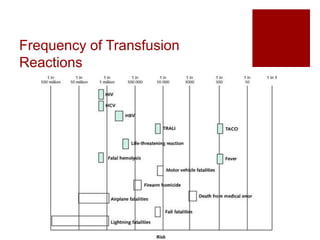
This document discusses several common transfusion reactions including febrile nonhemolytic reactions, delayed hemolytic reactions, acute hemolytic reactions, transfusion-associated circulatory overload (TACO), transfusion-related acute lung injury (TRALI), and allergic reactions/anaphylaxis. It provides details on the presentation, diagnosis, treatment, and prevention of each reaction through several case examples of a patient named Mr. Red who experiences different reactions over the years as he requires multiple blood transfusions. The key message is that it is important for healthcare providers to recognize potential transfusion reactions so they can stop the transfusion if needed and assess the patient's condition, as some reactions may become life-threatening.