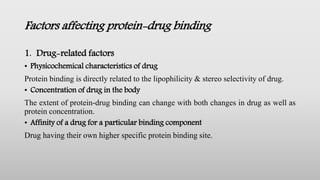
The document discusses protein-drug binding interactions, detailing the mechanisms, types, and factors influencing binding between drugs and proteins, particularly within blood and extravascular tissues. It explains the significance of protein binding in drug absorption, distribution, elimination, and potential therapeutic applications. Additionally, it highlights various binding components such as plasma proteins and specific interactions that can impact drug efficacy and safety.









![3. Drug interactions
a. Competition between drugs for the binding sites [ Displacement interactions]
• When two or more drugs can bind to the same site, competition between them for
interaction with the binding site results.
• Such drug-drug interaction for the common binding site is called as displacement
interaction.
b. Competition between drug & normal body constituents
• The free fatty acids are known to interact with a no. of drugs that binds primarily
to HAS. The free fatty acid level increase in
• Physiological (fasting)
• Pathological (diabetes, myocardial infraction)
• Pharmacologically induced (after heparin or caffeine administration)](https://image.slidesharecdn.com/proteinbindingofdrugs-210617105752/85/Protein-binding-interactions-12-320.jpg)