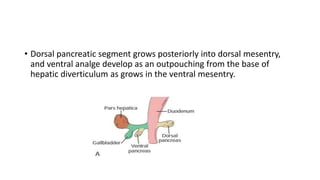
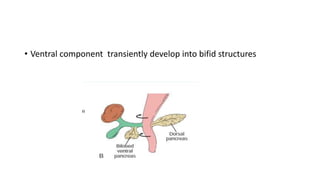
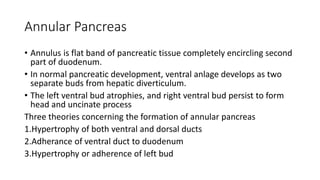
The pancreas develops from endoderm of the primitive duodenum in two parts - a dorsal and ventral part. The dorsal part forms the body, tail, and part of the head, while the right ventral bud persists to form the head and uncinate process.
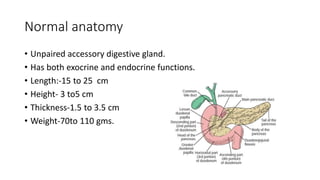
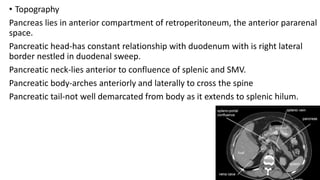
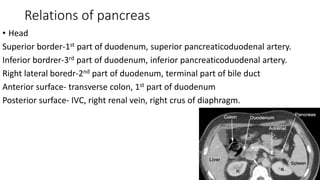
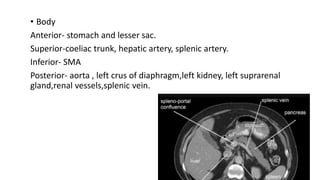
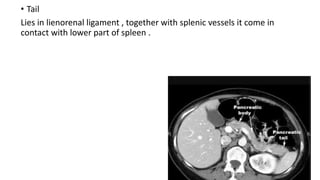
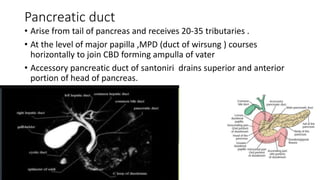
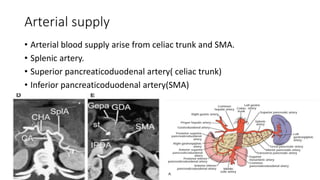
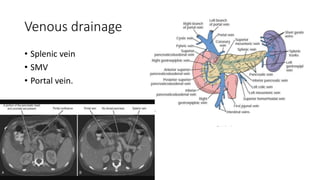
The pancreas has both exocrine and endocrine functions. It is located in the retroperitoneum with the head adjacent to the duodenum. The pancreatic duct arises in the tail and drains into the ampulla of Vater after joining the common bile duct. Arterial blood supply comes from the celiac trunk and SMA, while venous drainage is via the splenic and portal veins.
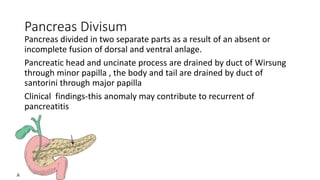
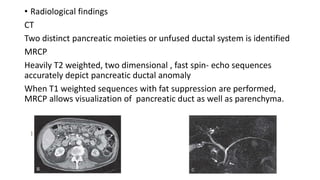
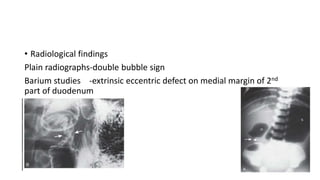
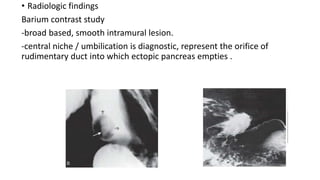
Congenital anomalies include