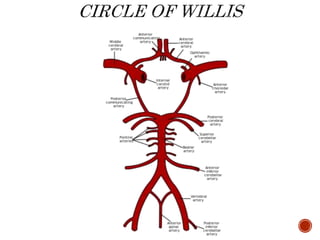
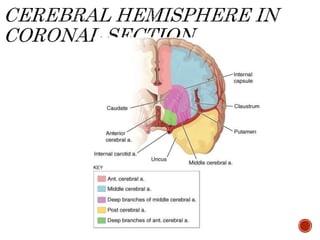
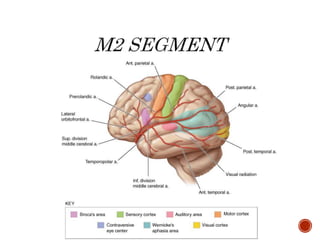
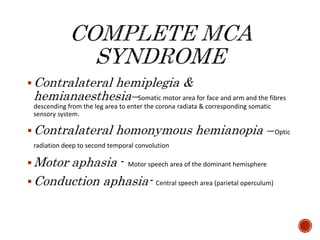
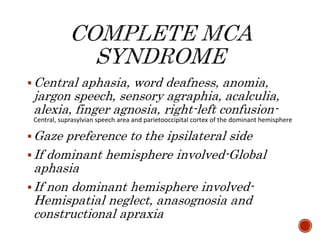
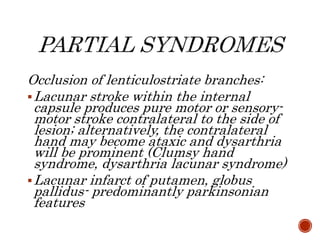
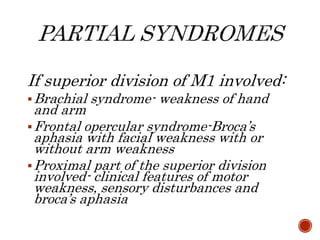
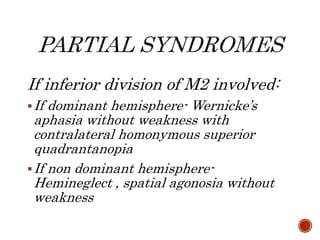
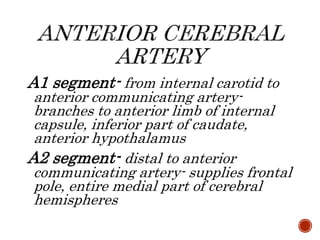
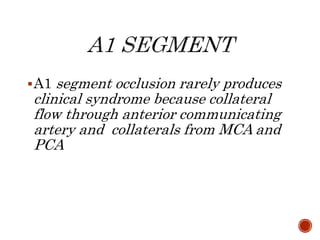
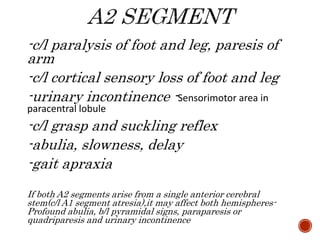
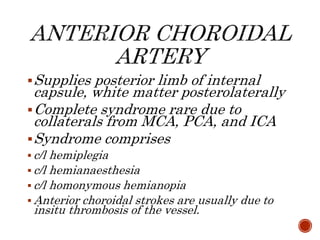
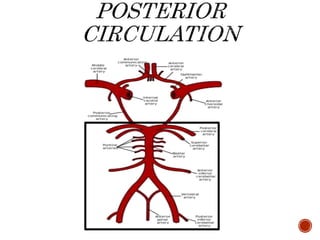
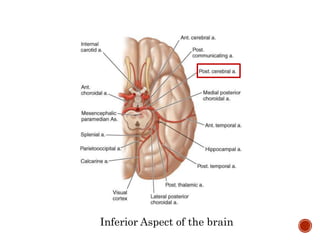
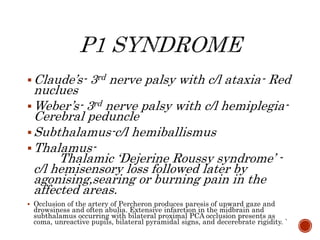
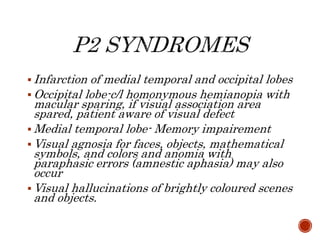
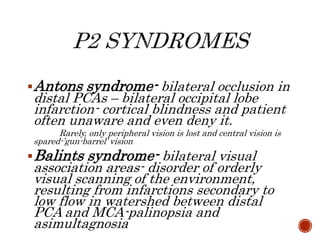
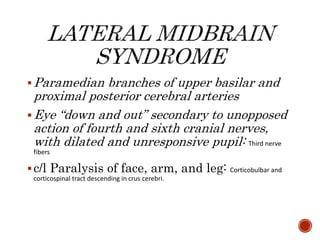
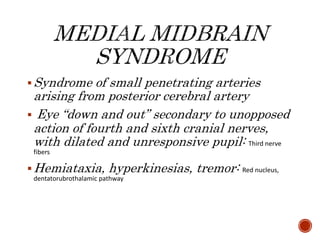
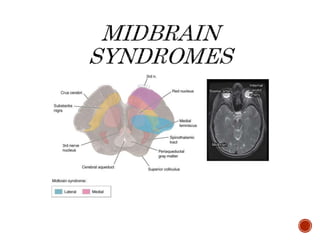
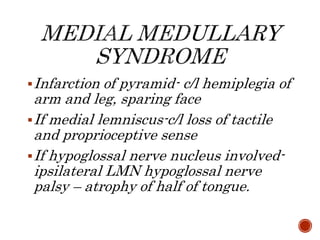
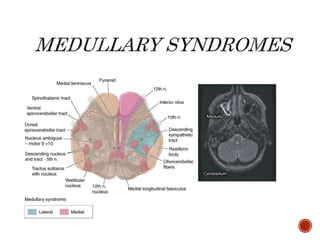
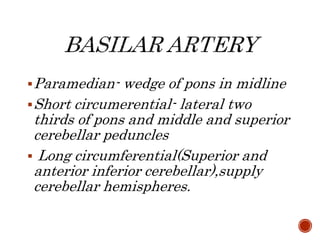
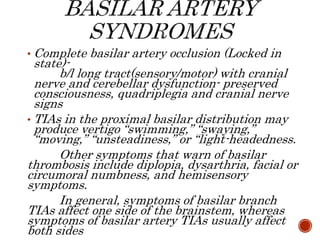
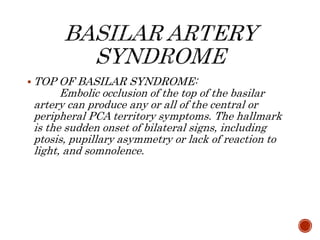
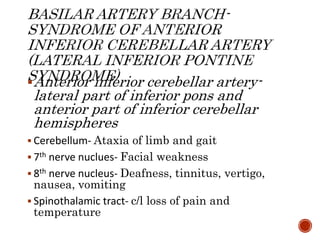
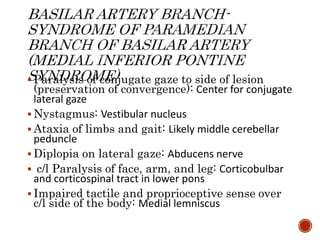
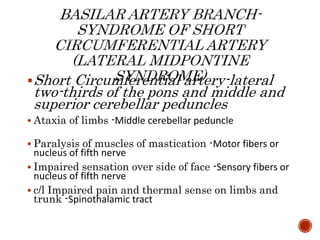
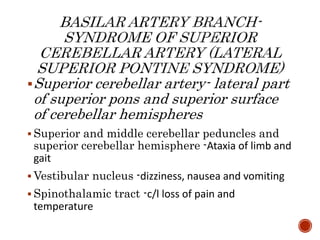
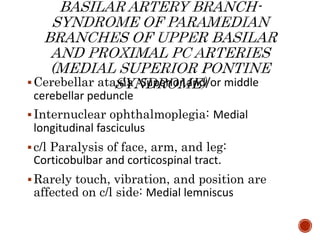
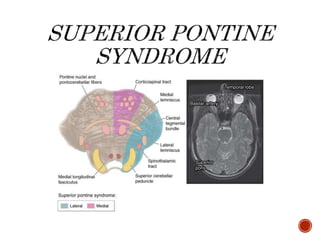
This document describes the anatomy and clinical presentations of strokes caused by occlusions in the major arteries that supply the brain. It discusses strokes in the anterior and posterior circulations, including the territories supplied by the internal carotid, vertebral, basilar and cerebral arteries. For each artery, it outlines the signs and symptoms that result from occlusions in different vessel segments, such as hemiplegia, aphasia and homonymous hemianopia.