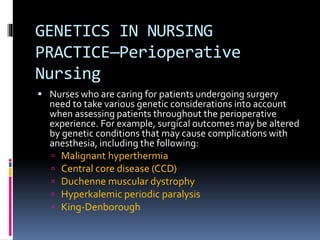
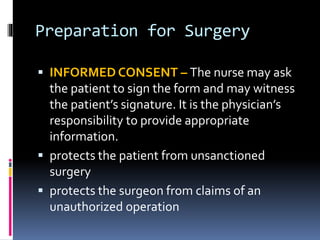
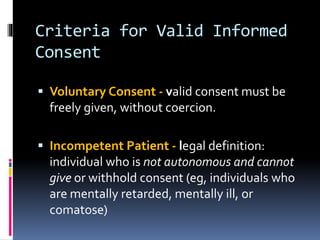
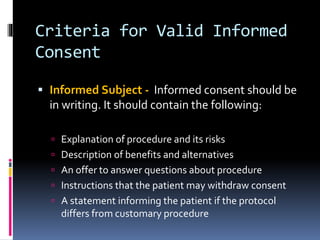
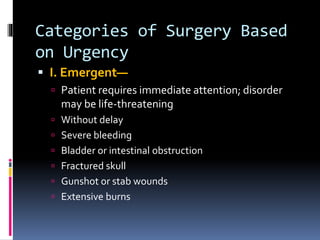
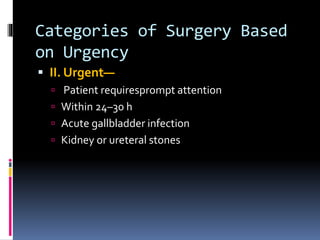
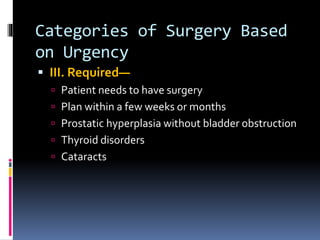
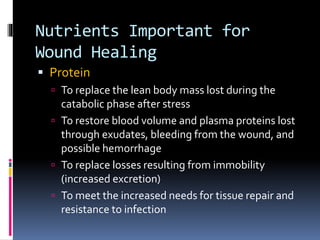
This document discusses key aspects of perioperative nursing, including definitions of preoperative, intraoperative, and postoperative phases. It outlines nursing roles and responsibilities in each phase, such as obtaining informed consent, preparing patients for surgery, monitoring patients in the operating room and PACU, and promoting recovery. Nutritional needs for wound healing and risk factors for surgical complications are also summarized.