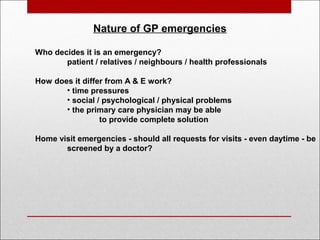
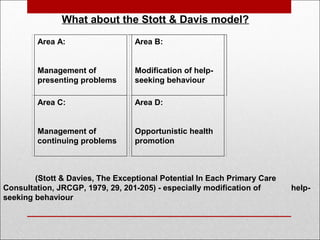
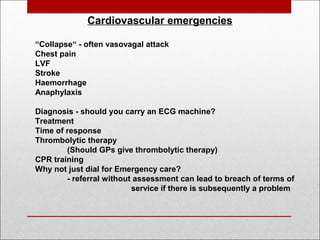
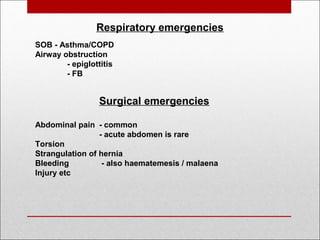
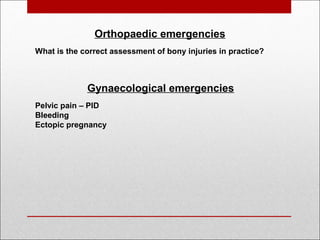
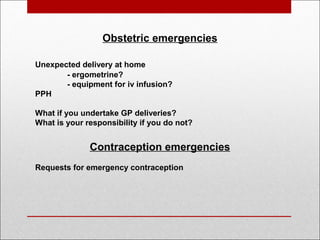
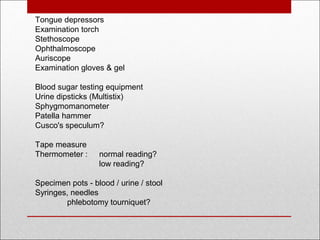
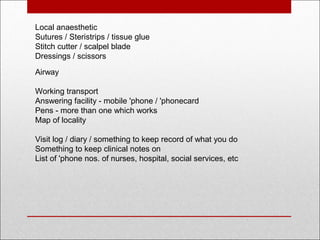
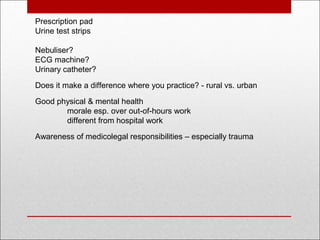
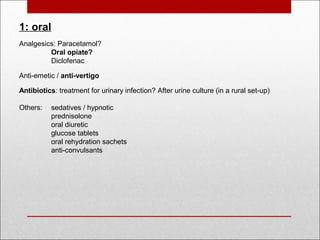
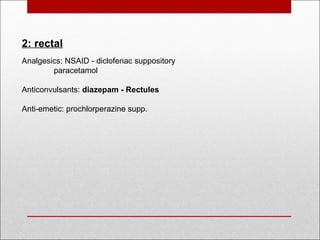
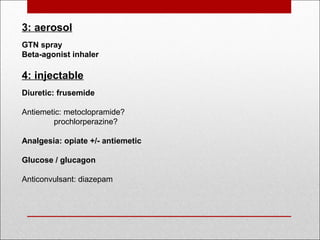
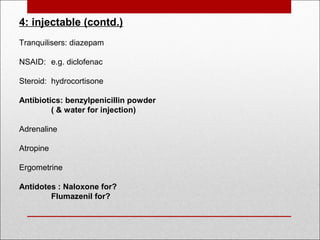
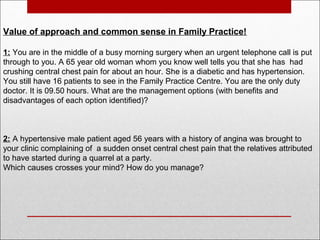
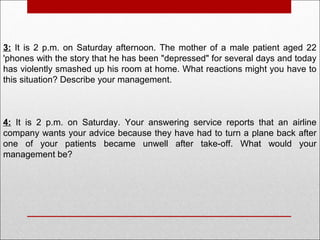
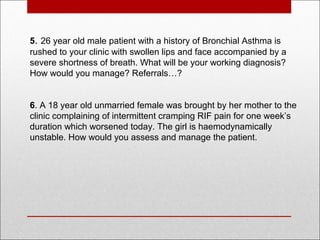
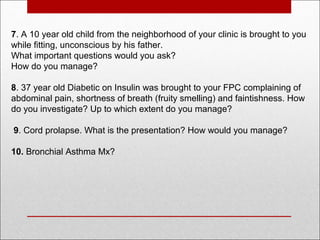
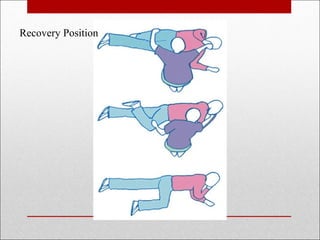
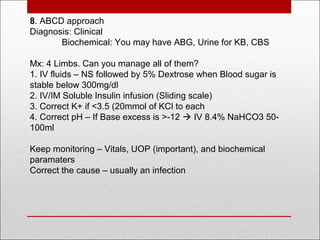
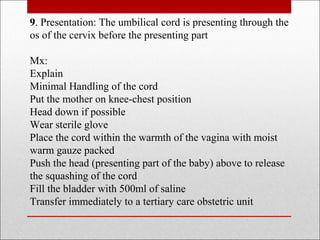
The document discusses various emergencies in general practice, detailing types of cases such as cardiovascular, respiratory, surgical, and psychological emergencies, along with management strategies and necessary equipment for primary care physicians. It emphasizes the distinction between emergency response in general practice compared to hospital settings, including the importance of initial assessment and potential interventions. The document also outlines essential drugs and procedures for managing different emergencies, stakeholder responsibilities, and the necessity of effective communication in urgent situations.