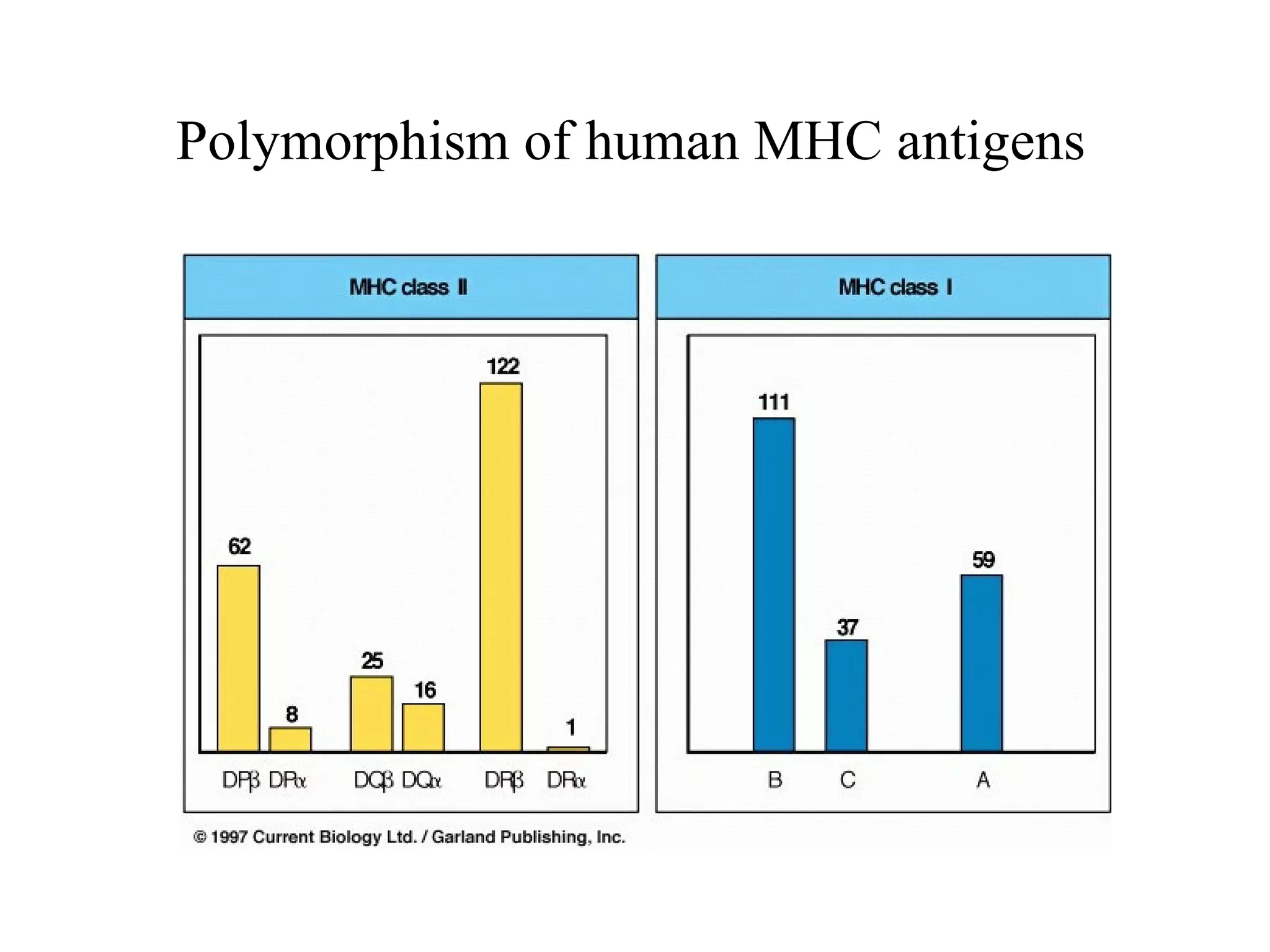
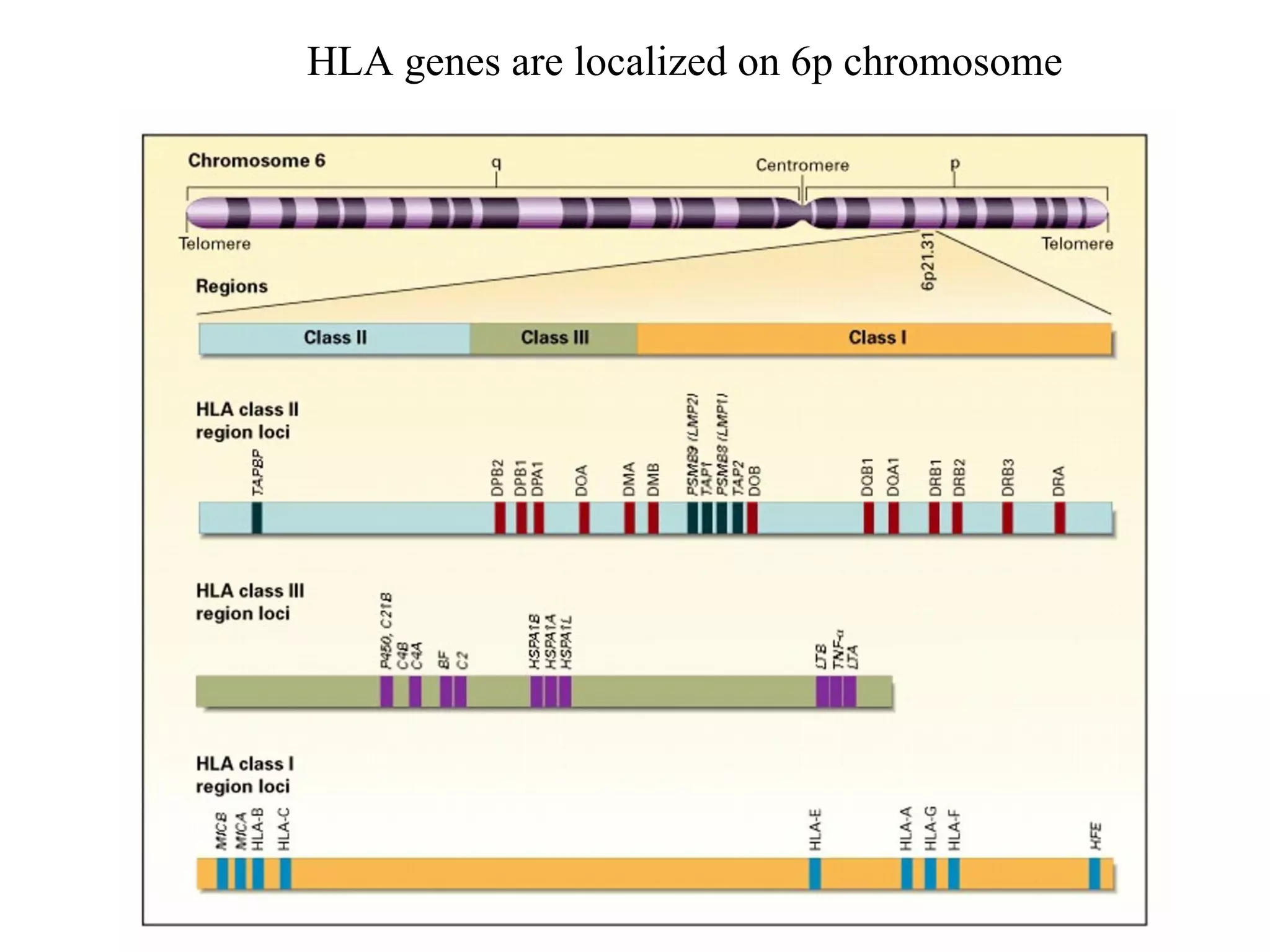
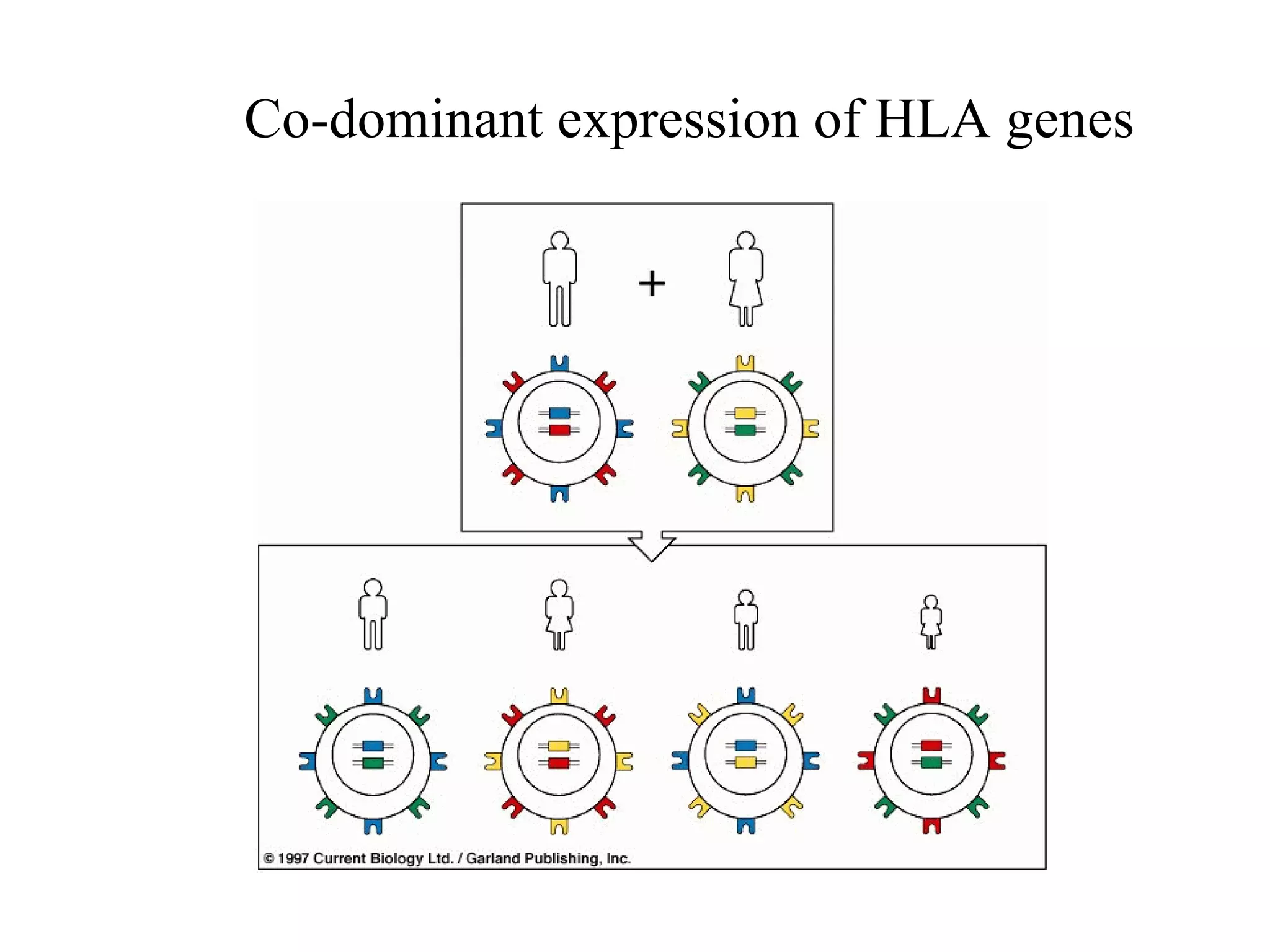
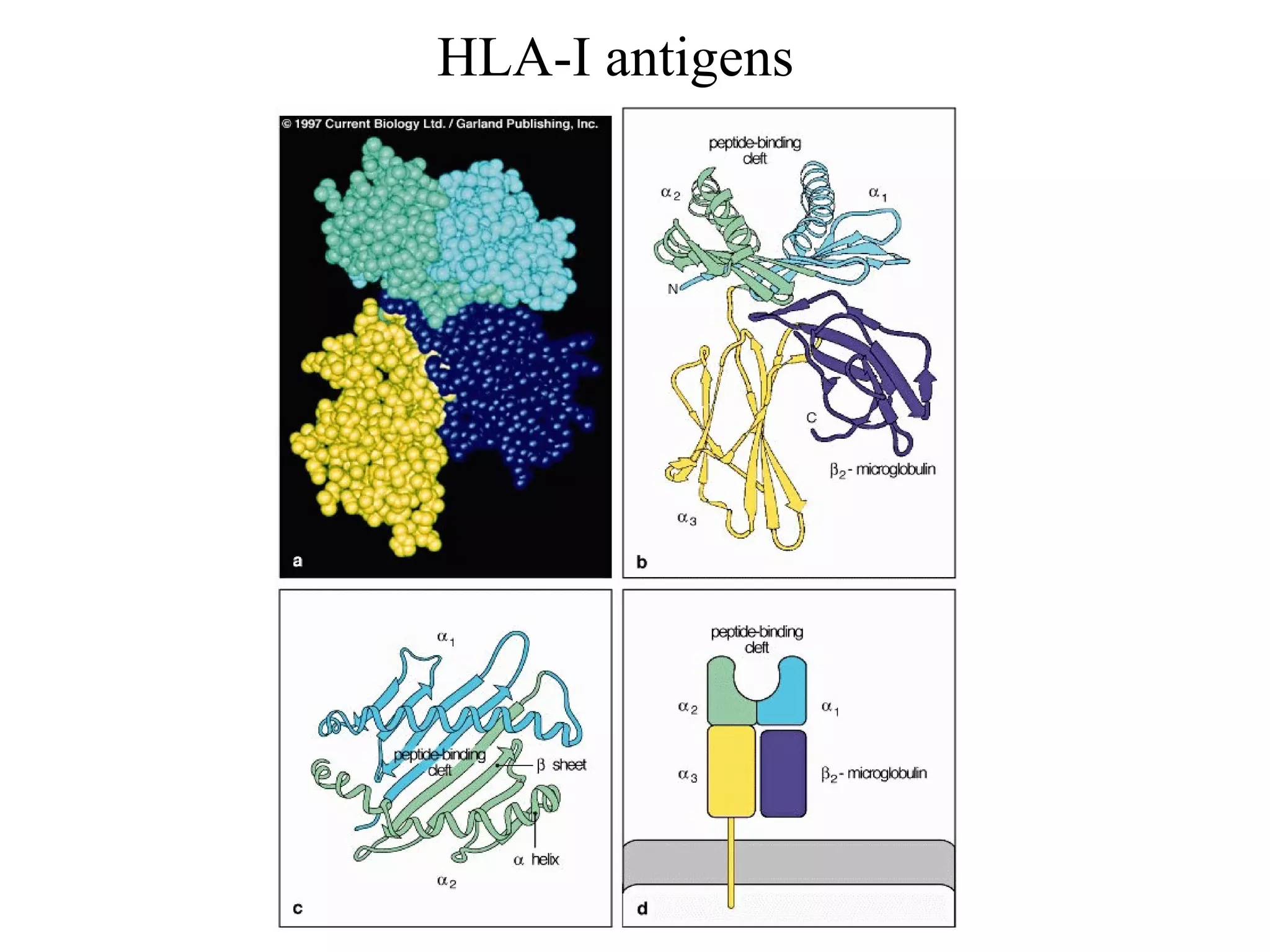
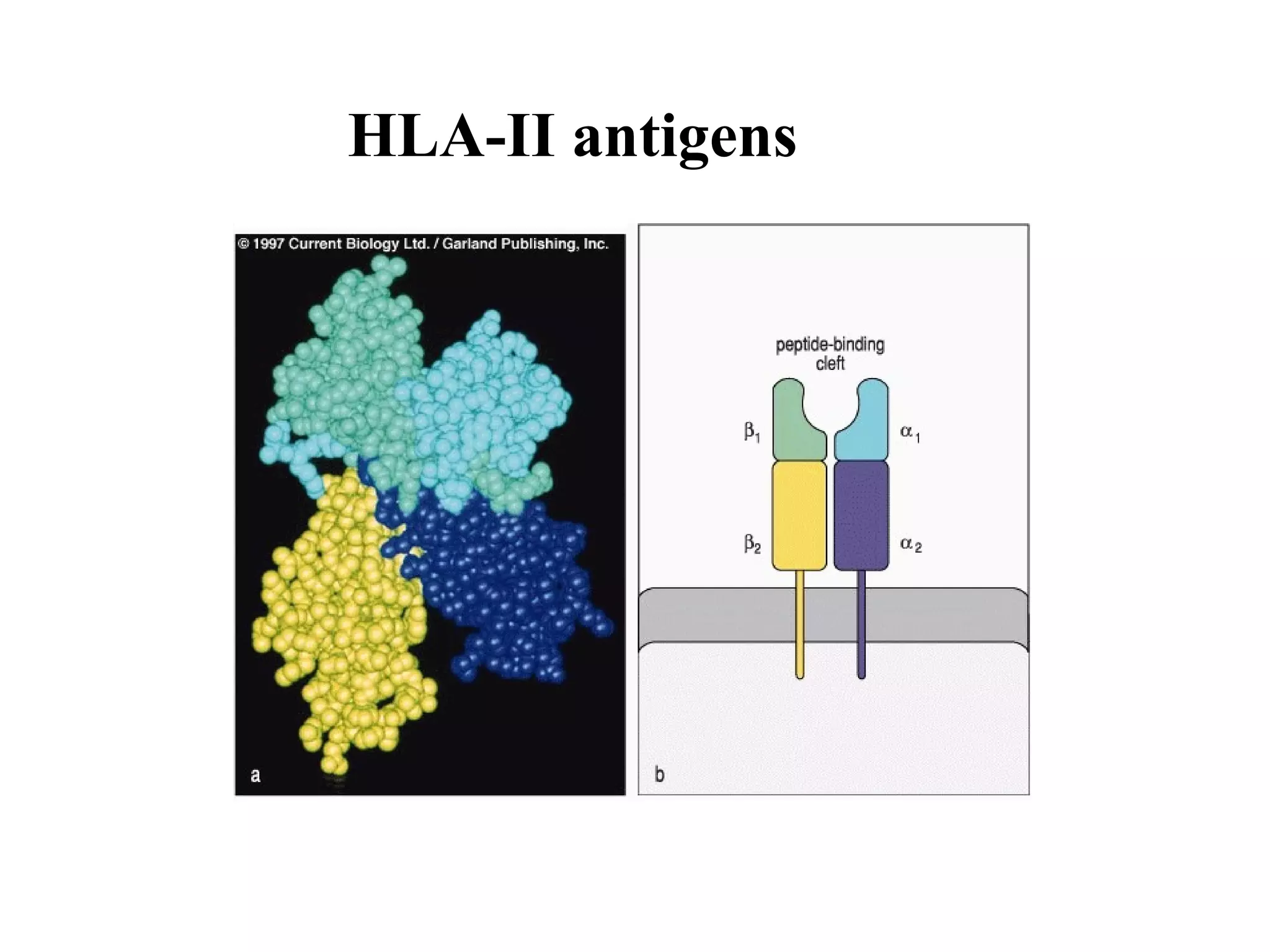
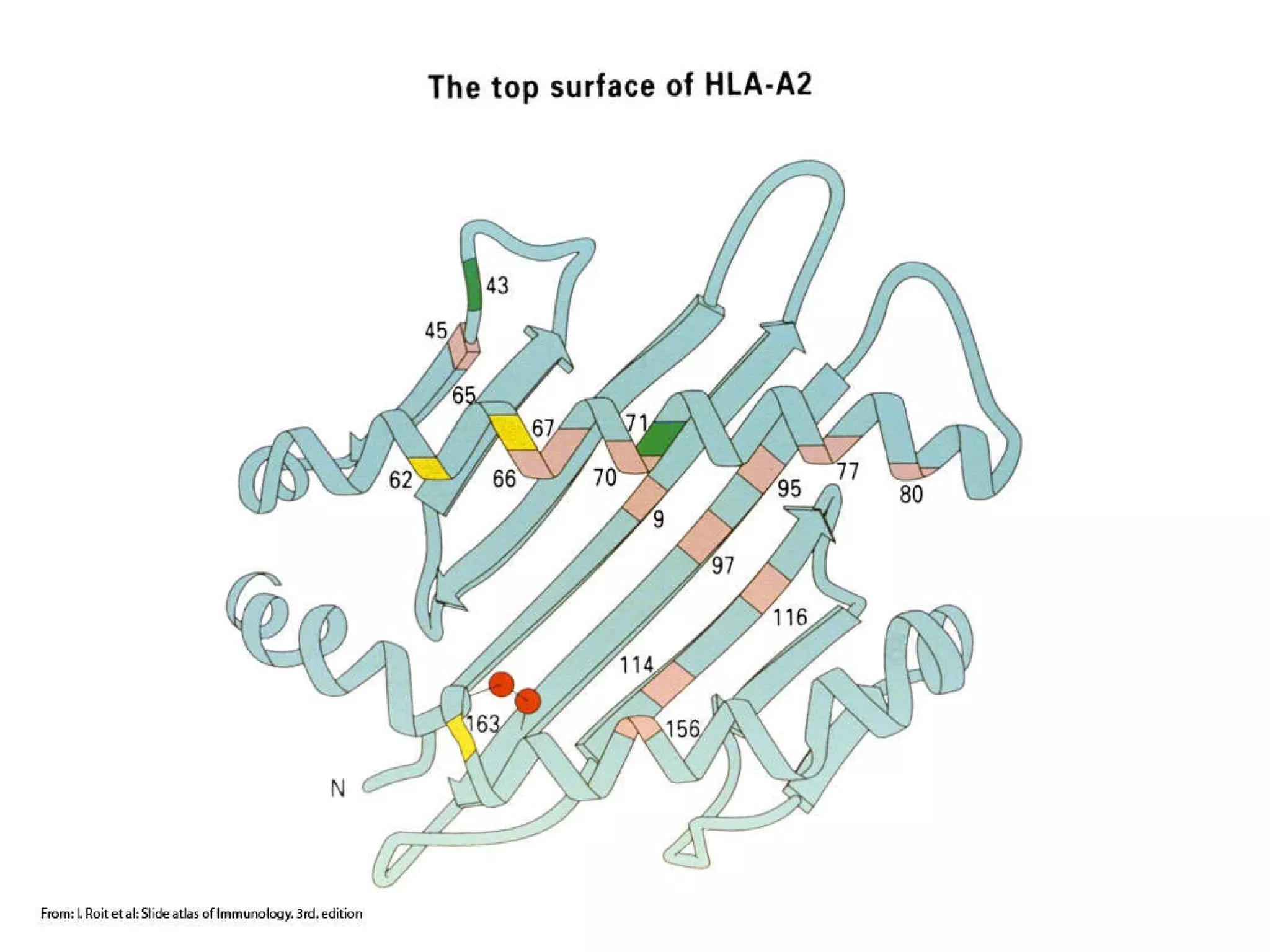
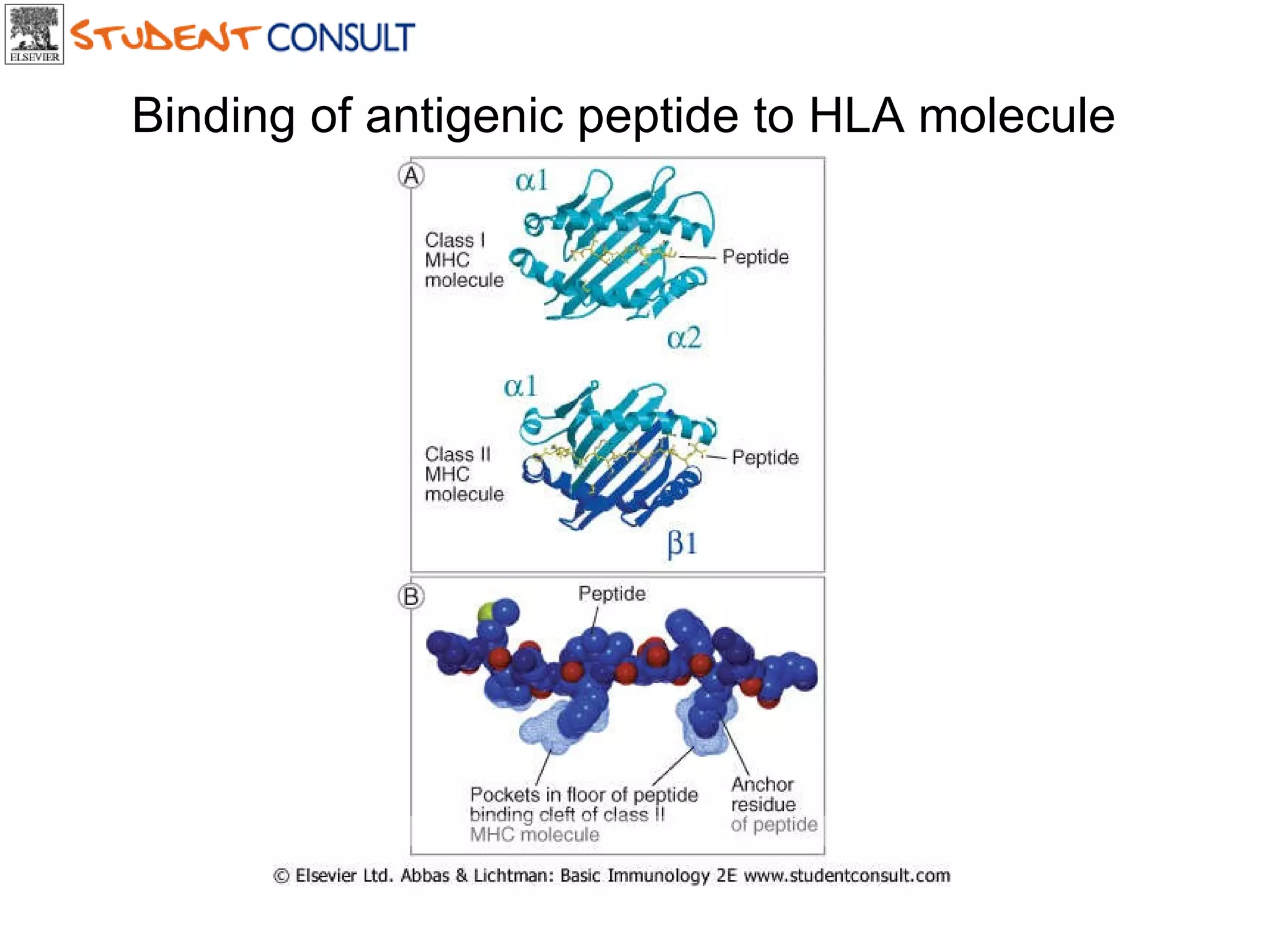
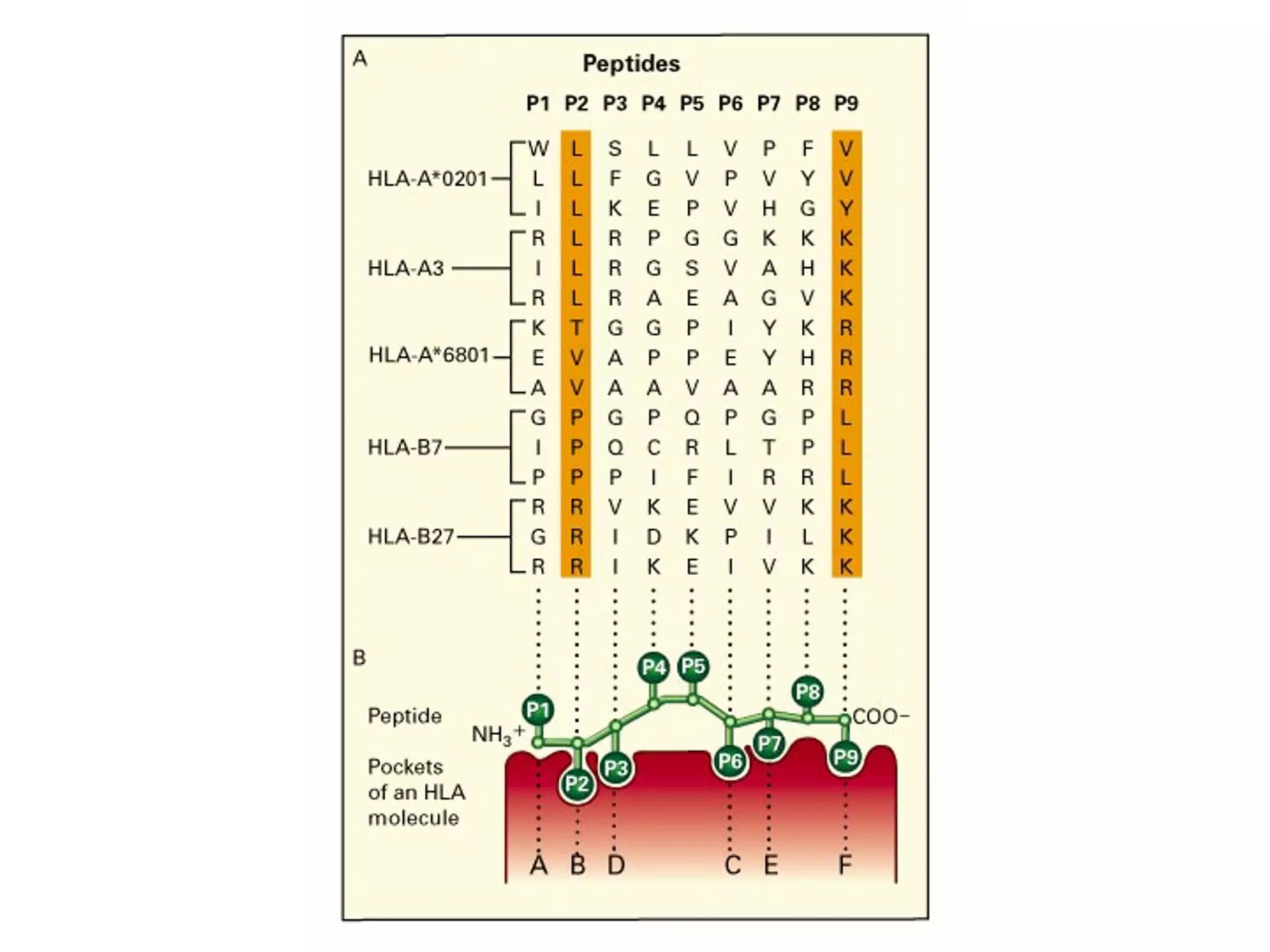
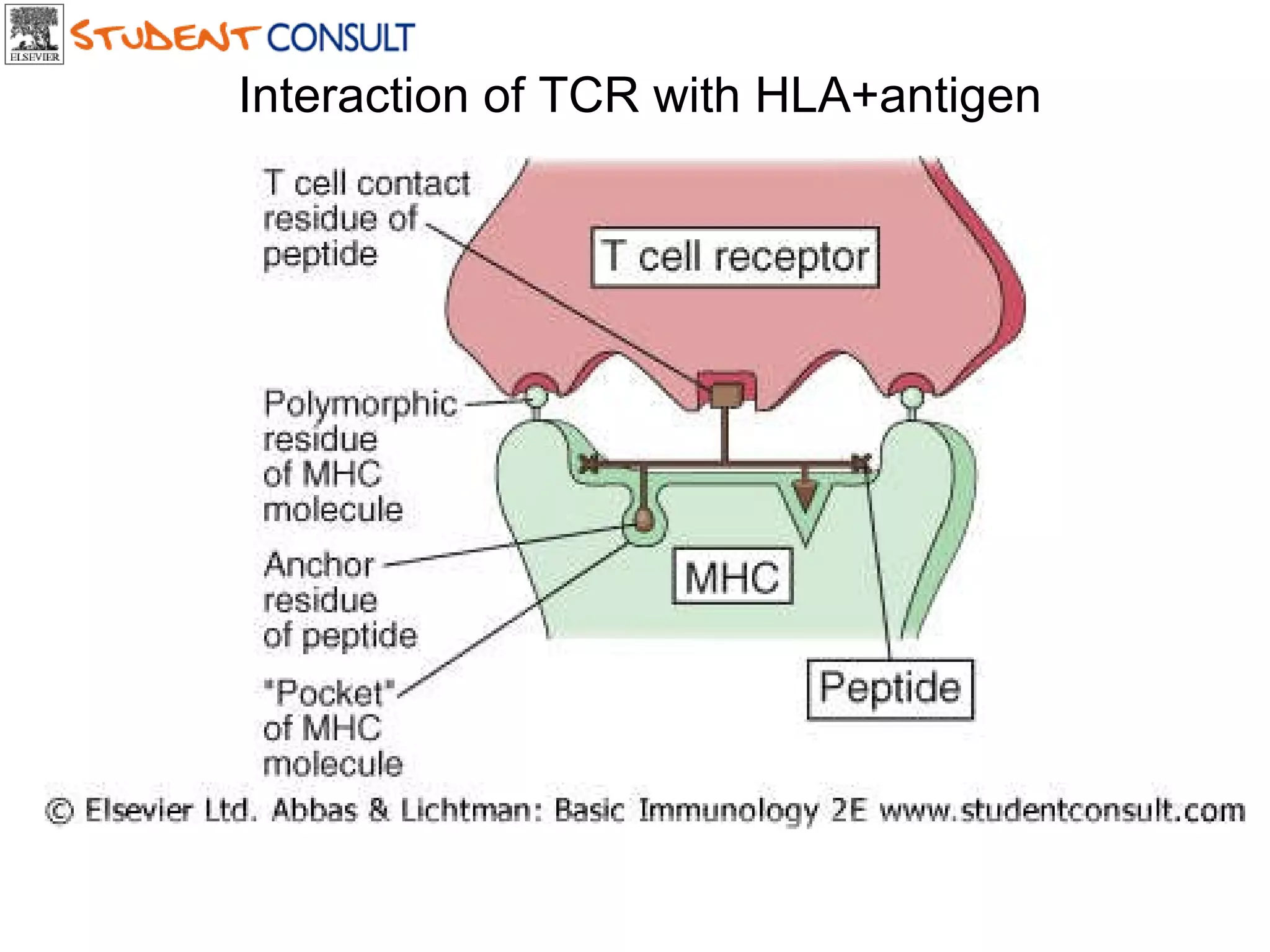
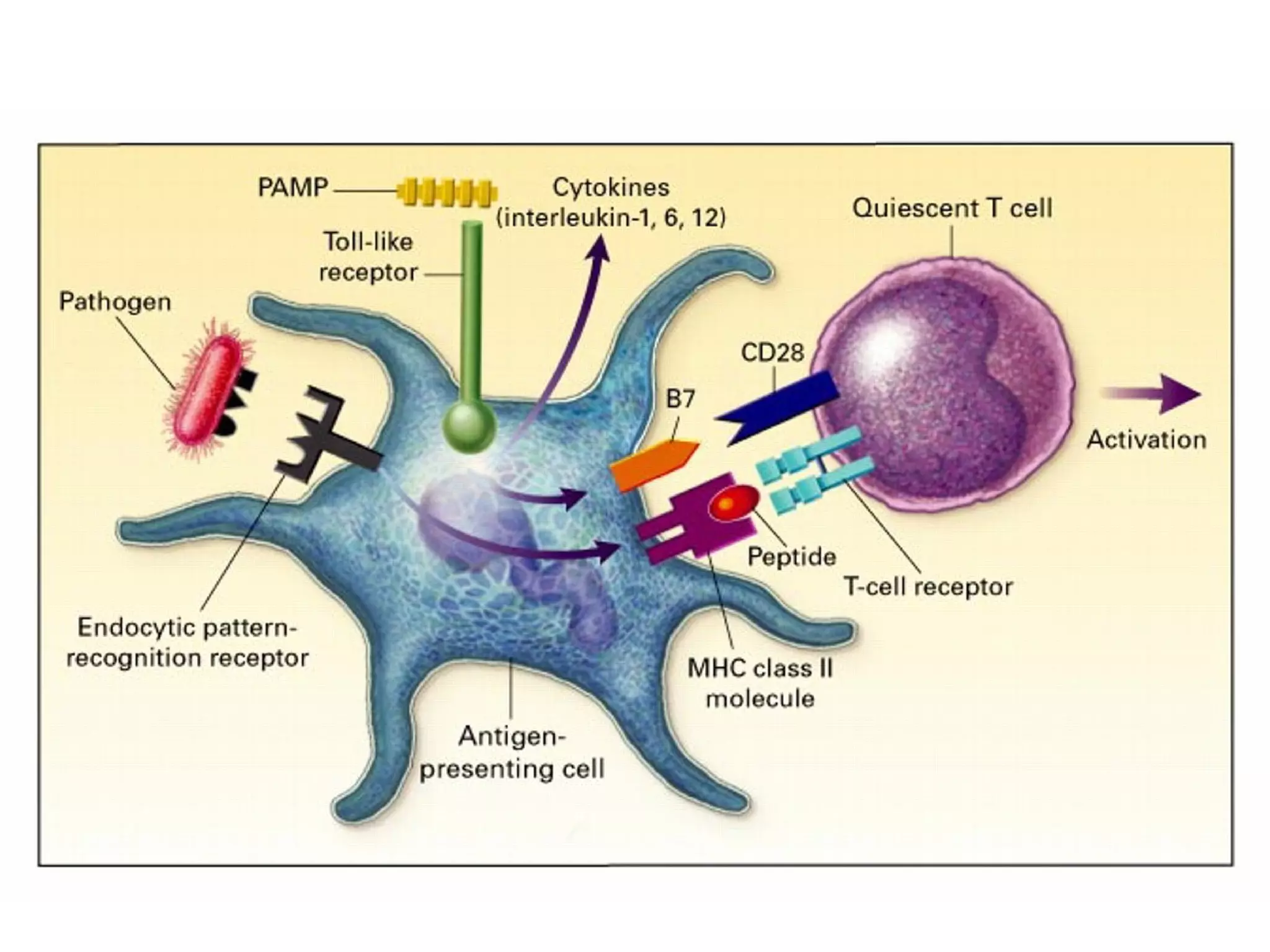
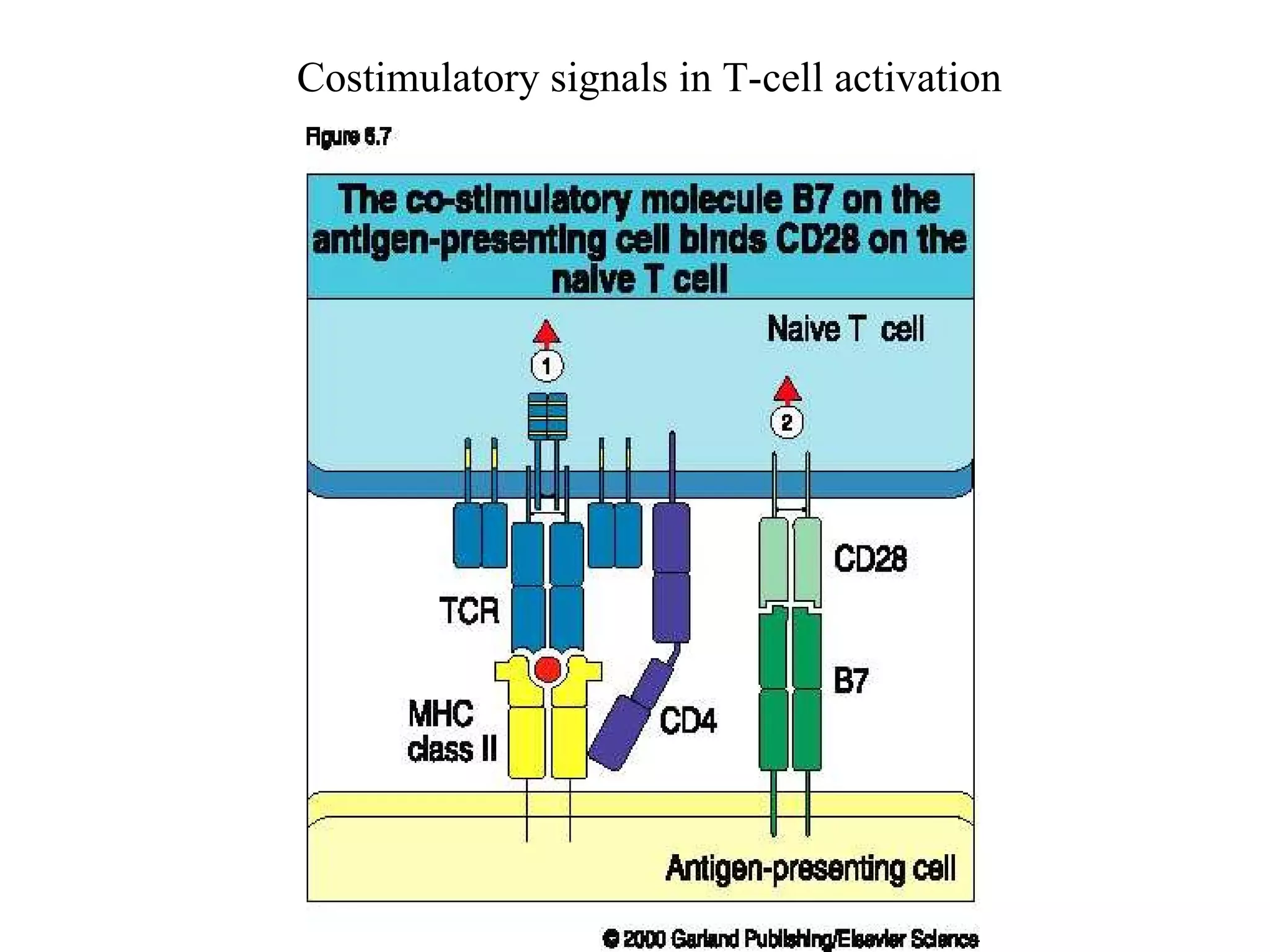
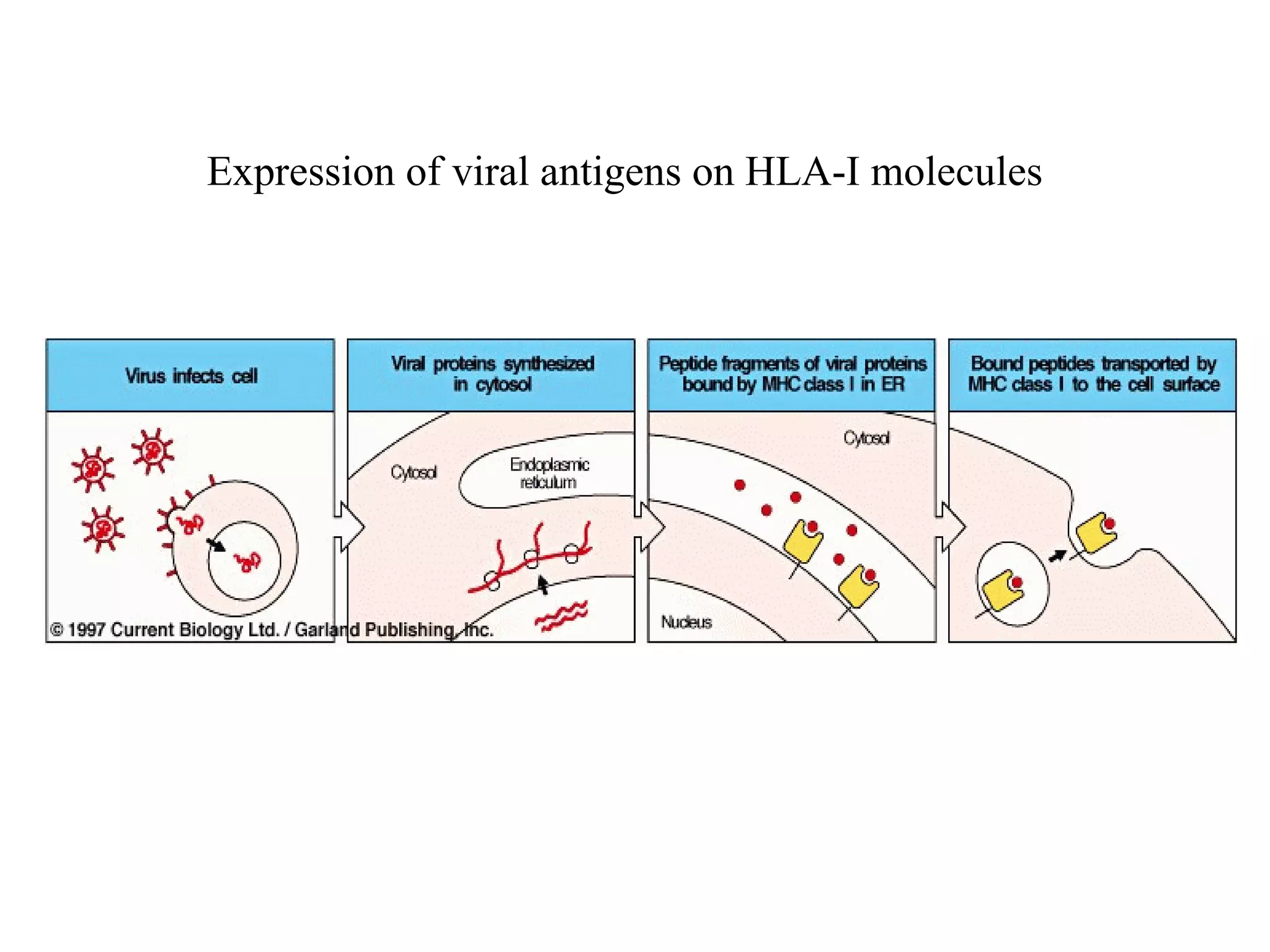
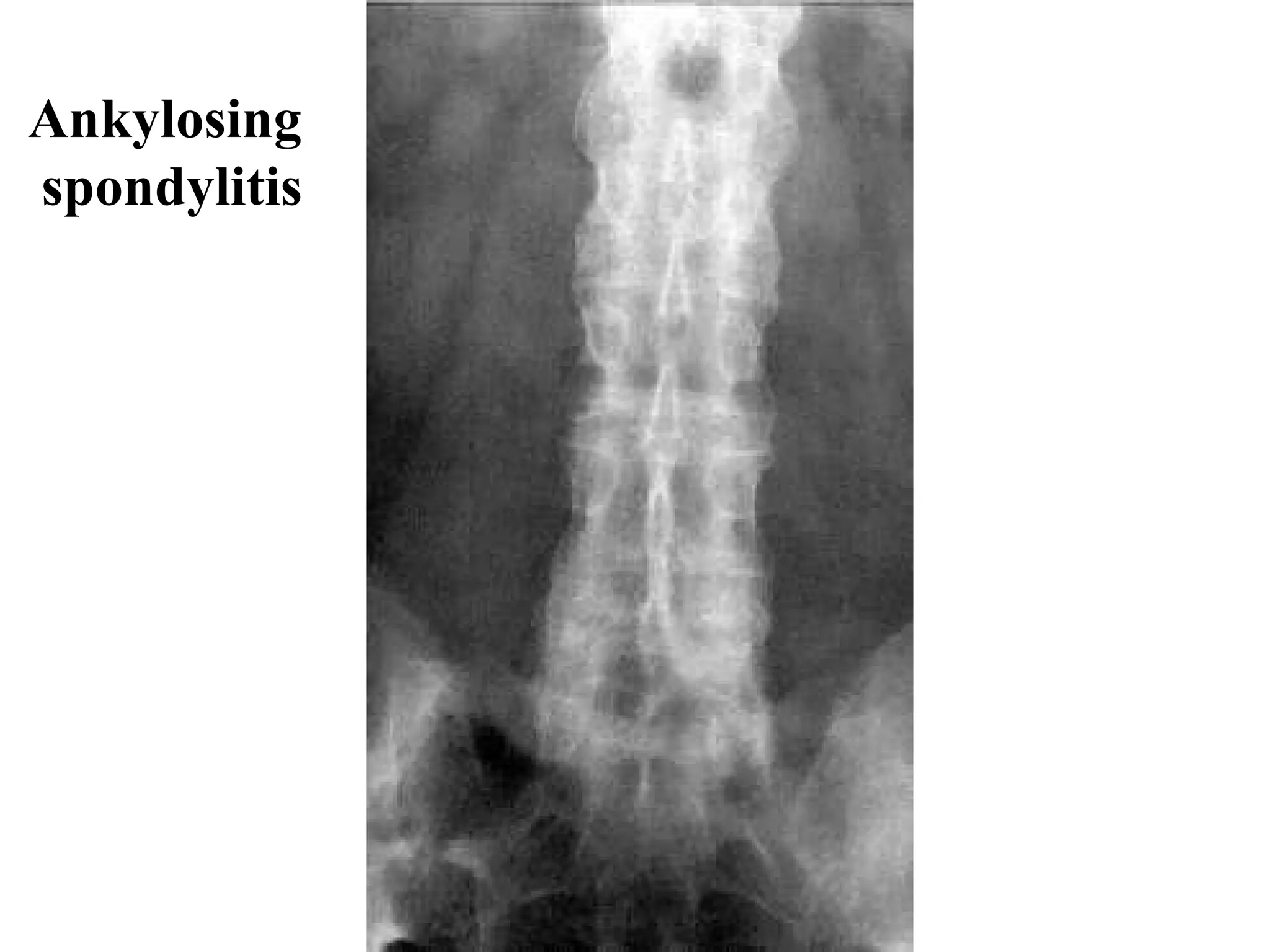
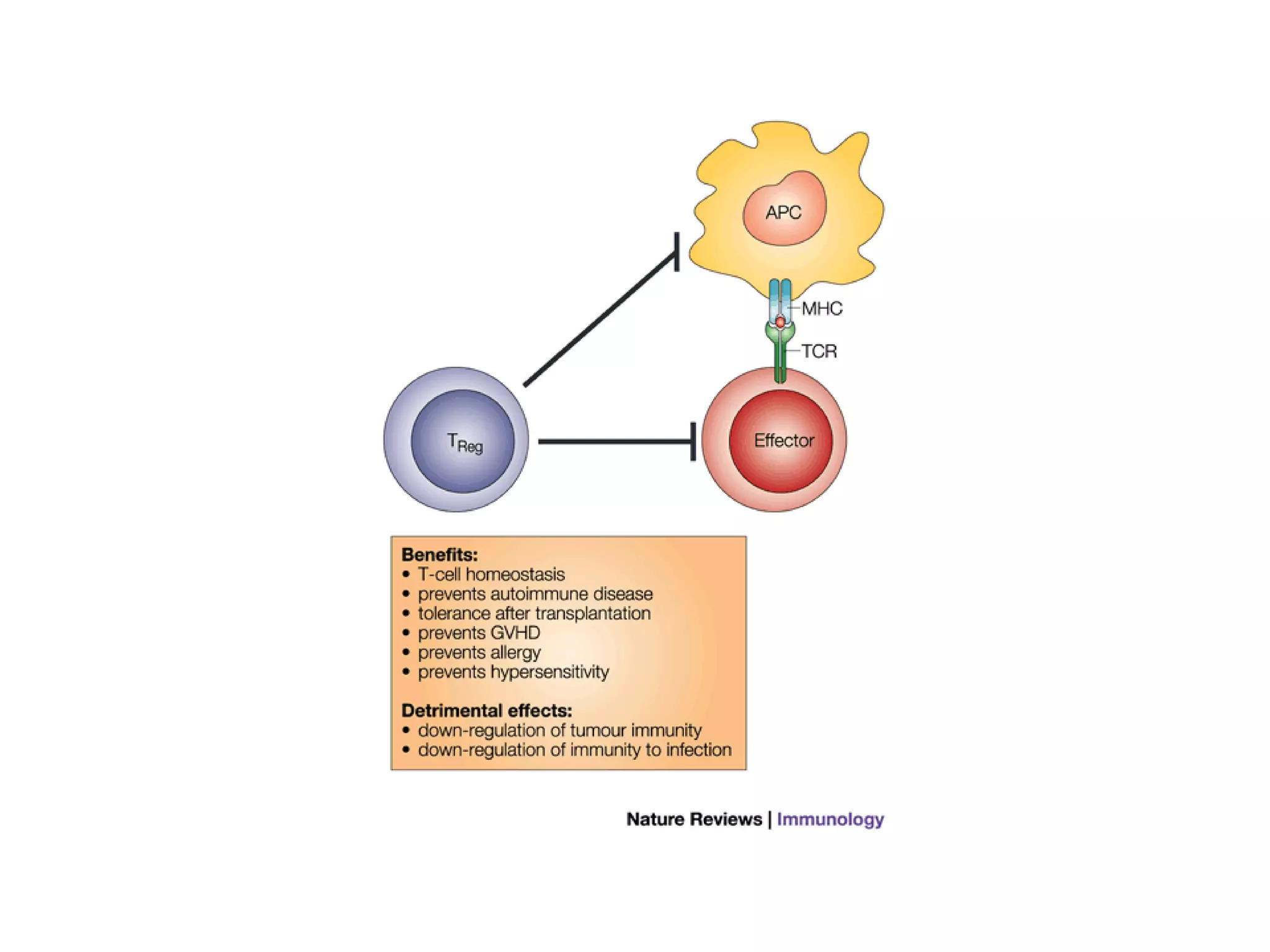
Human Leukocyte Antigens (HLA) are human MHC antigens located on chromosome 6p that show polymorphism and co-dominant expression. There are two main types of HLA antigens - HLA class I and II. HLA molecules present antigenic peptides to initiate immune responses through interactions with T-cell receptors. Certain diseases like ankylosing spondylitis are associated with particular HLA antigens due to increased relative risk, though most carriers of risk alleles do not develop diseases. Cytokines play important regulatory roles in immune responses through effects on cells like macrophages, granulocytes, and lymphocytes.