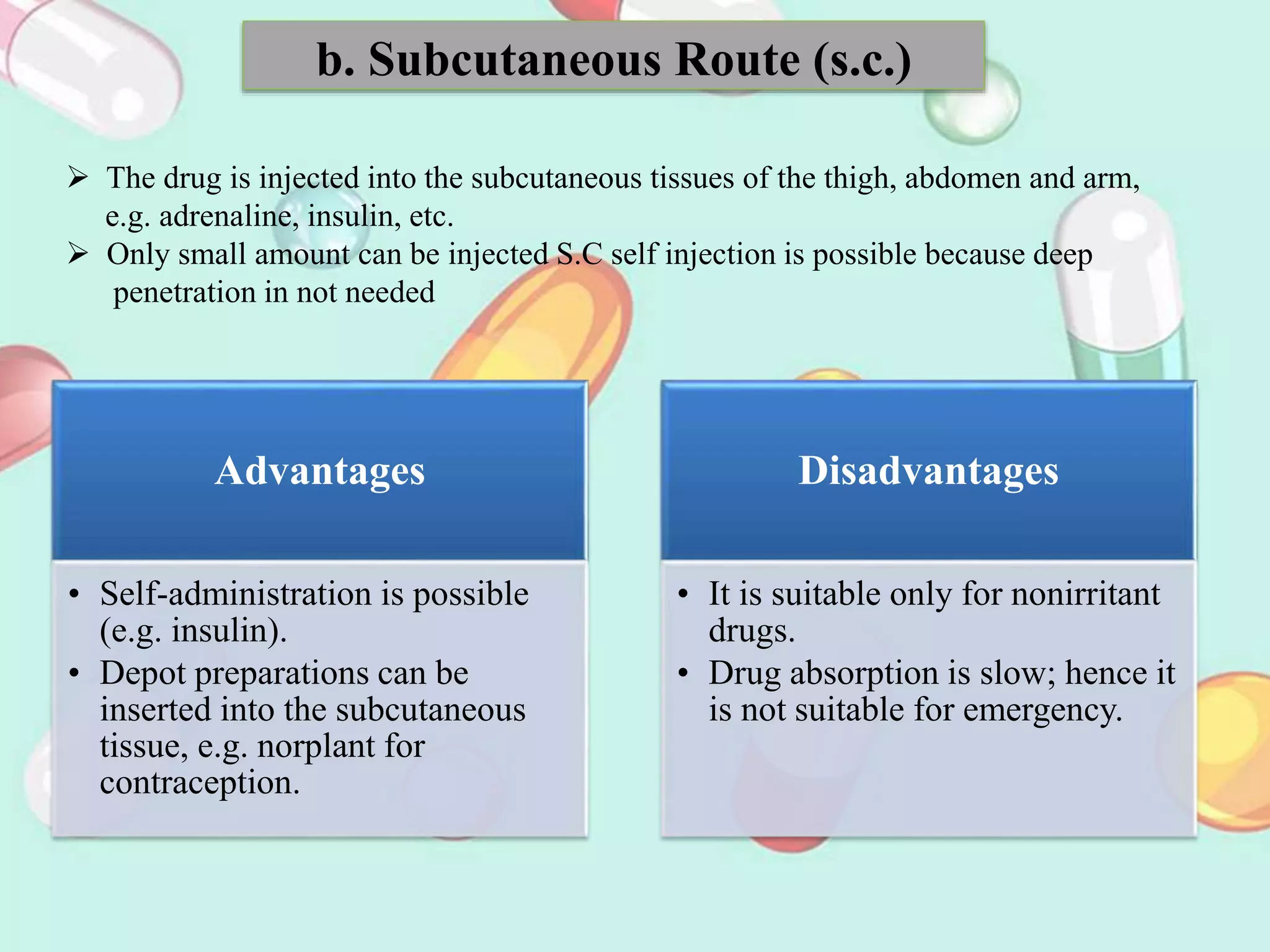
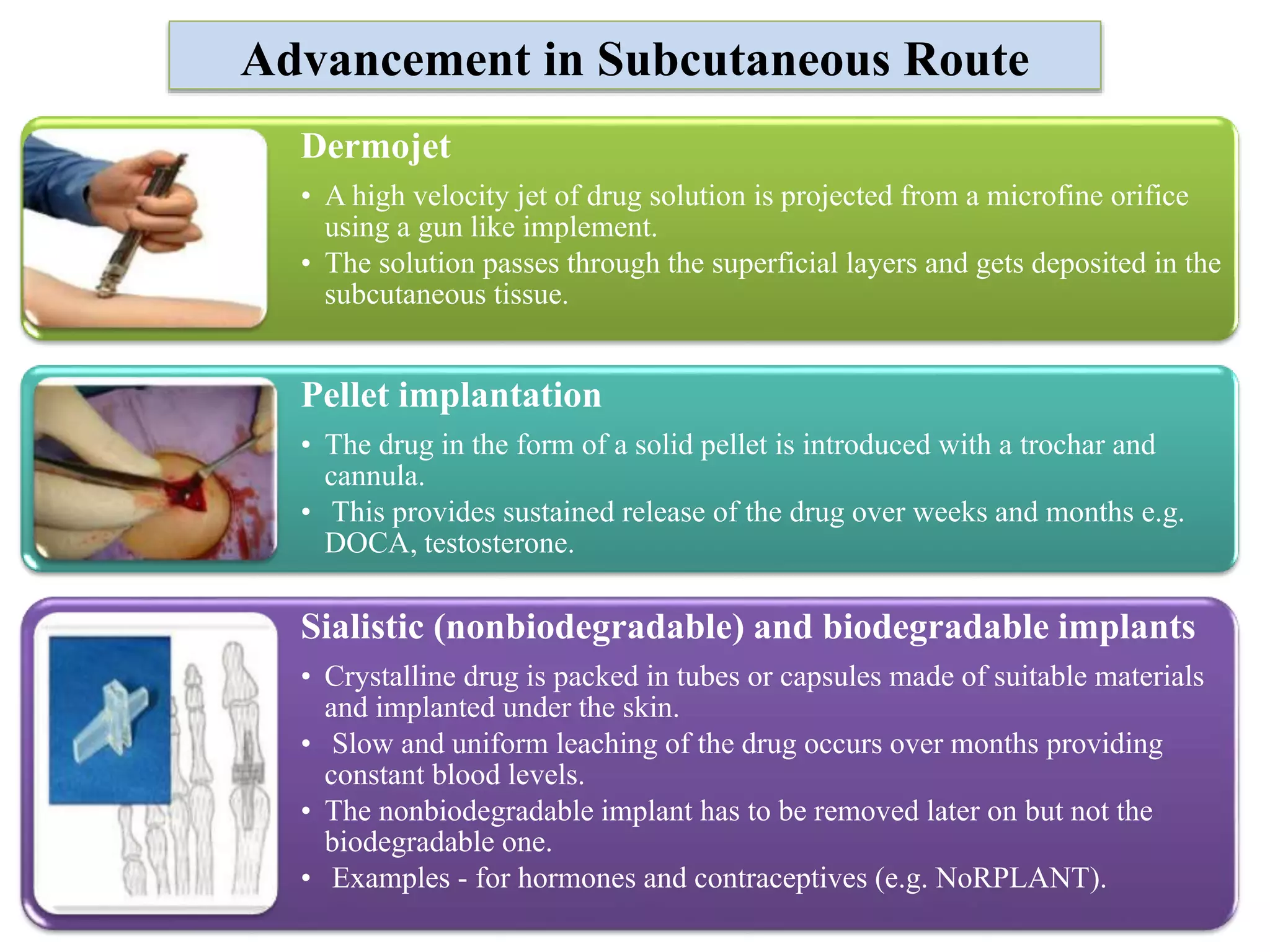
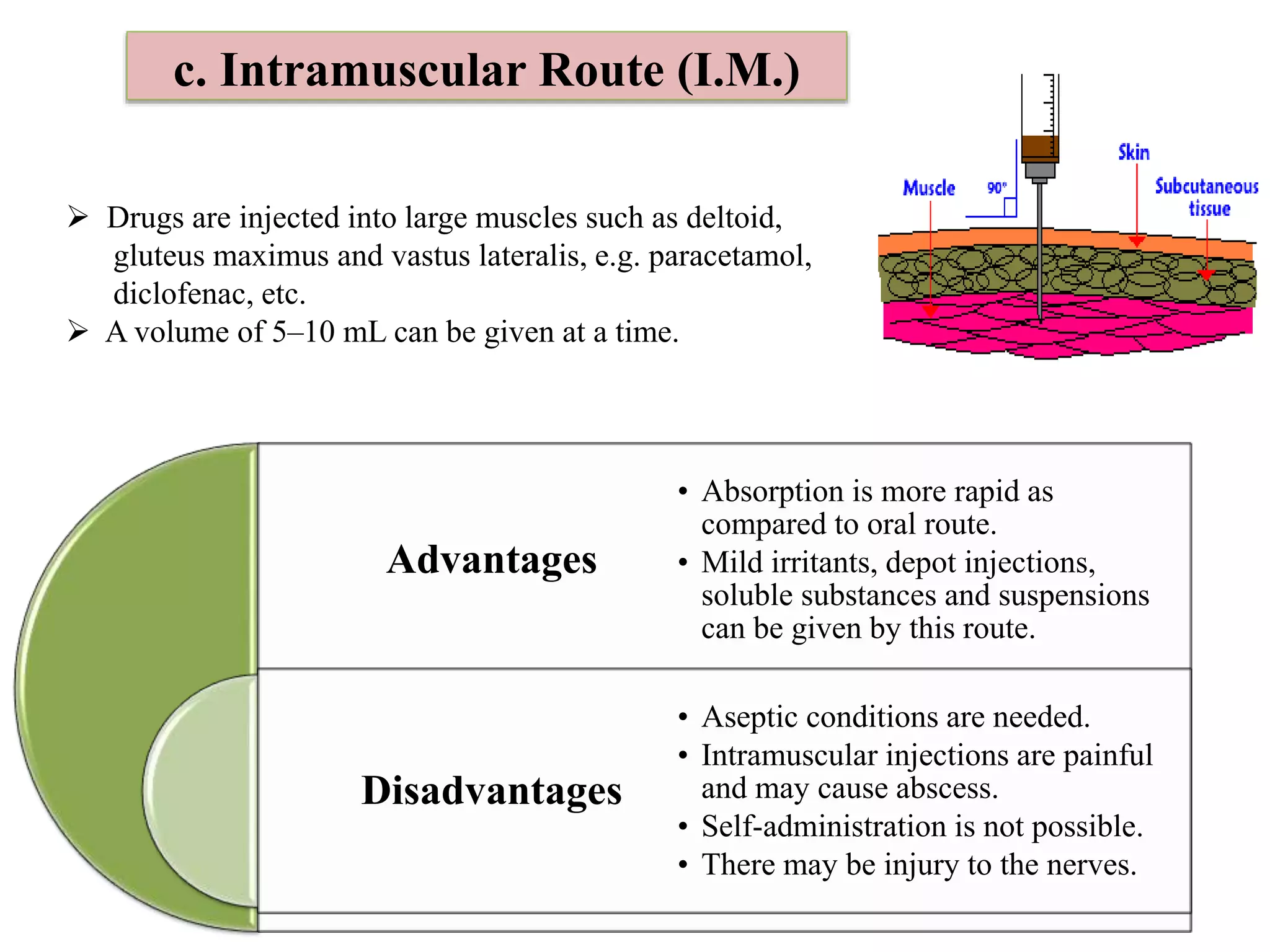
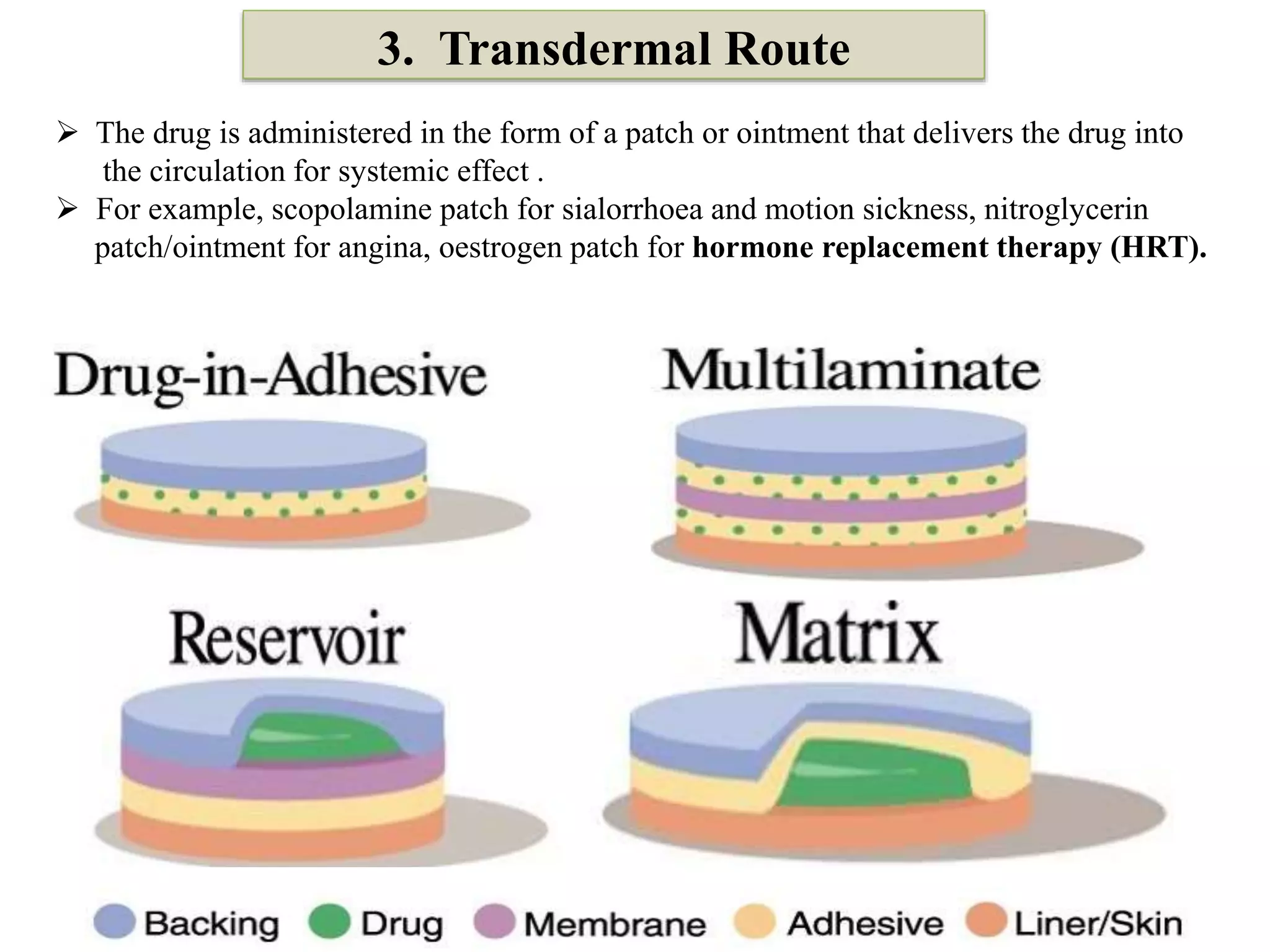
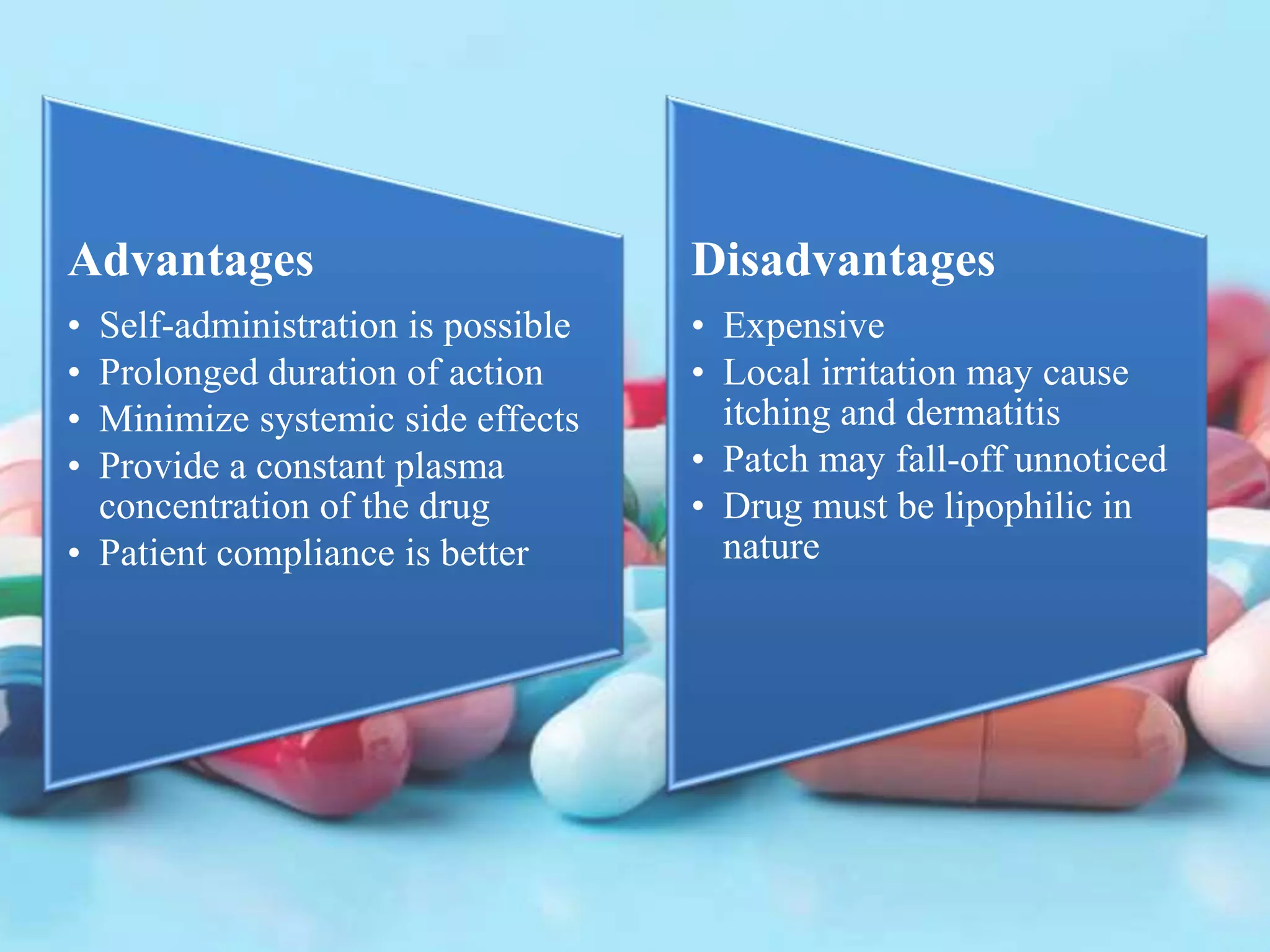
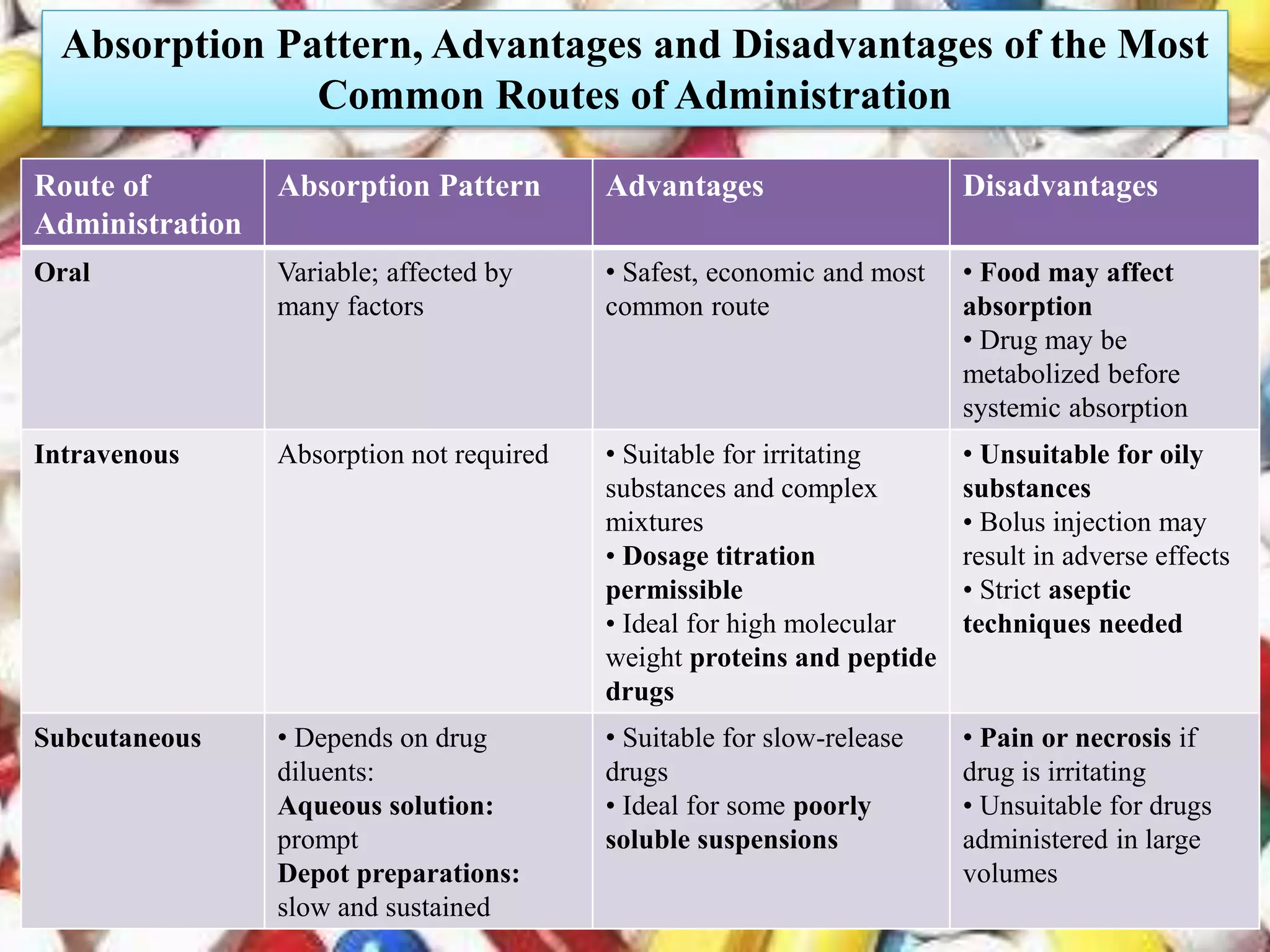
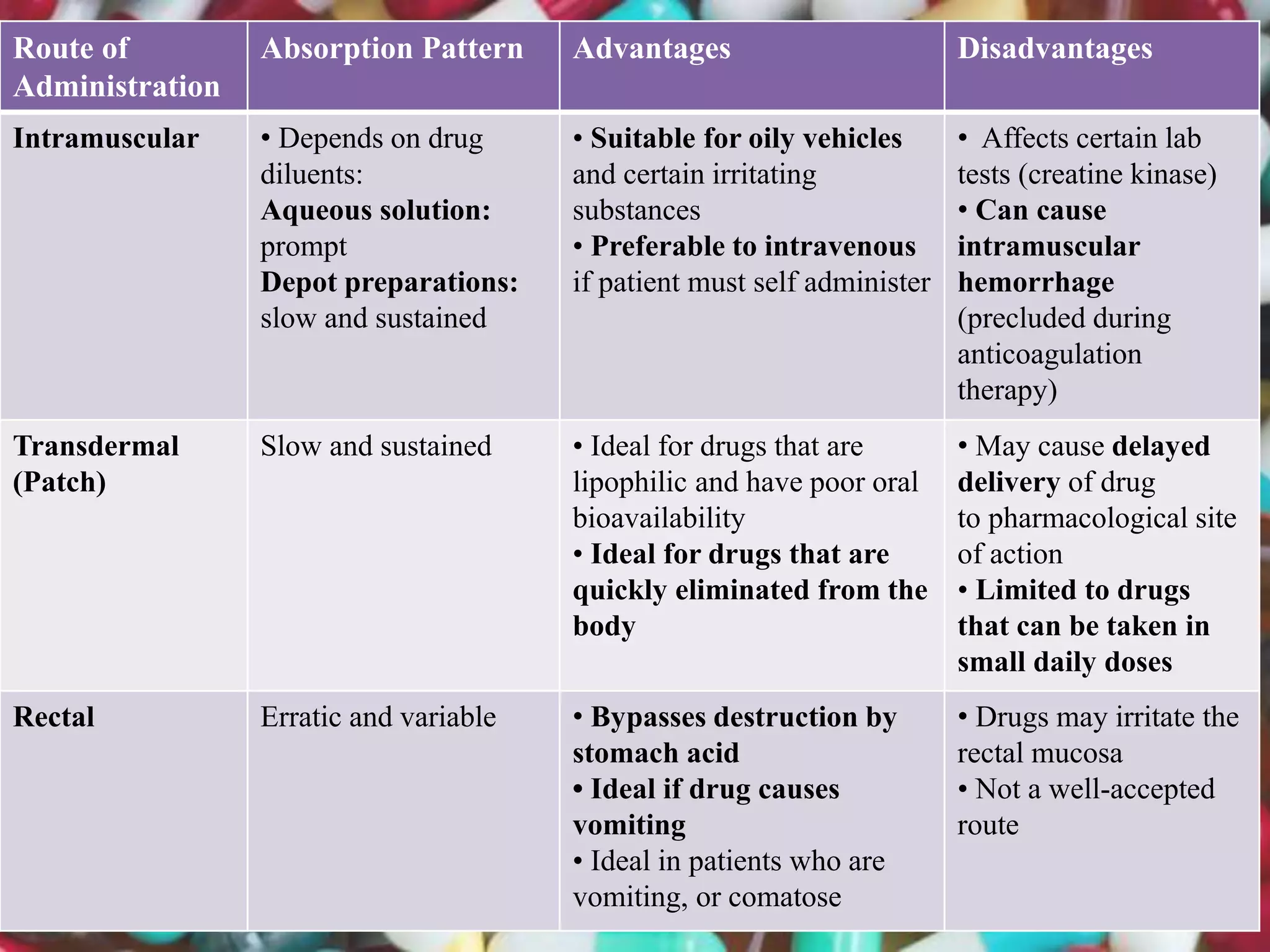
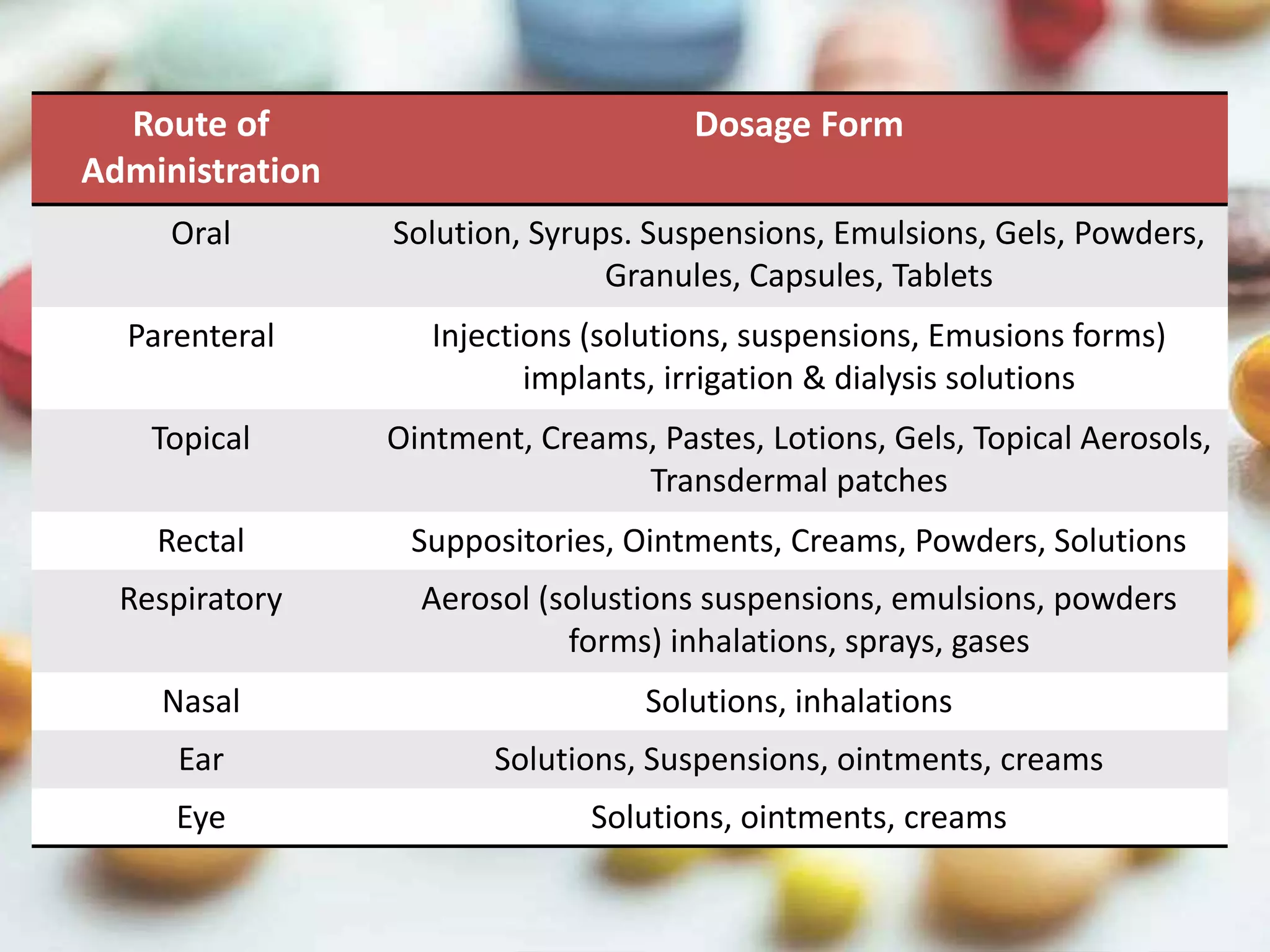
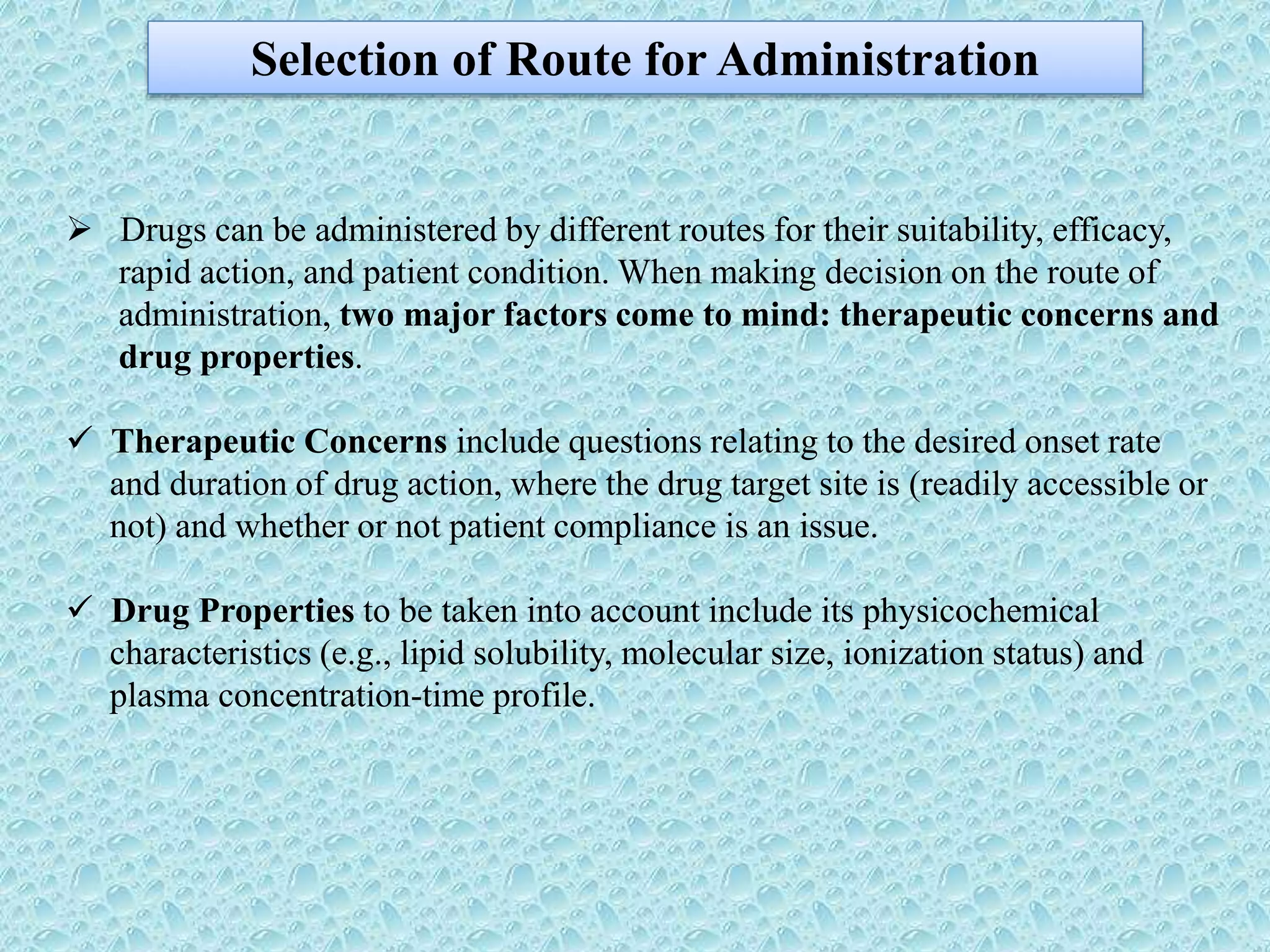
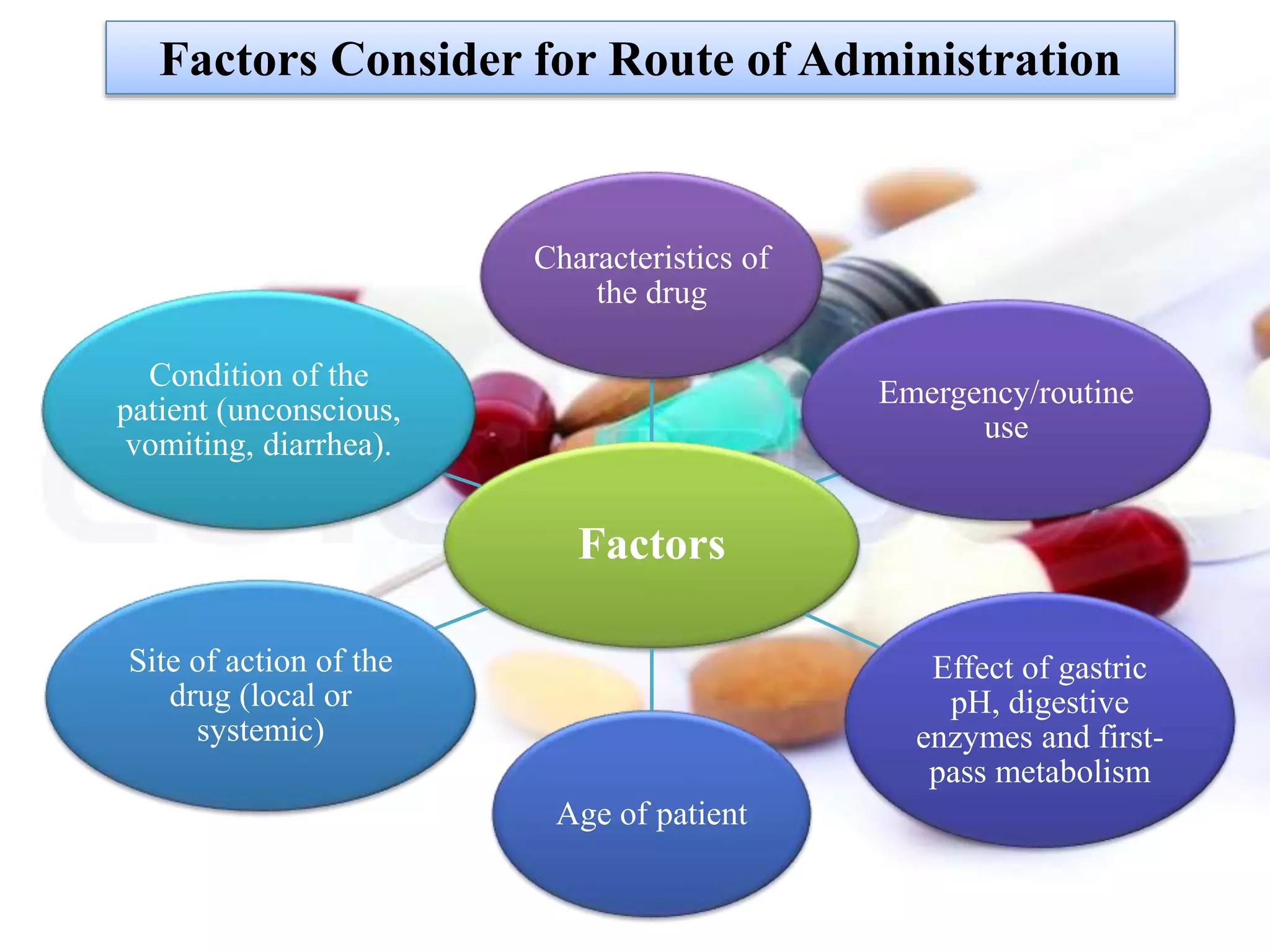
The document outlines various drug administration routes based on therapeutic concerns and drug properties, highlighting how the choice of route can depend on factors like patient condition and drug characteristics. Key routes include parenteral for rapid action in emergencies and oral for convenience in chronic conditions, with detailed discussion on subtypes such as intravenous, intramuscular, subcutaneous, and inhalation. It also emphasizes the importance of understanding pharmacokinetics and patient compliance in the context of drug absorption and administration.
![Condition of Patient (Acute or Chronic)
In an acute or emergency situation, the route used must allow sufficiently fast
absorption to ensure a prompt onset of action.
Route of Choice in
Acute Condition
Parenteral Injection
(I.V., I.M., S.C.)
Intrathecal route
(for amphotericin B
in cryptococcal
meningitis)
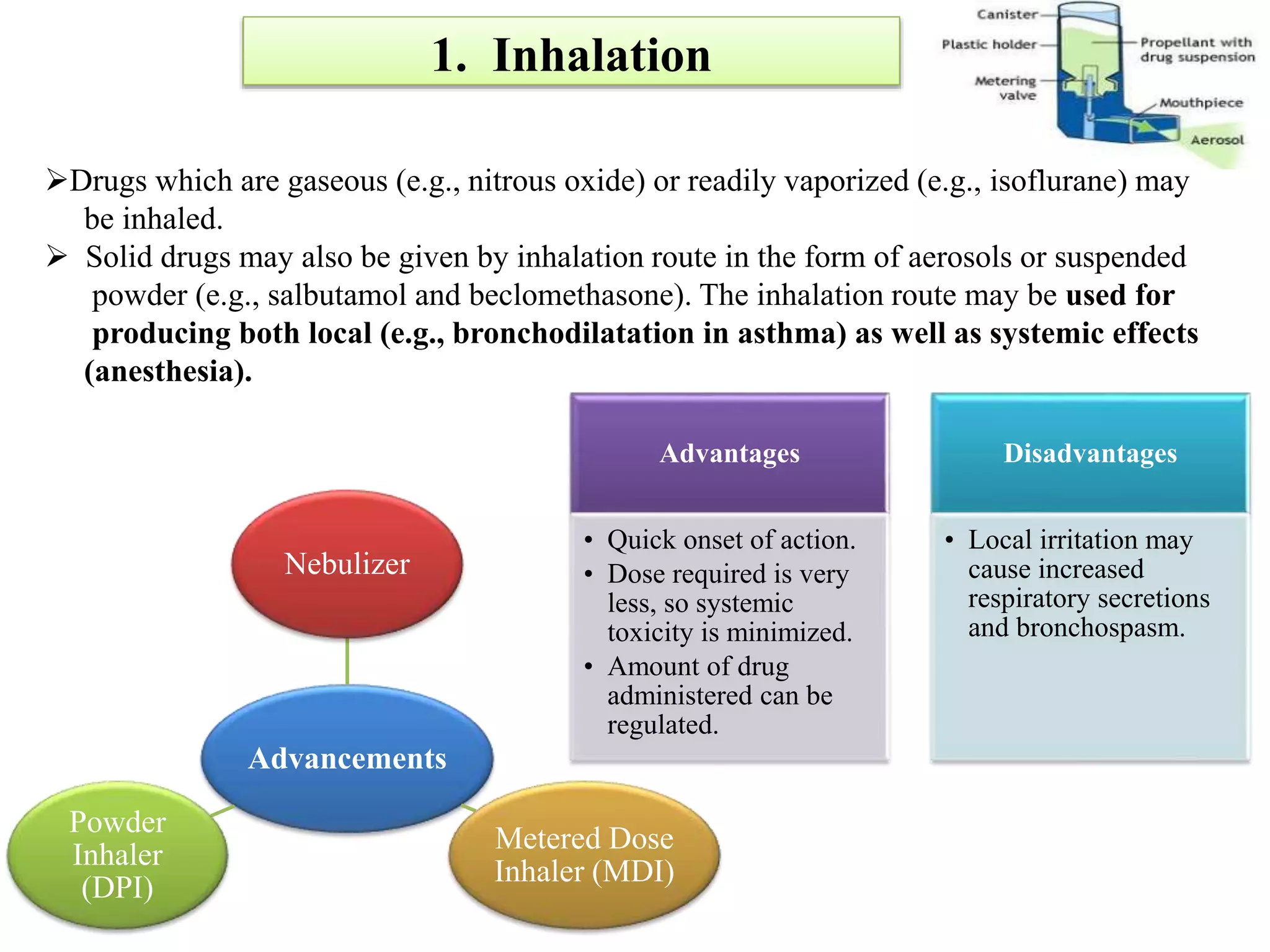
Inhalation Route (for
bronchodilators [by
nebulizer] in acute
bronchial asthma attack)
Sublingual Route (for
nitroglycerin in acute
angina attack)
With young children, the rectal route (as enema or suppository) may also be used,
especially when the patient is unconscious or when vomiting occurs.](https://image.slidesharecdn.com/routesofadministration-190206074844/75/Routes-of-administration-4-2048.jpg)