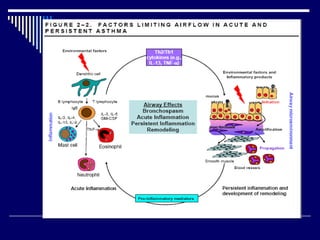
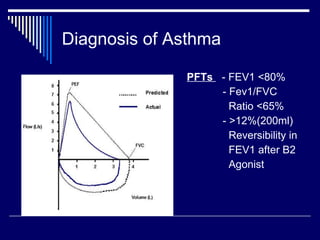
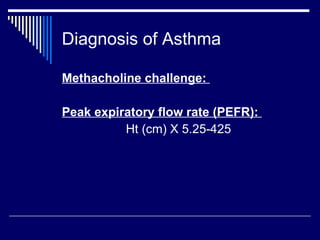
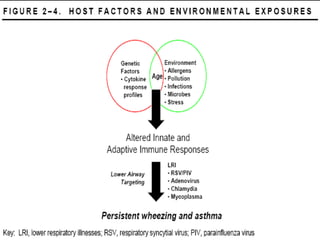
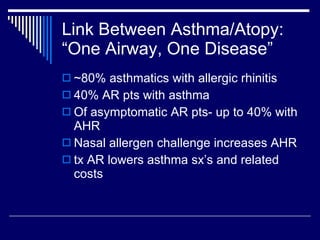
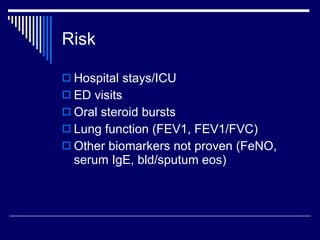
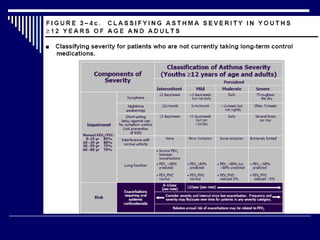
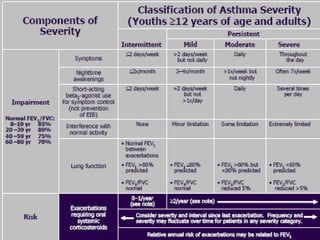
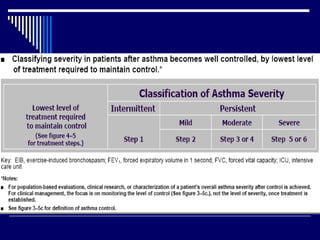
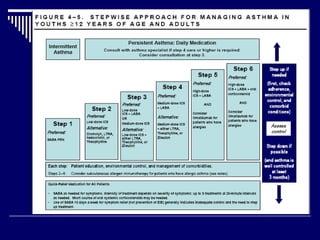
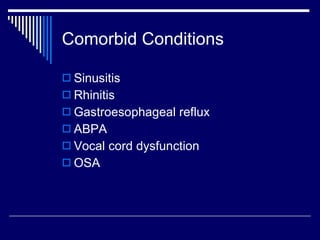
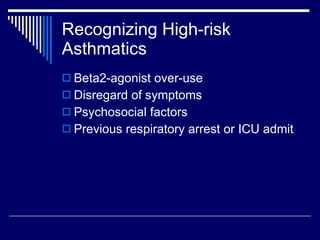
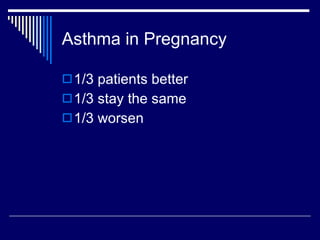
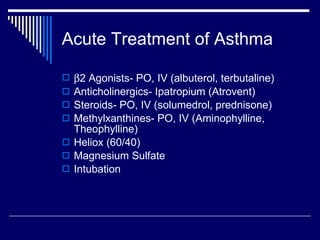
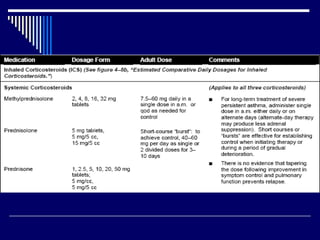
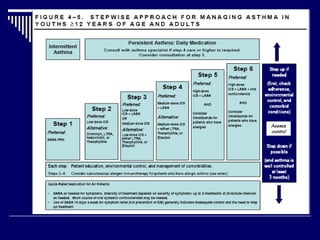
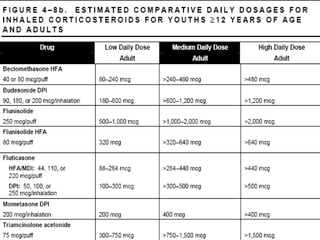
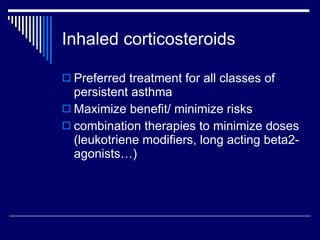
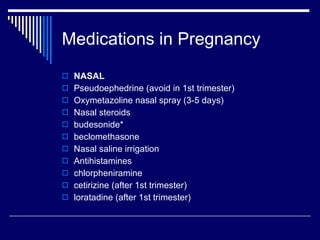
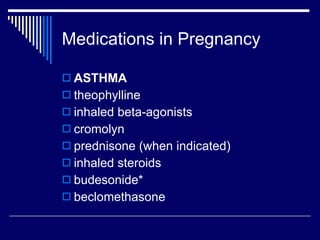
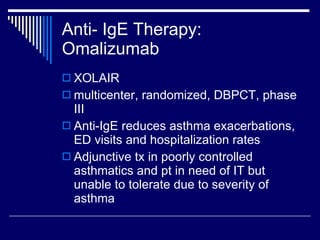
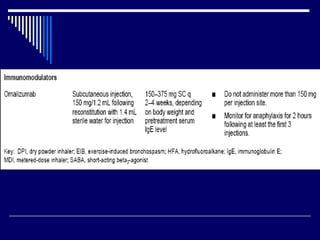
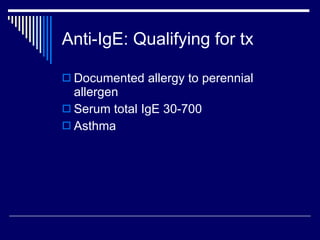
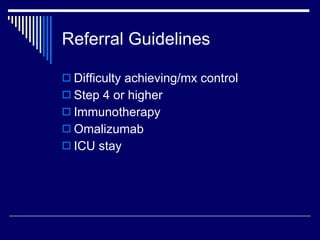
This document provides an overview of asthma diagnosis and management. It discusses defining asthma as a chronic inflammatory airway disease, guidelines for diagnosis and assessing severity, common precipitating factors and comorbidities, and treatment options including inhaled corticosteroids as first-line controller therapy and omalizumab for severe uncontrolled asthma. It also addresses special considerations for asthma diagnosis and treatment during pregnancy.