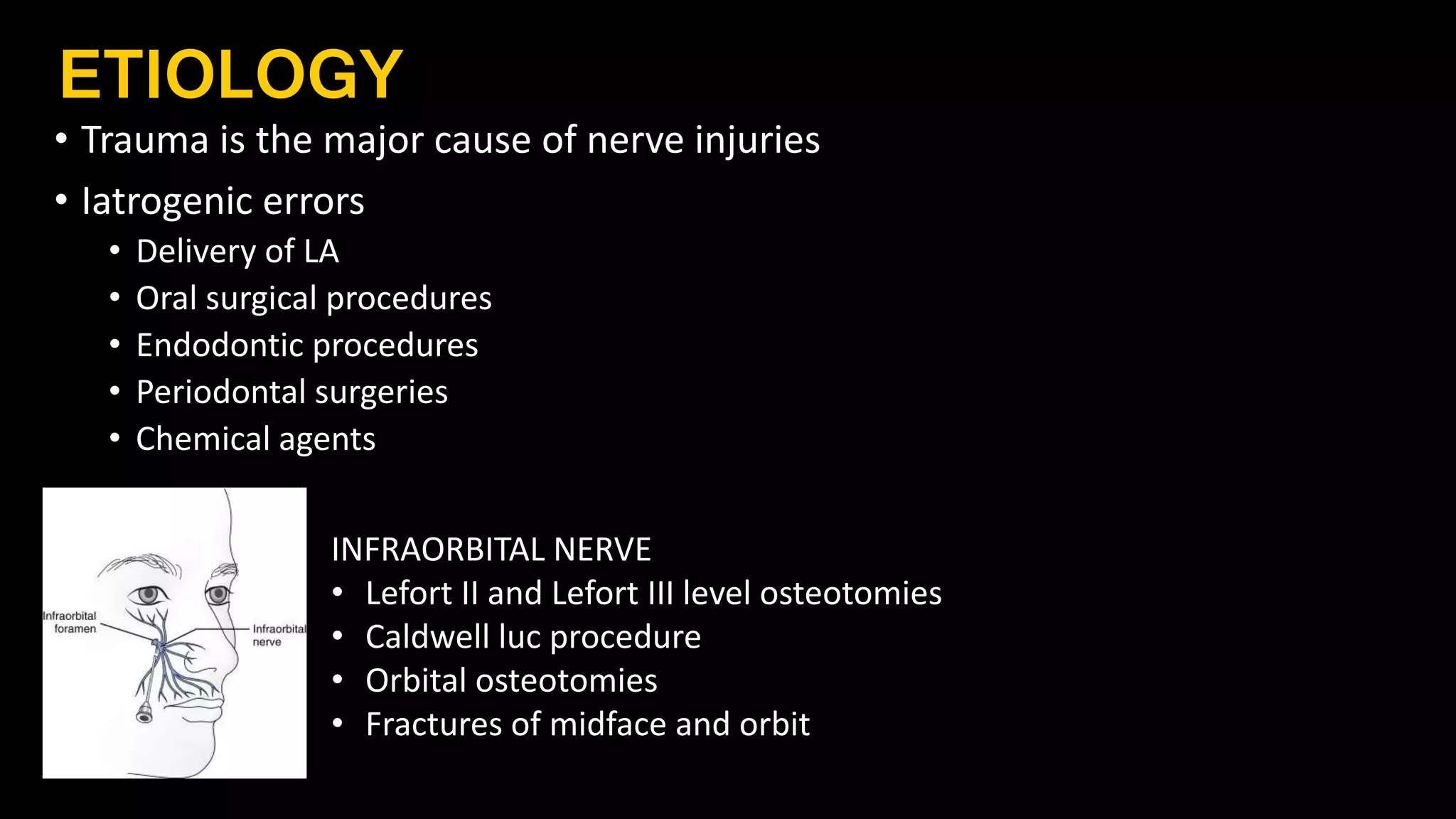
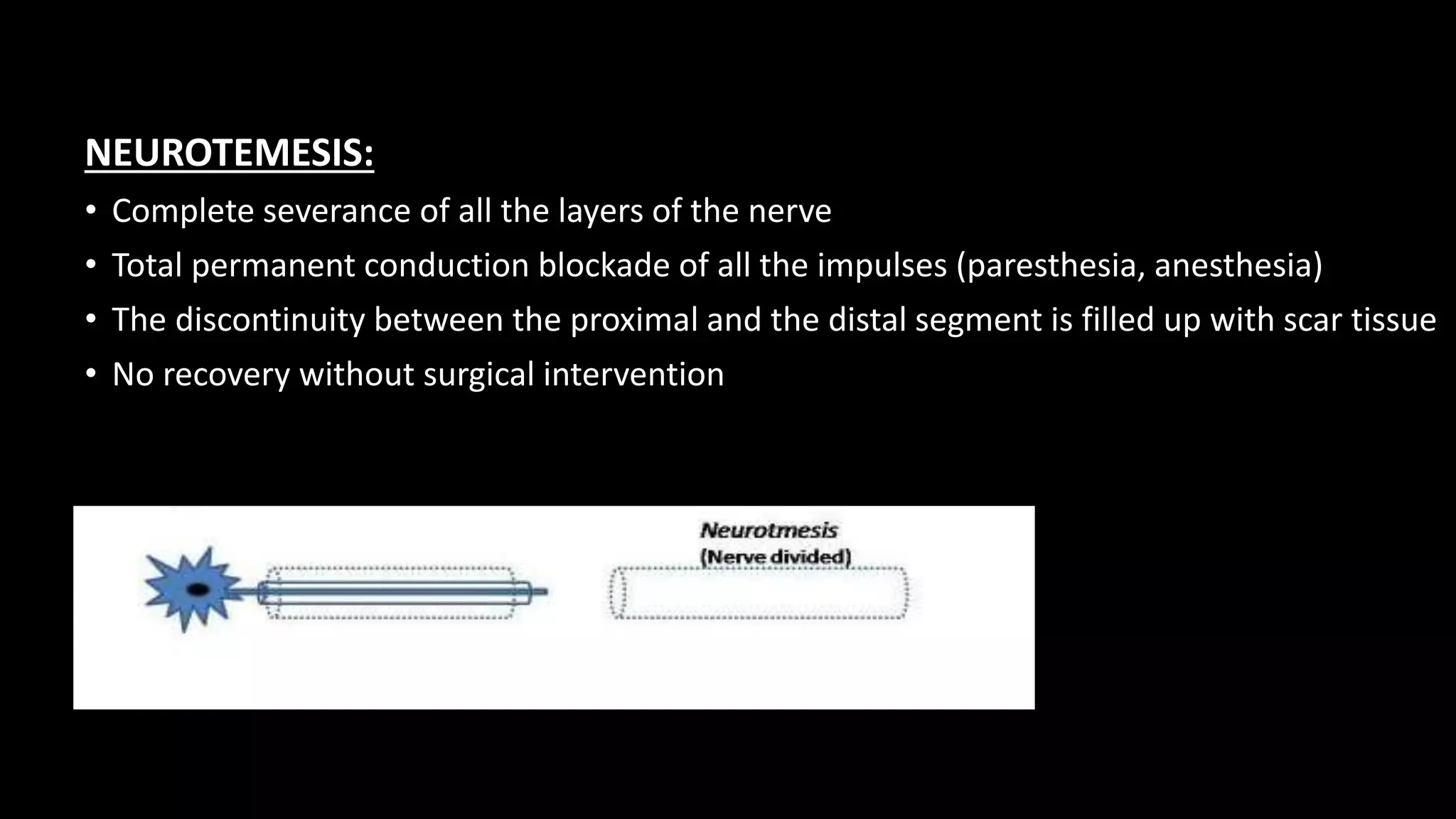
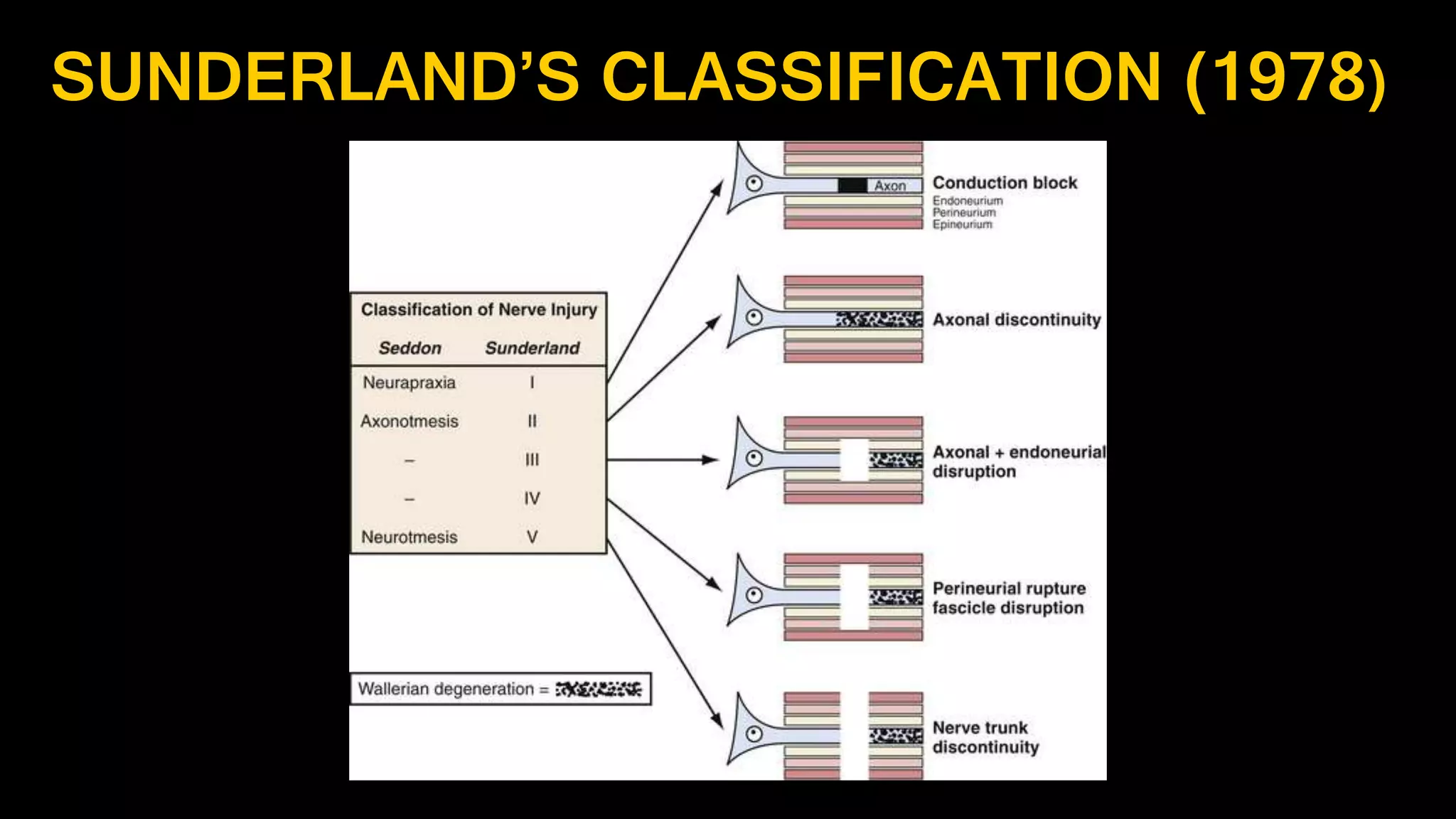
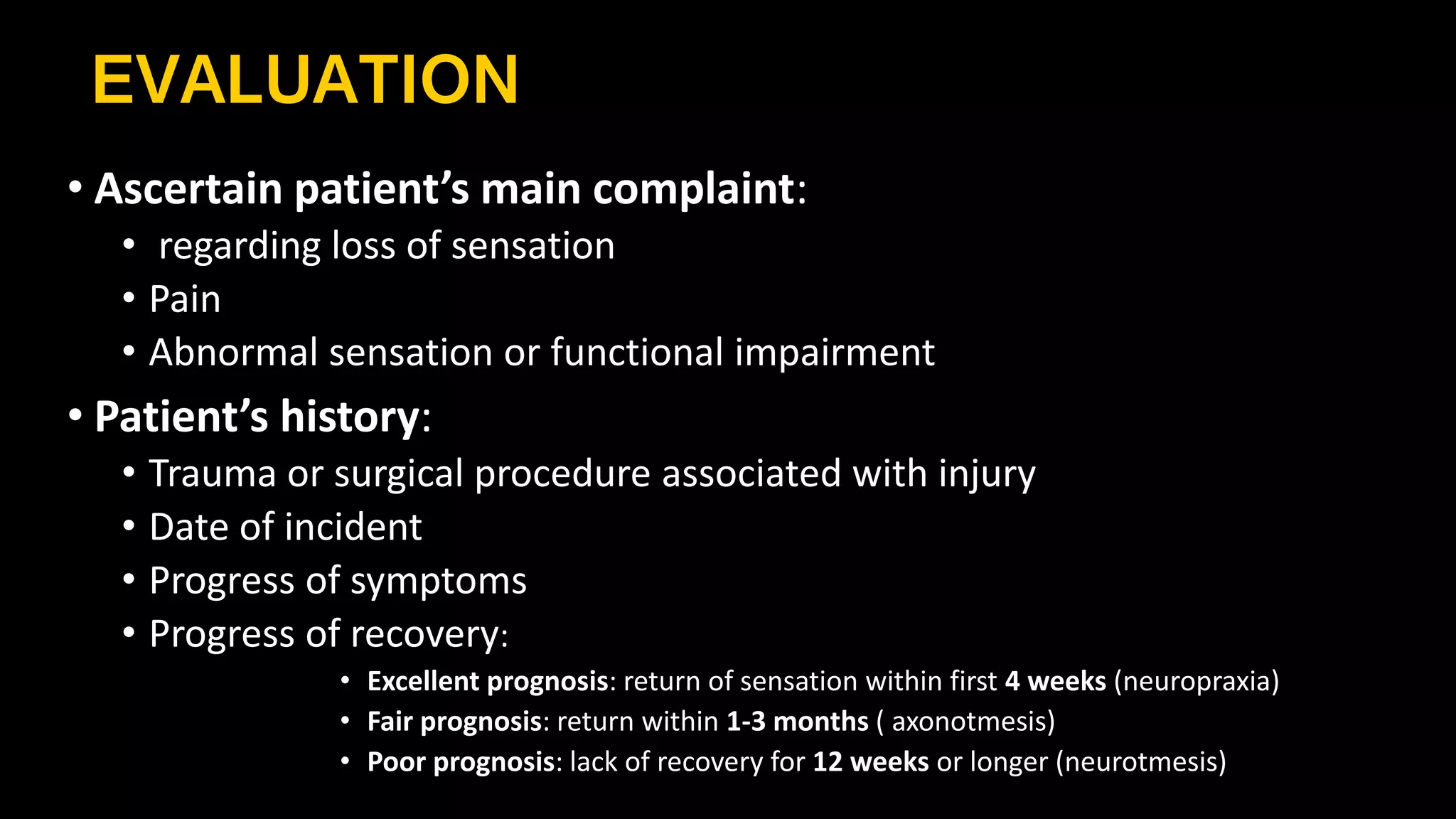
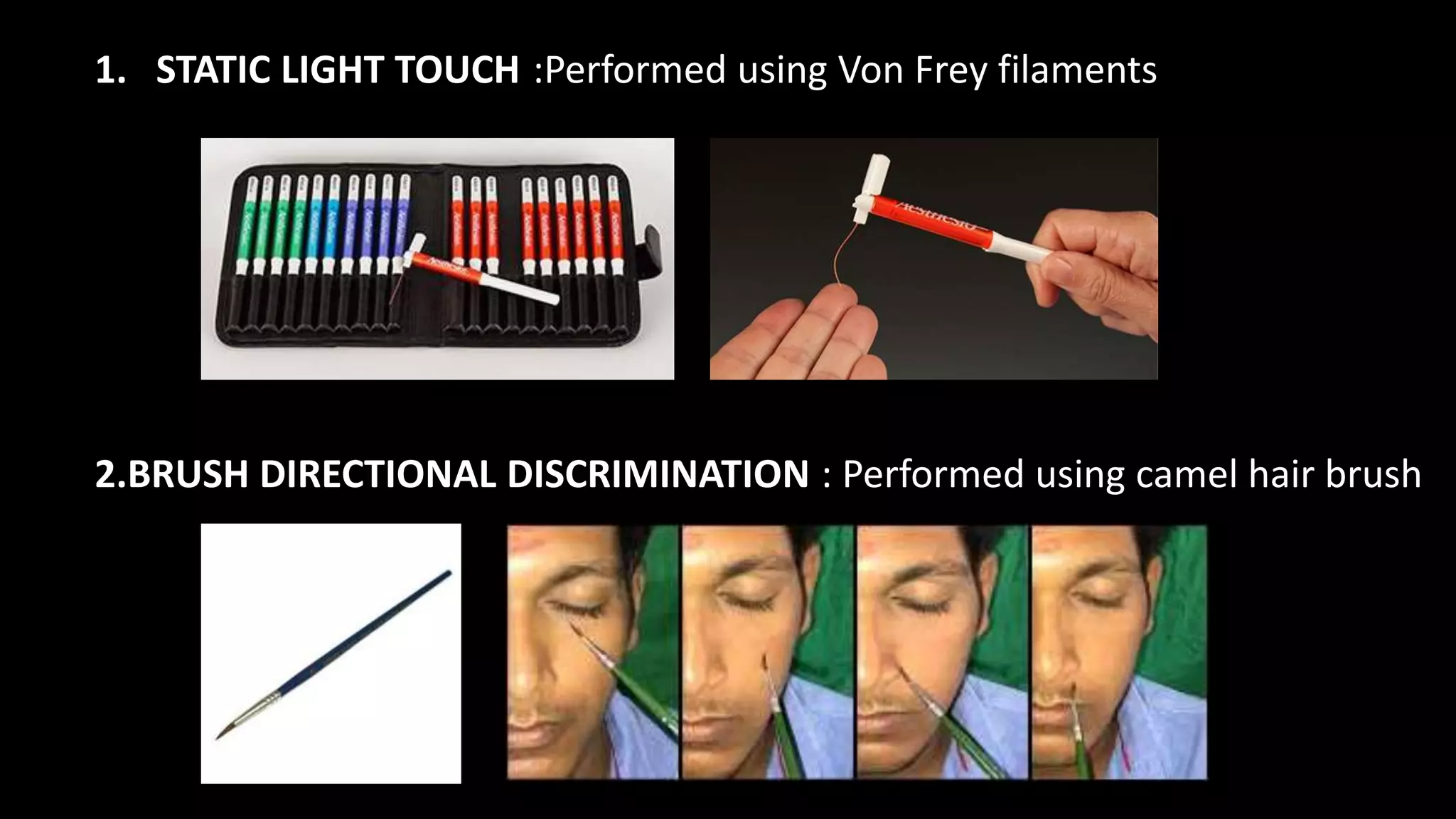
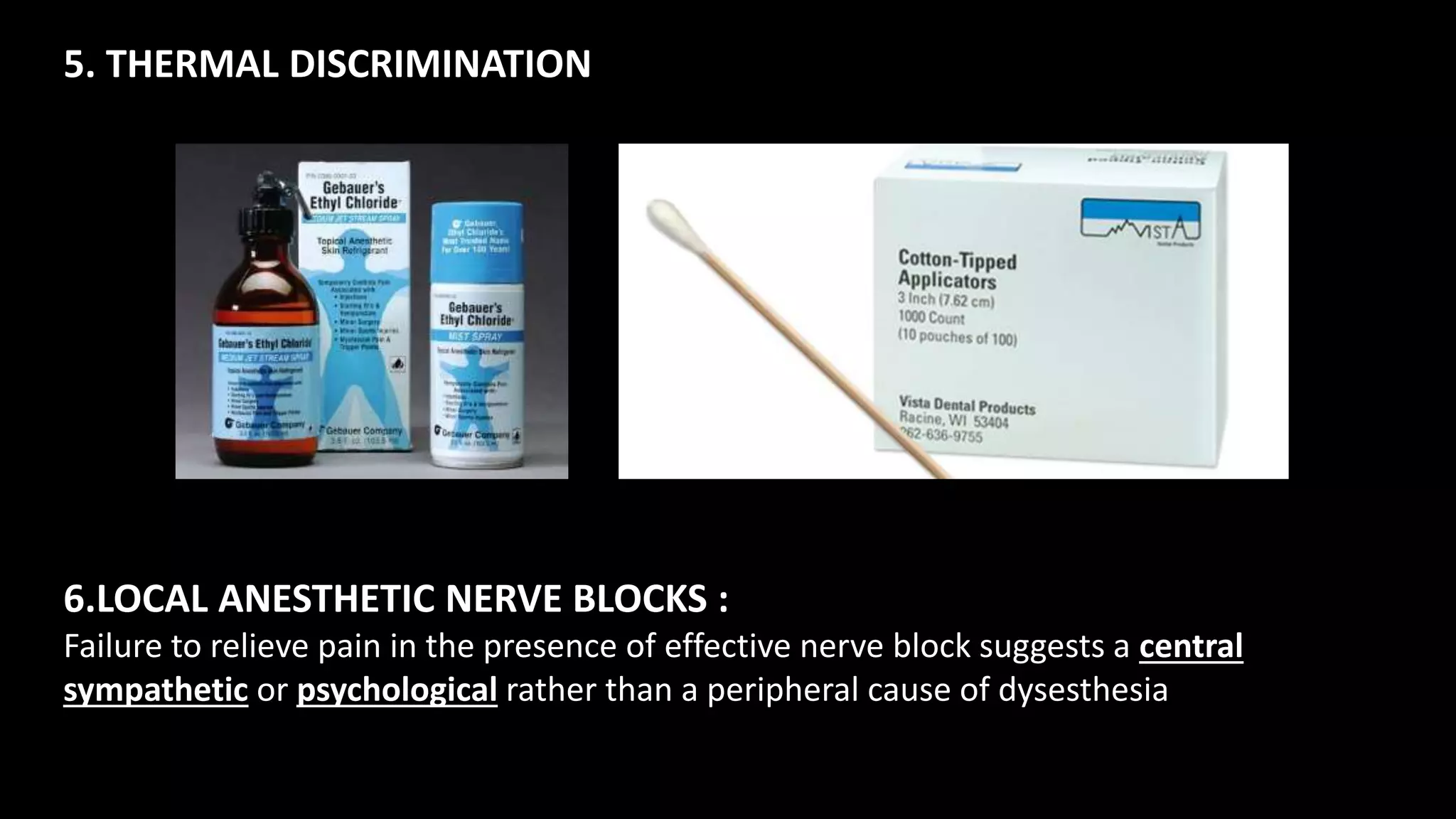
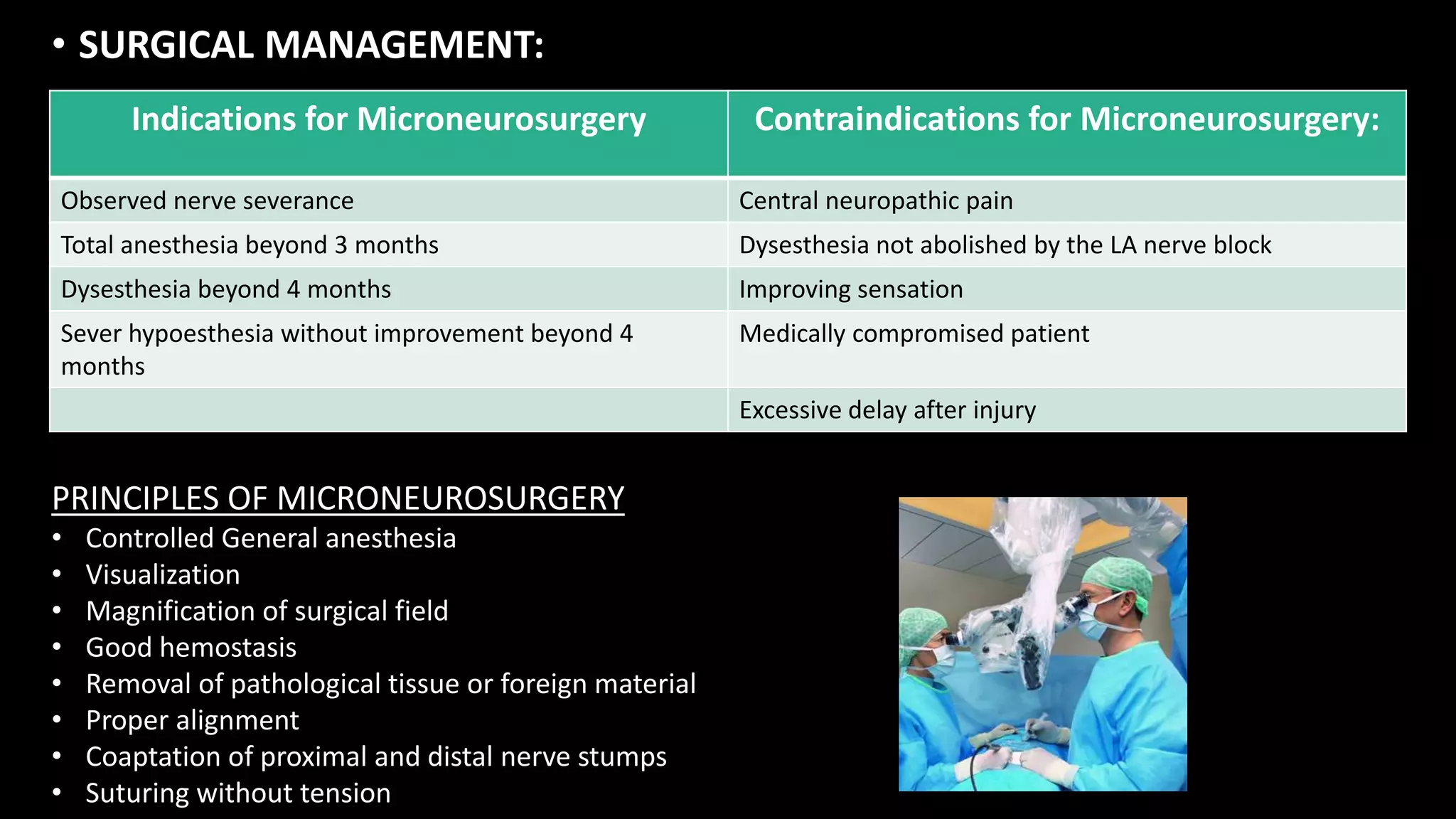
The document discusses the classification of nerve injuries, primarily focusing on traumatic causes and medical procedures leading to such injuries, categorized by Seddon's and Sunderland's classifications. It elaborates on symptoms, evaluation methods, and management strategies, including both medical and surgical interventions for different types of nerve damage. Post-operative protocols and nerve regeneration techniques, along with their implications on recovery, are also highlighted.