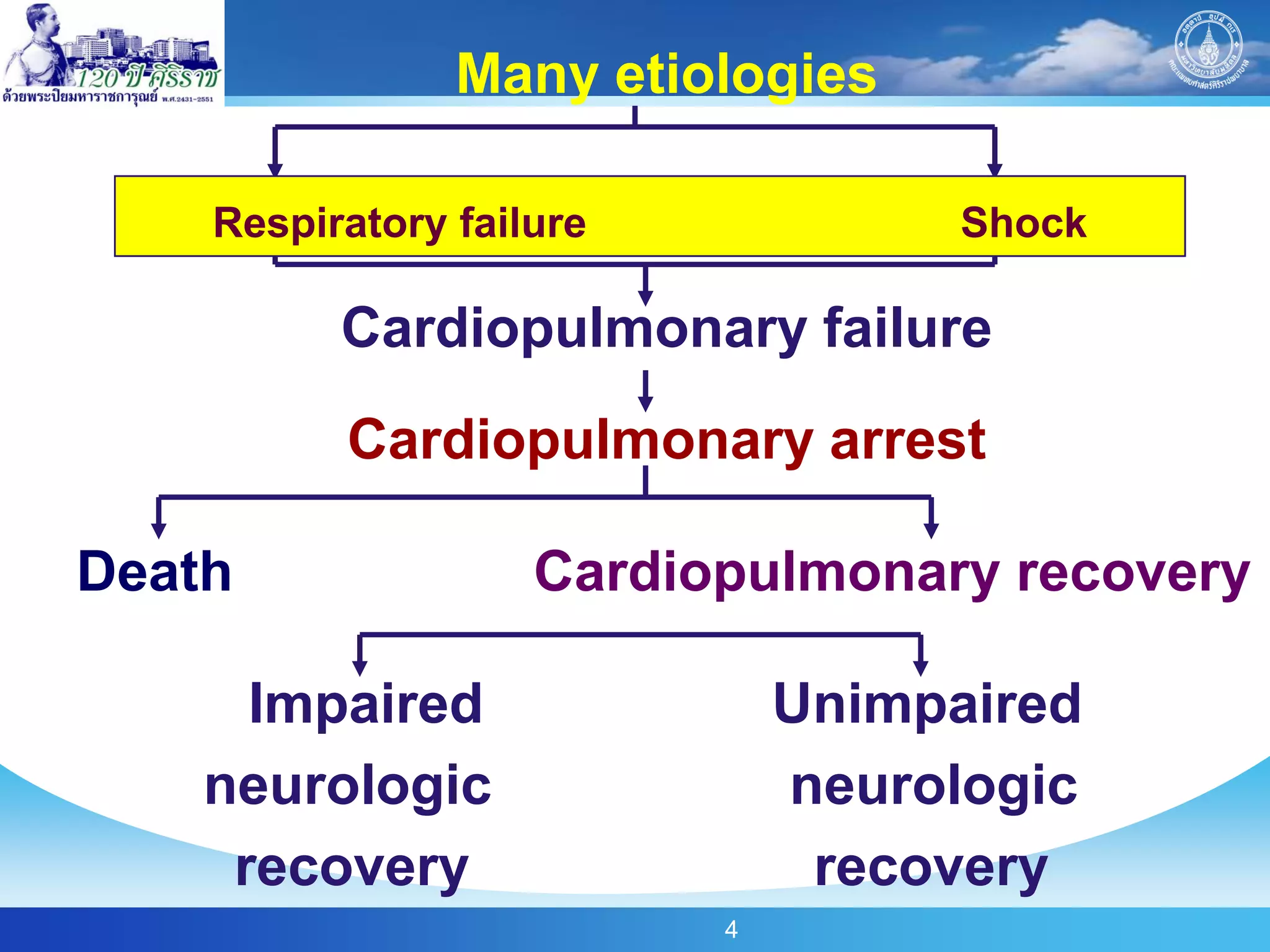
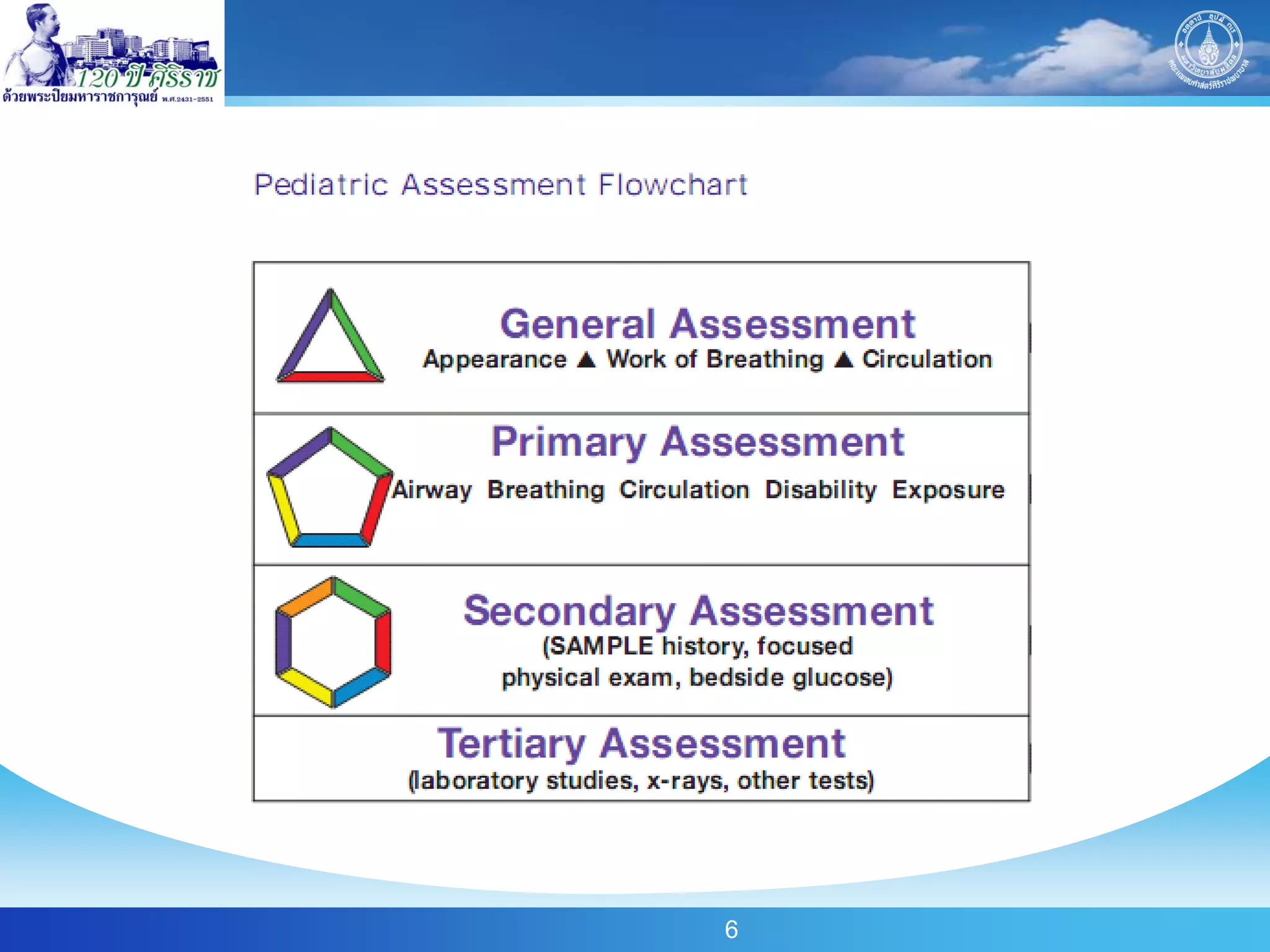
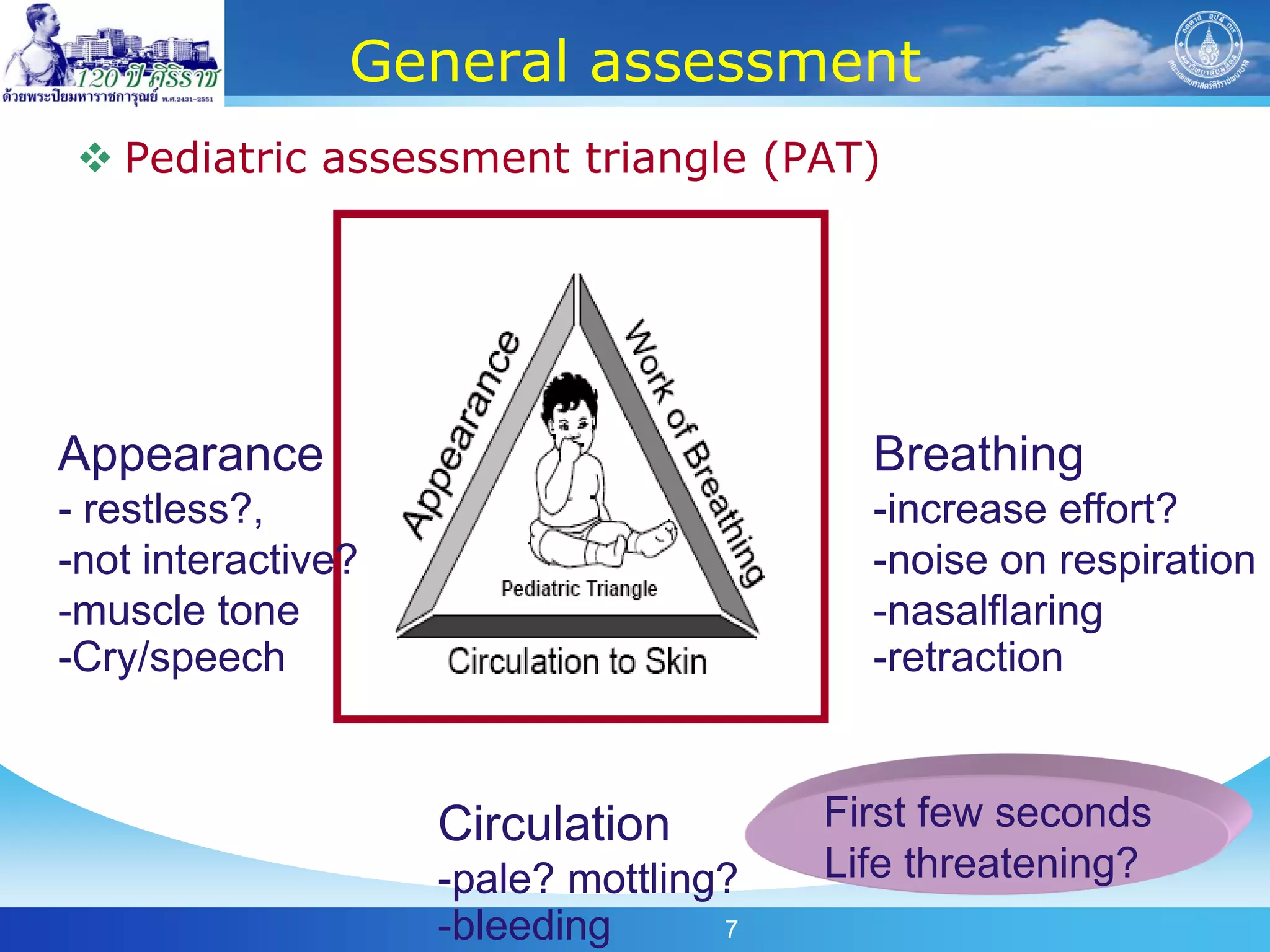
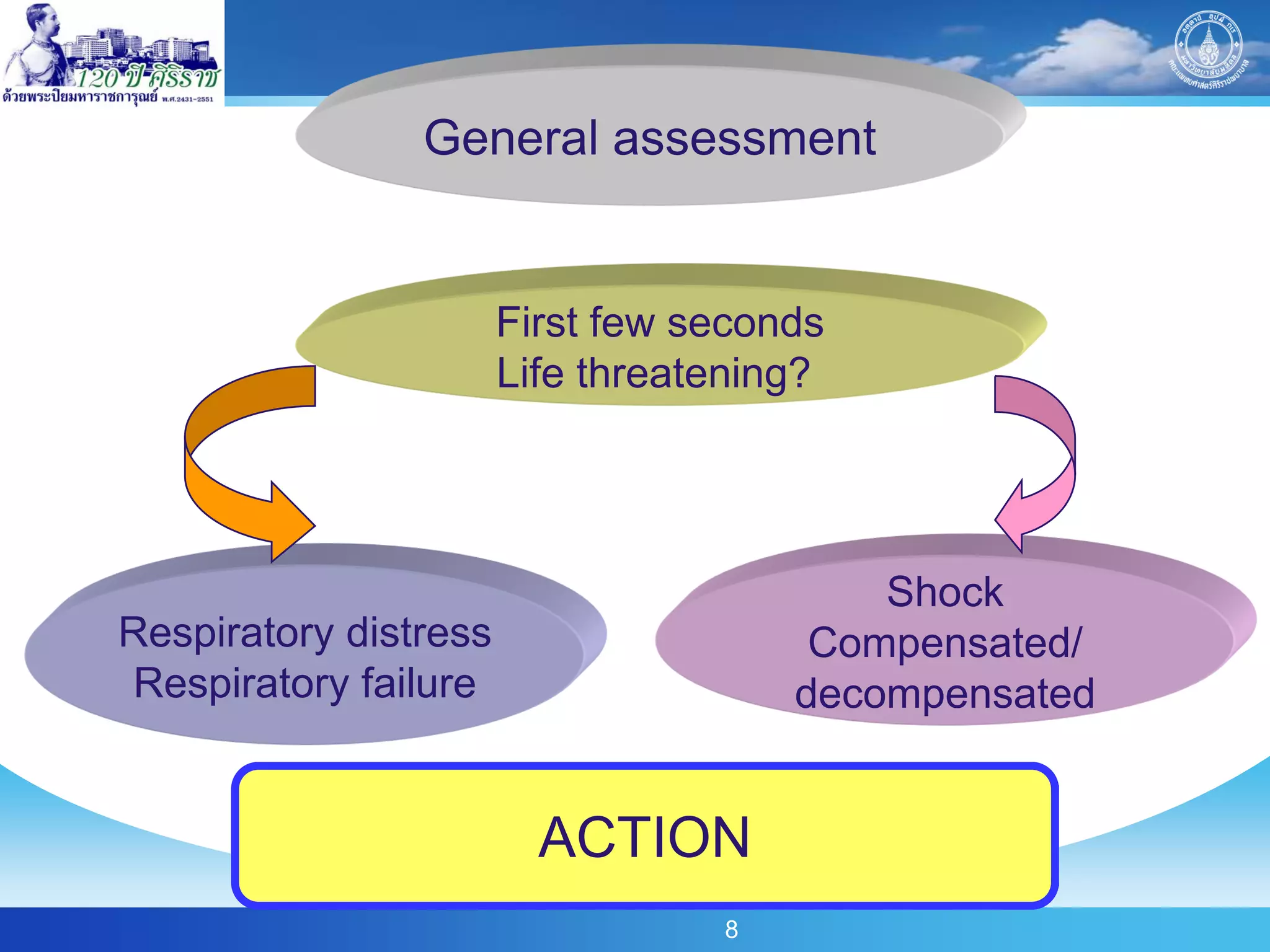
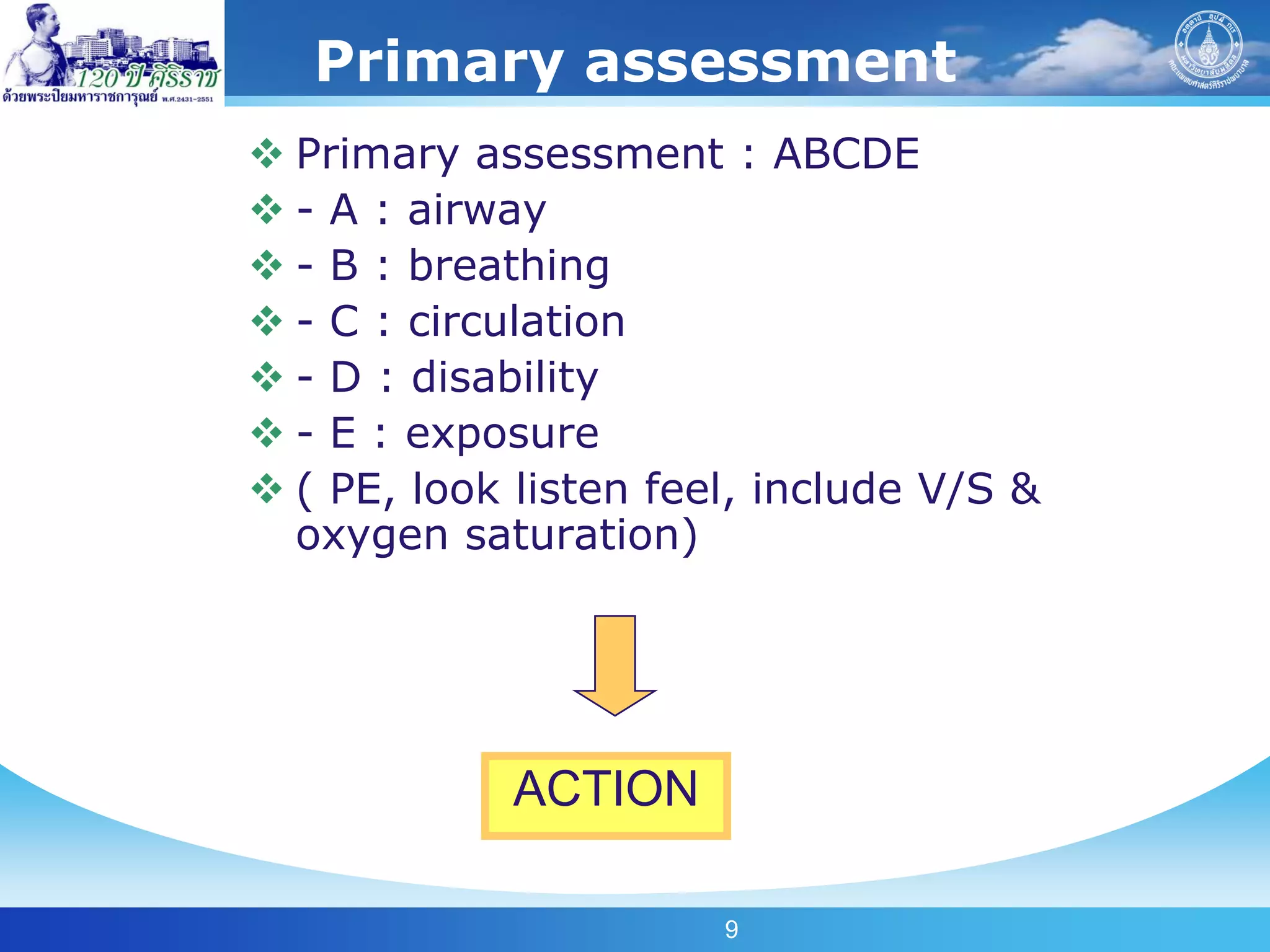
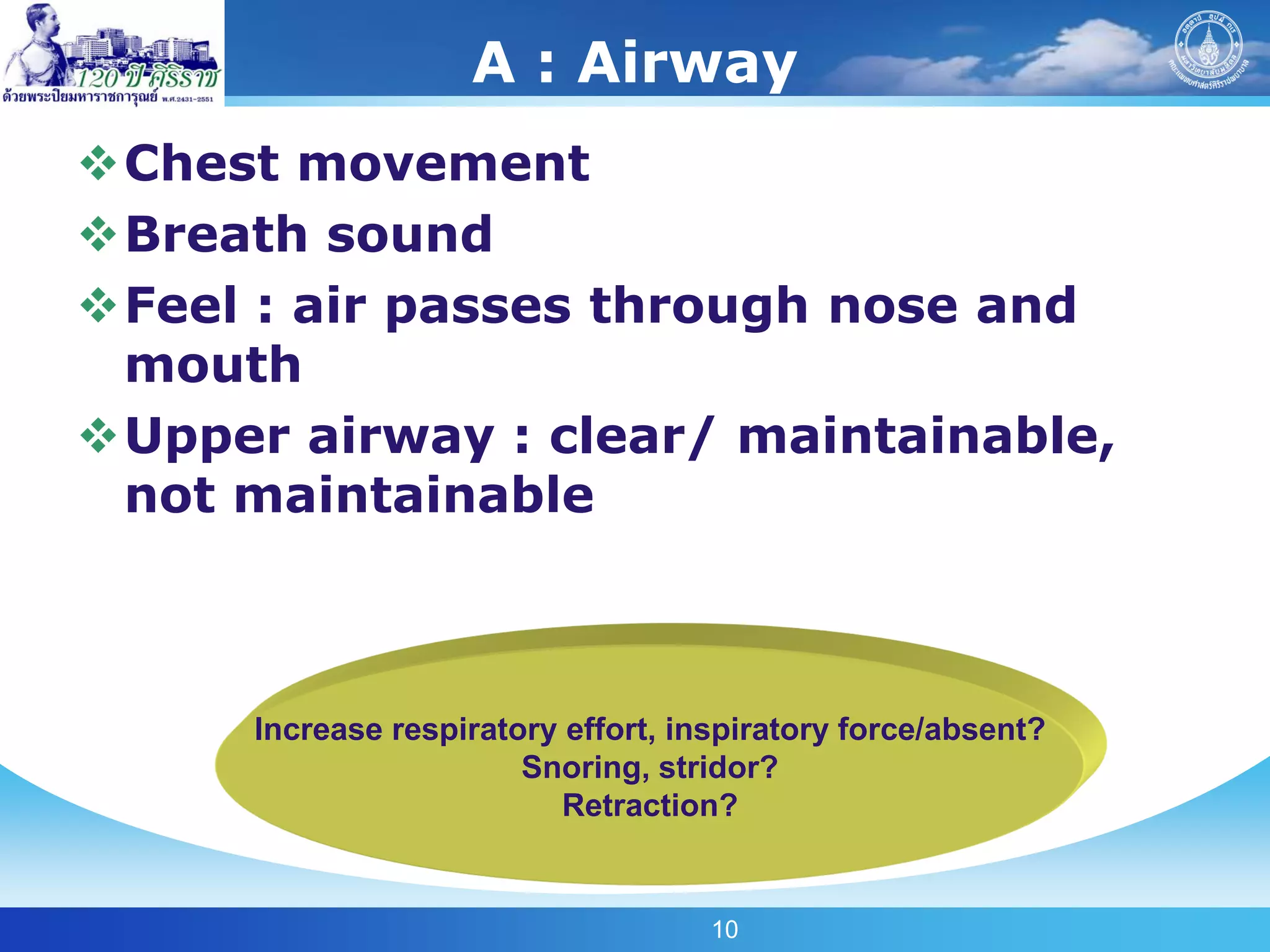
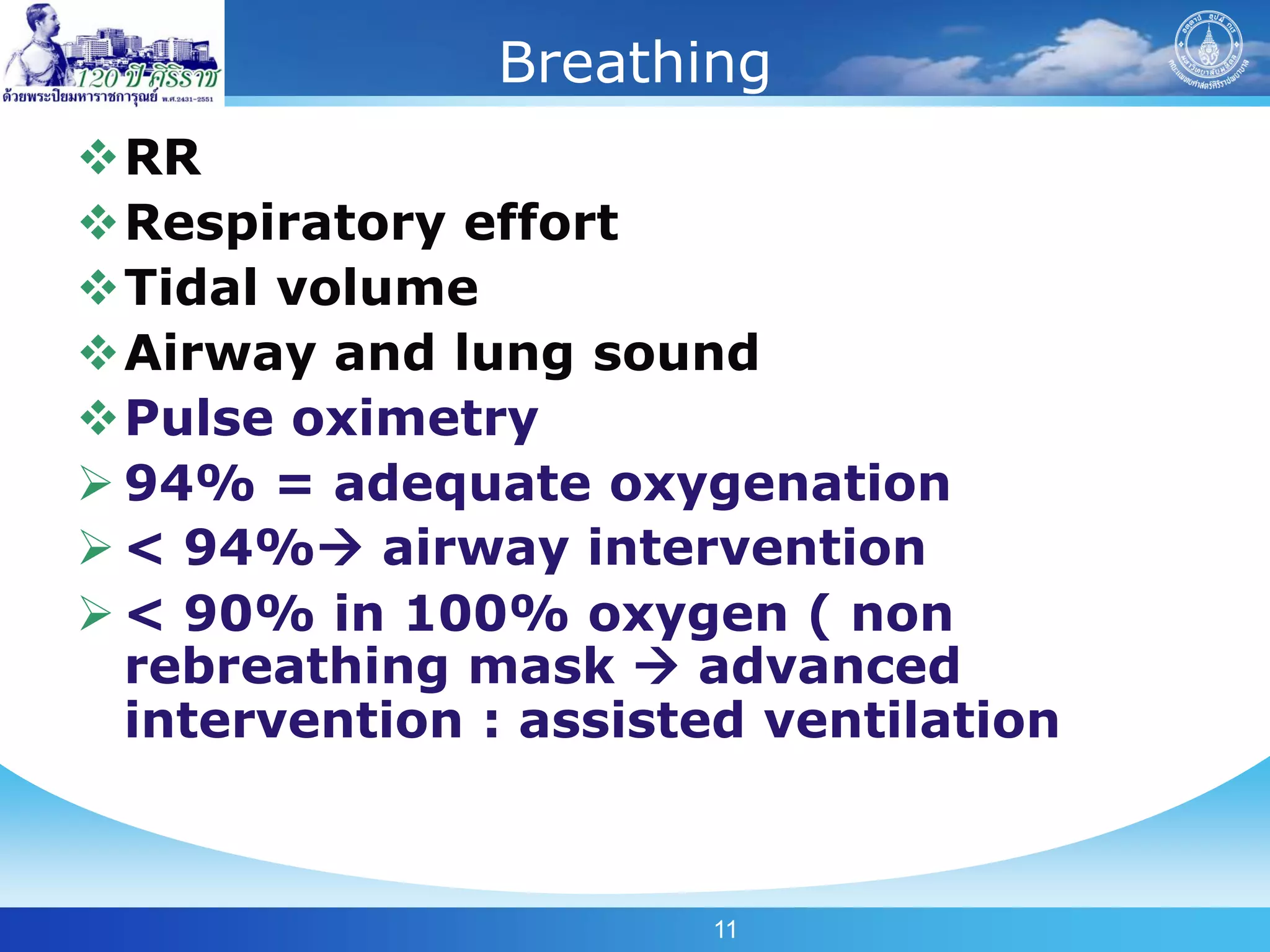
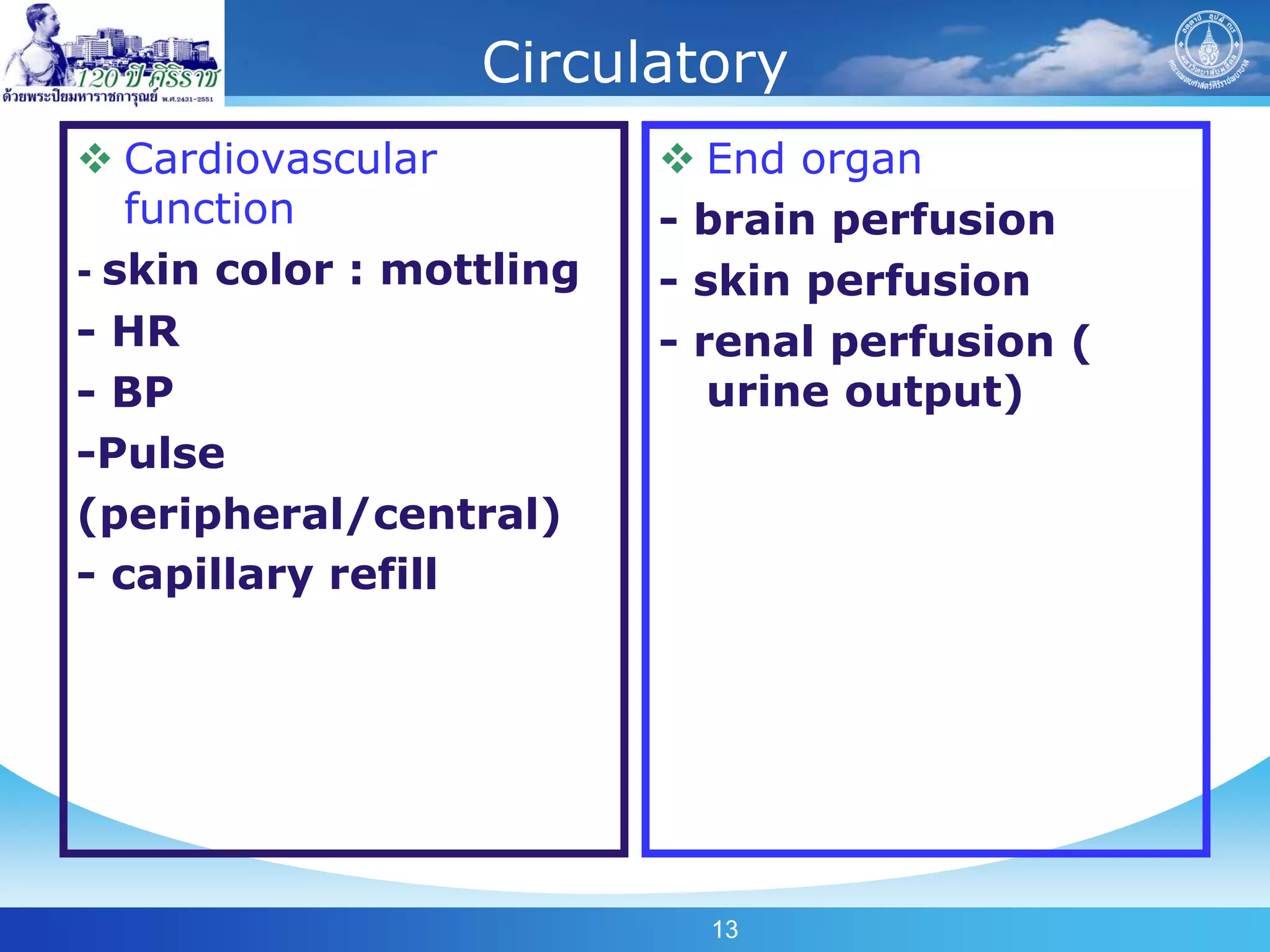
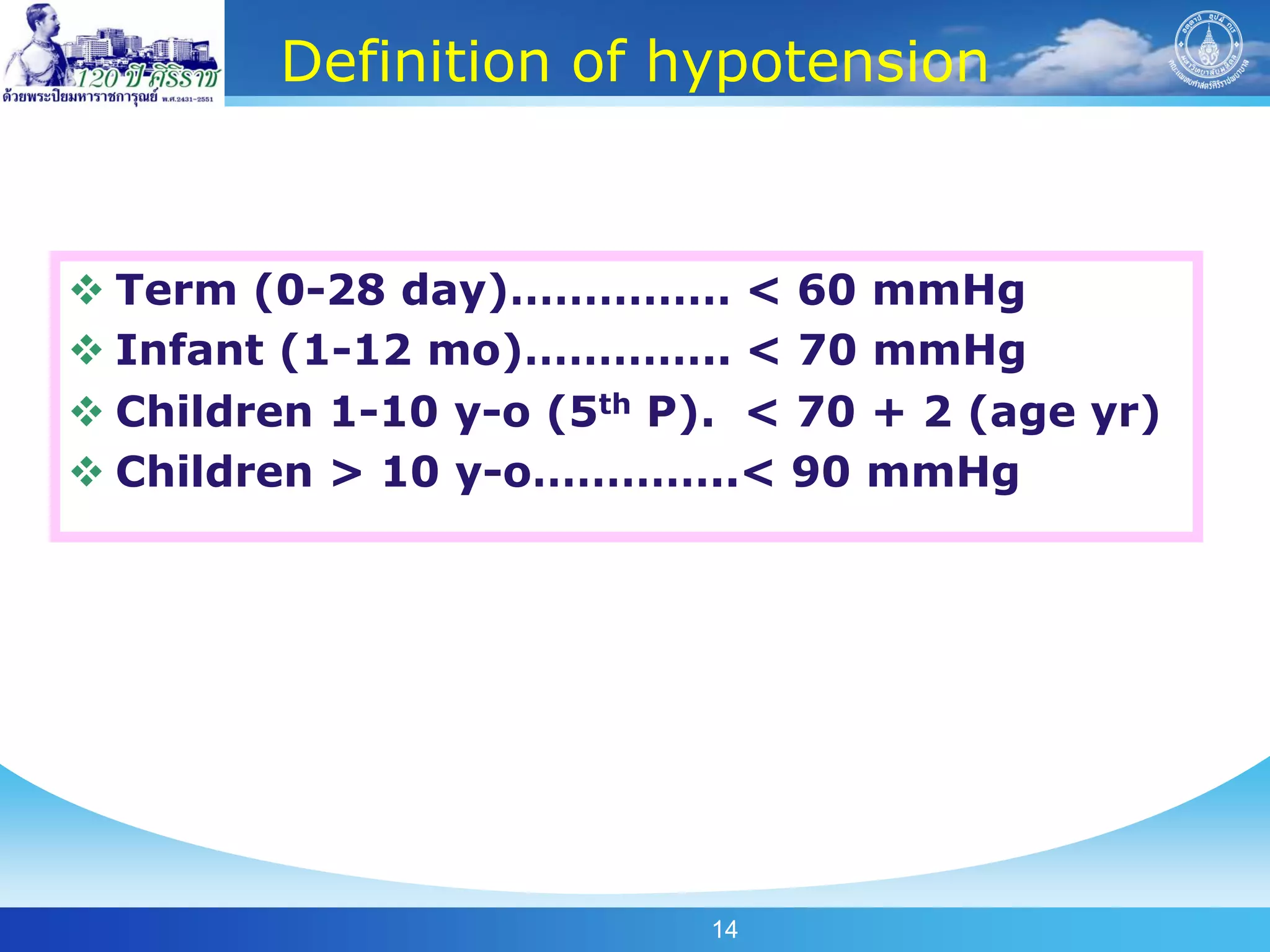
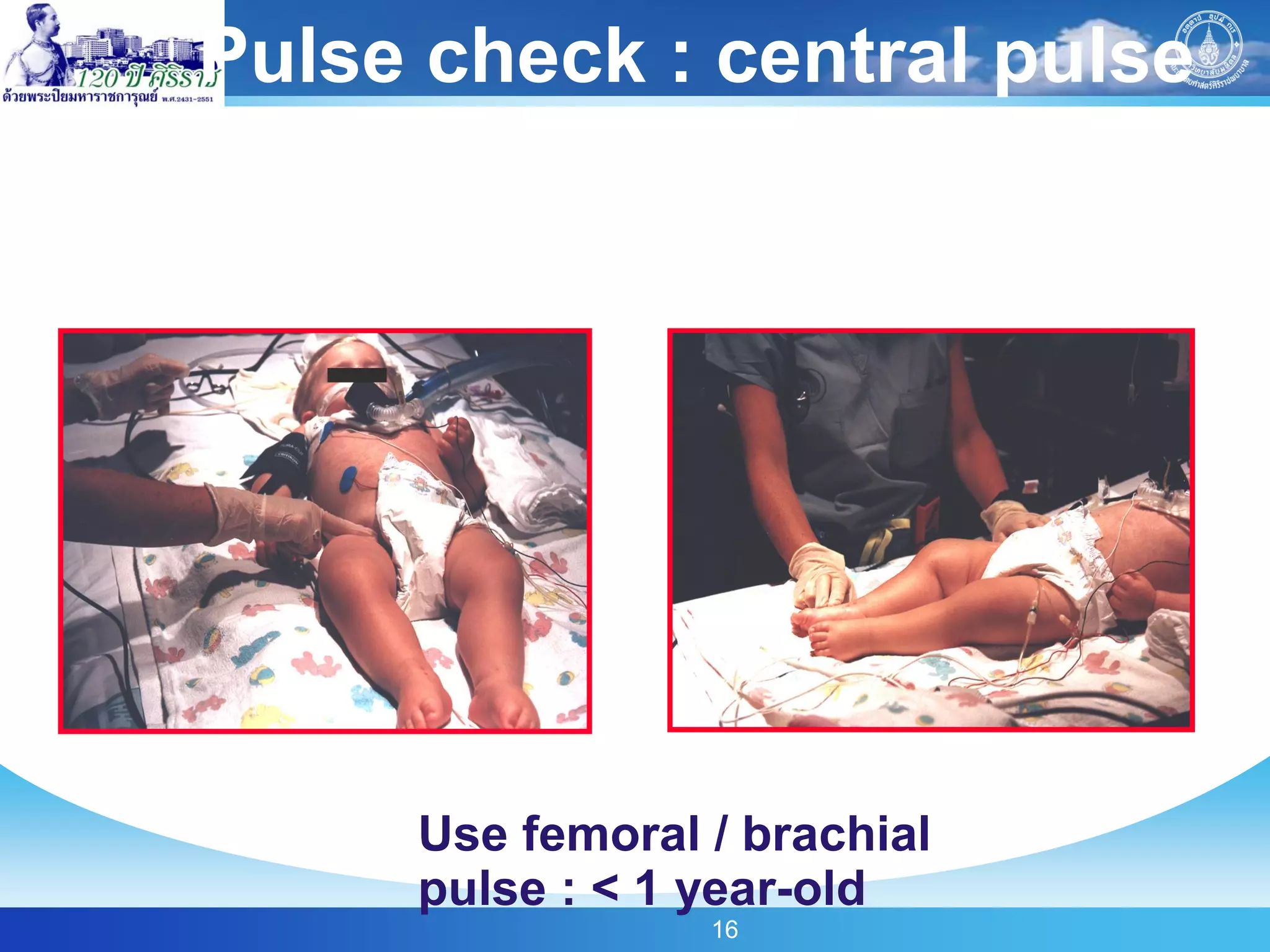
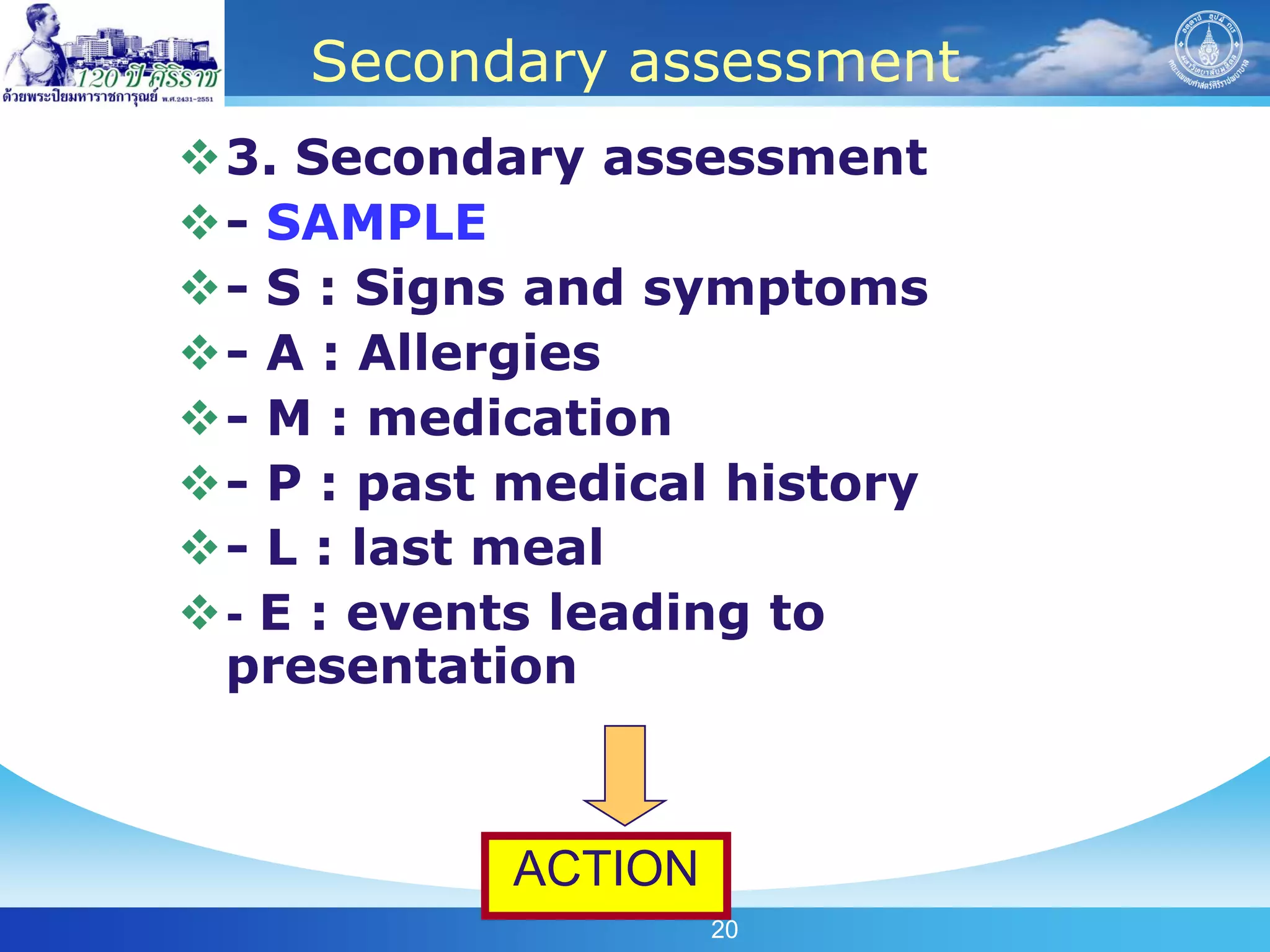
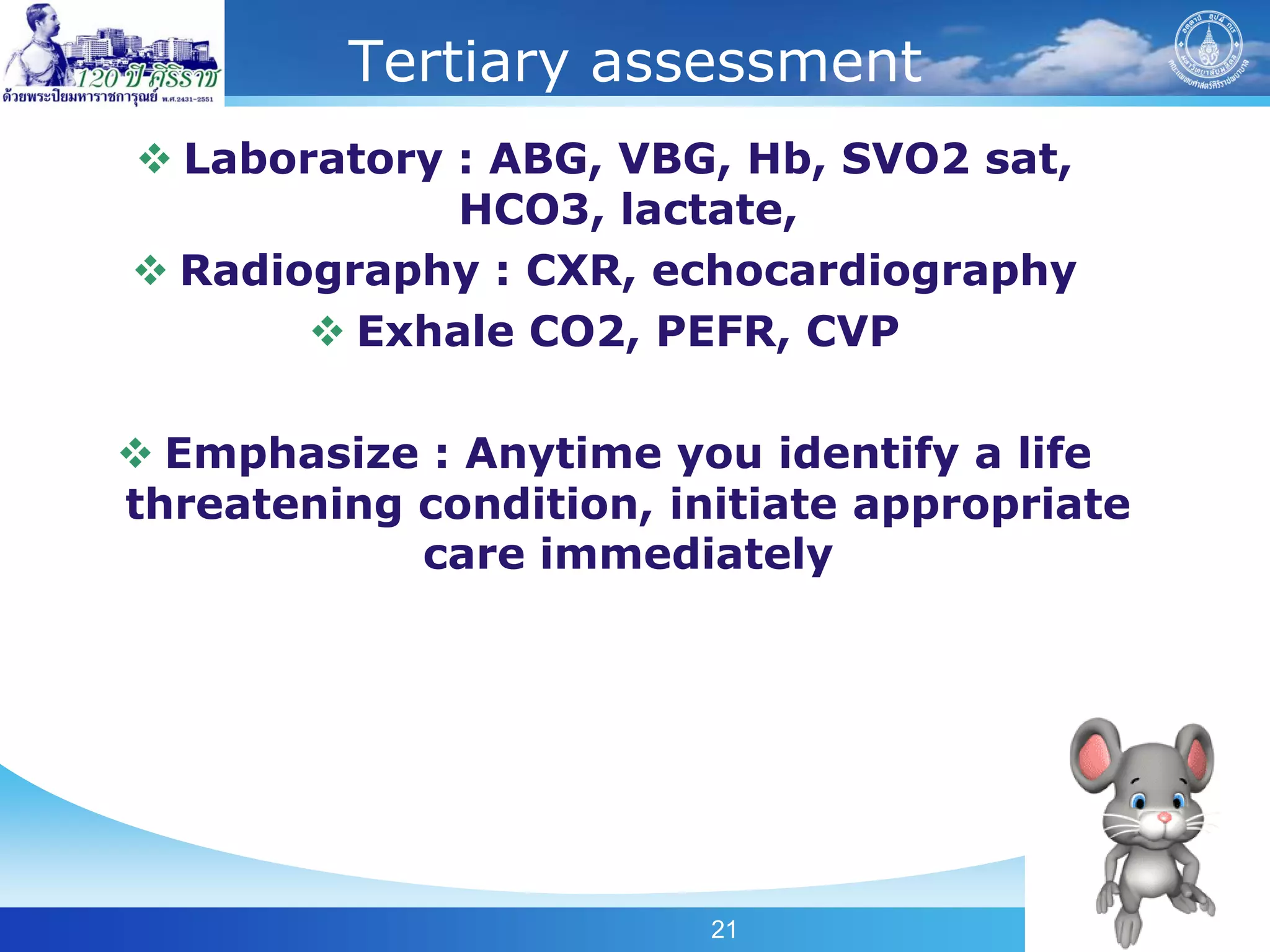
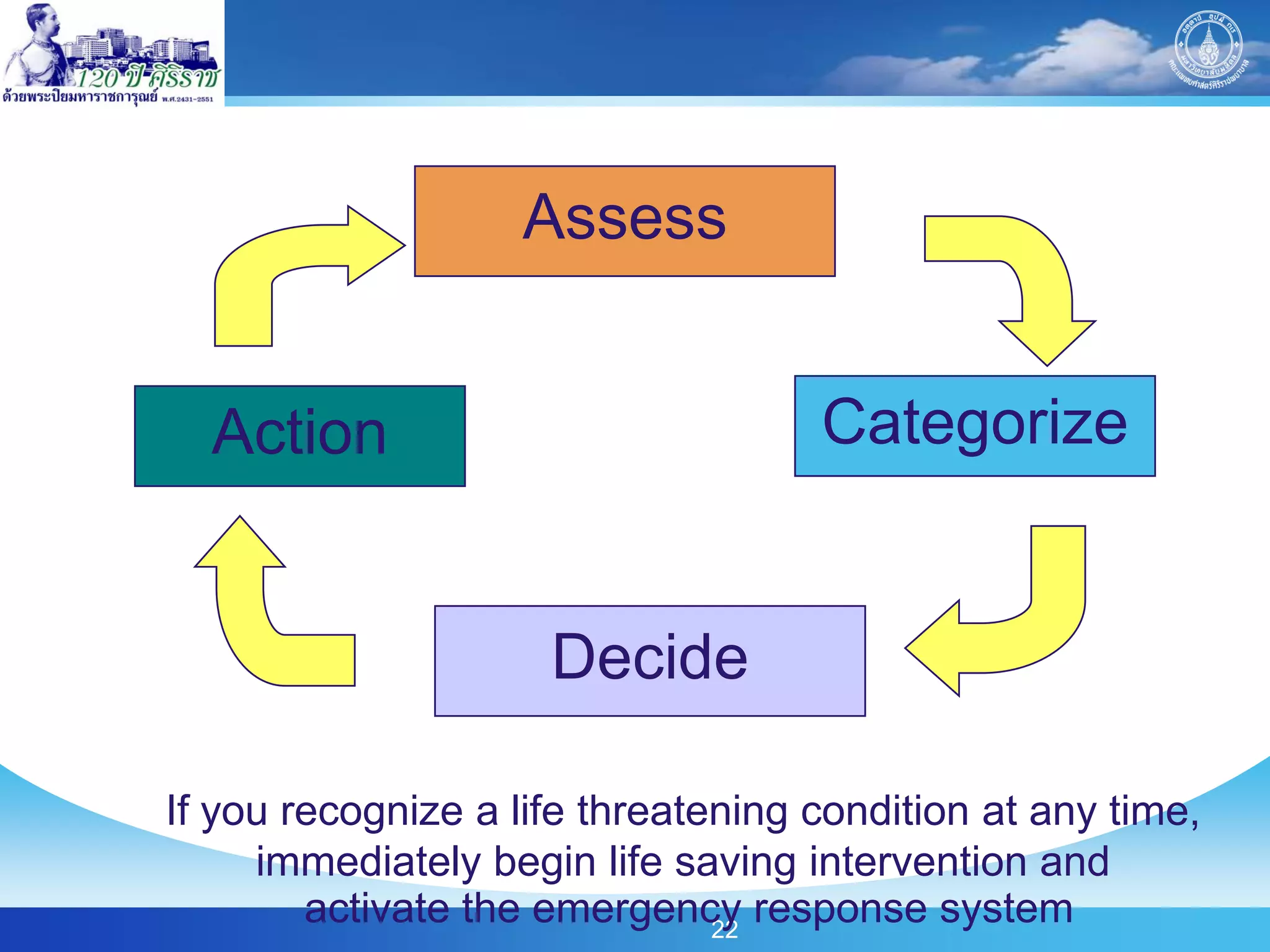
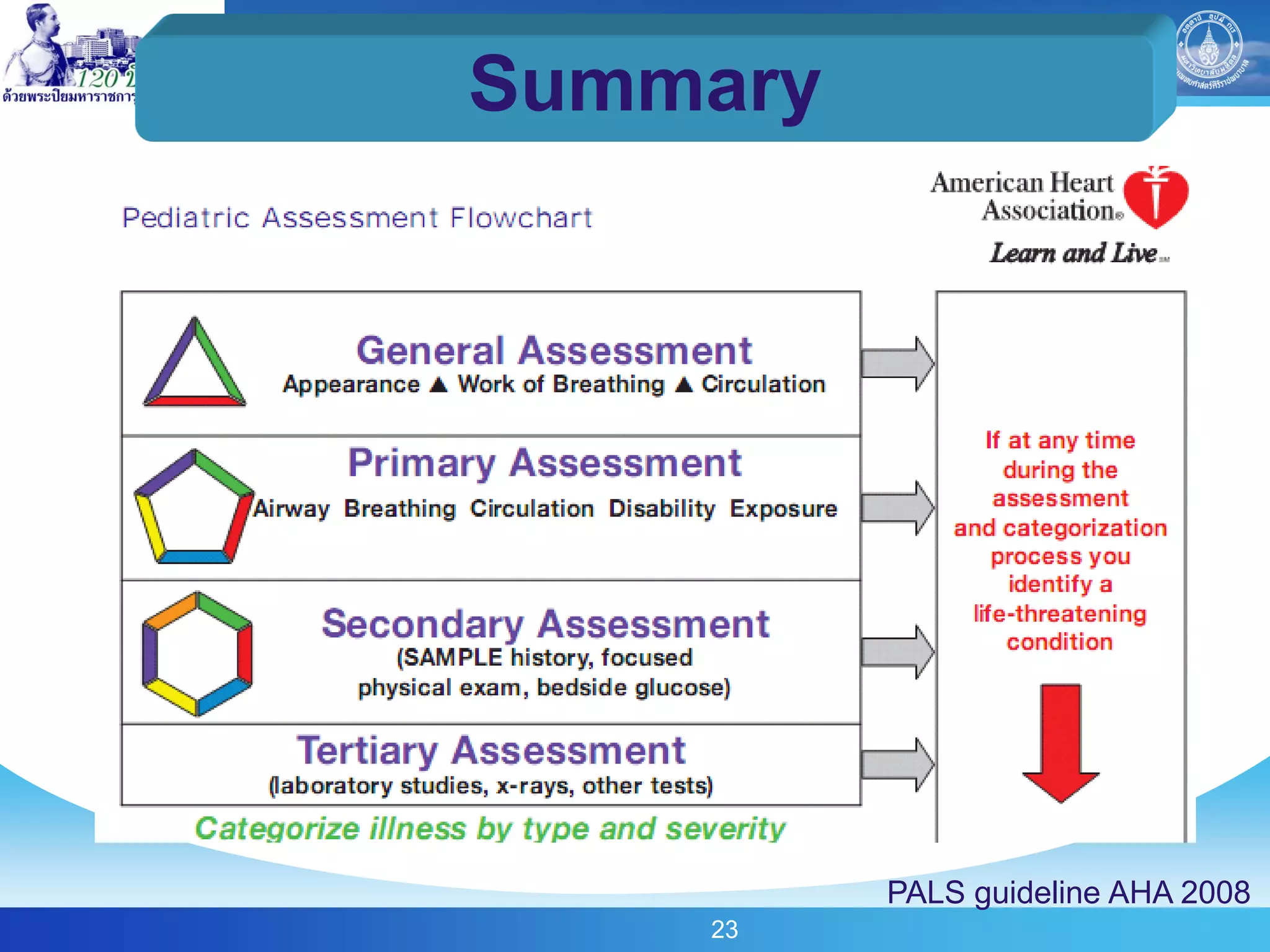
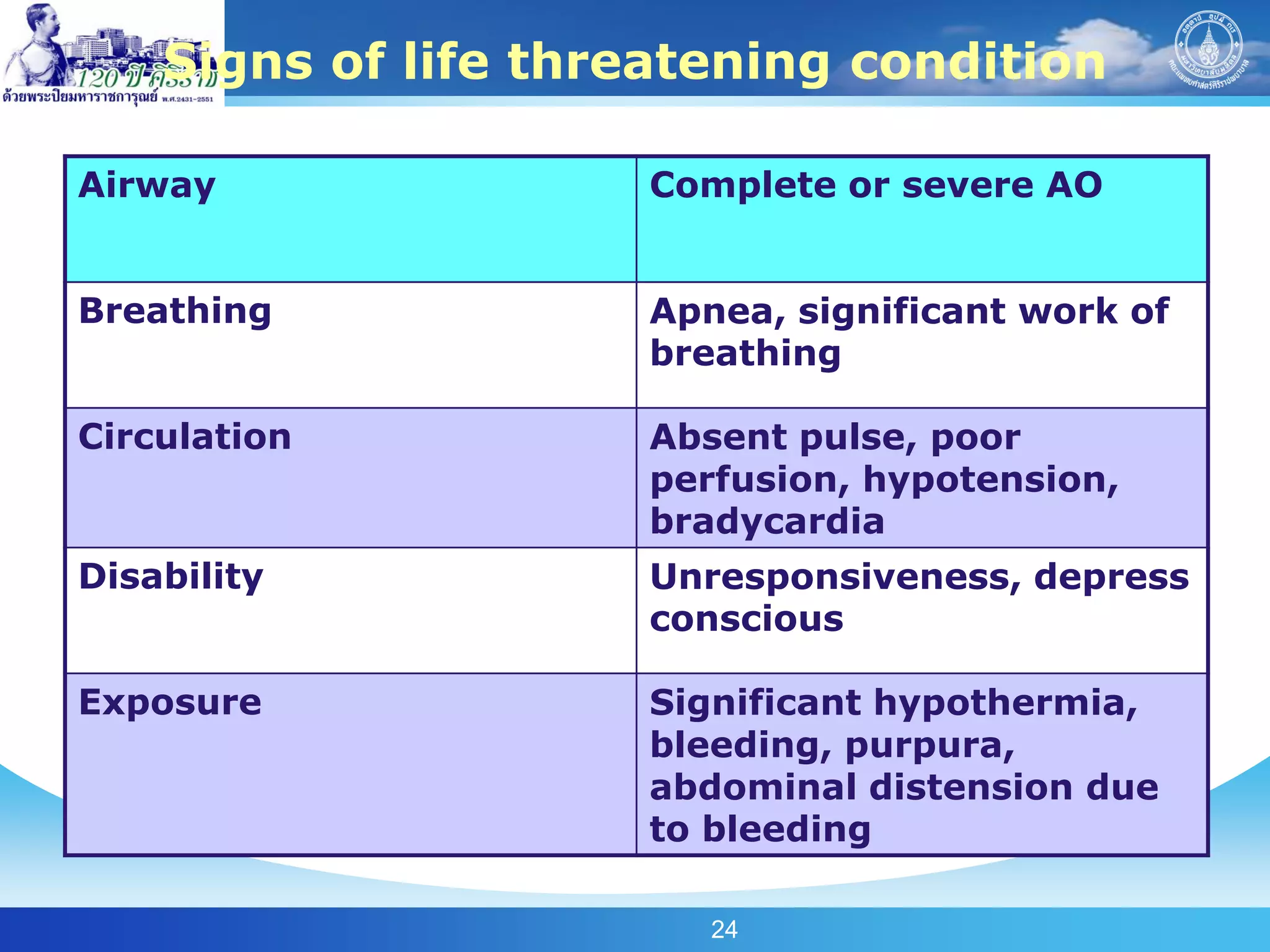
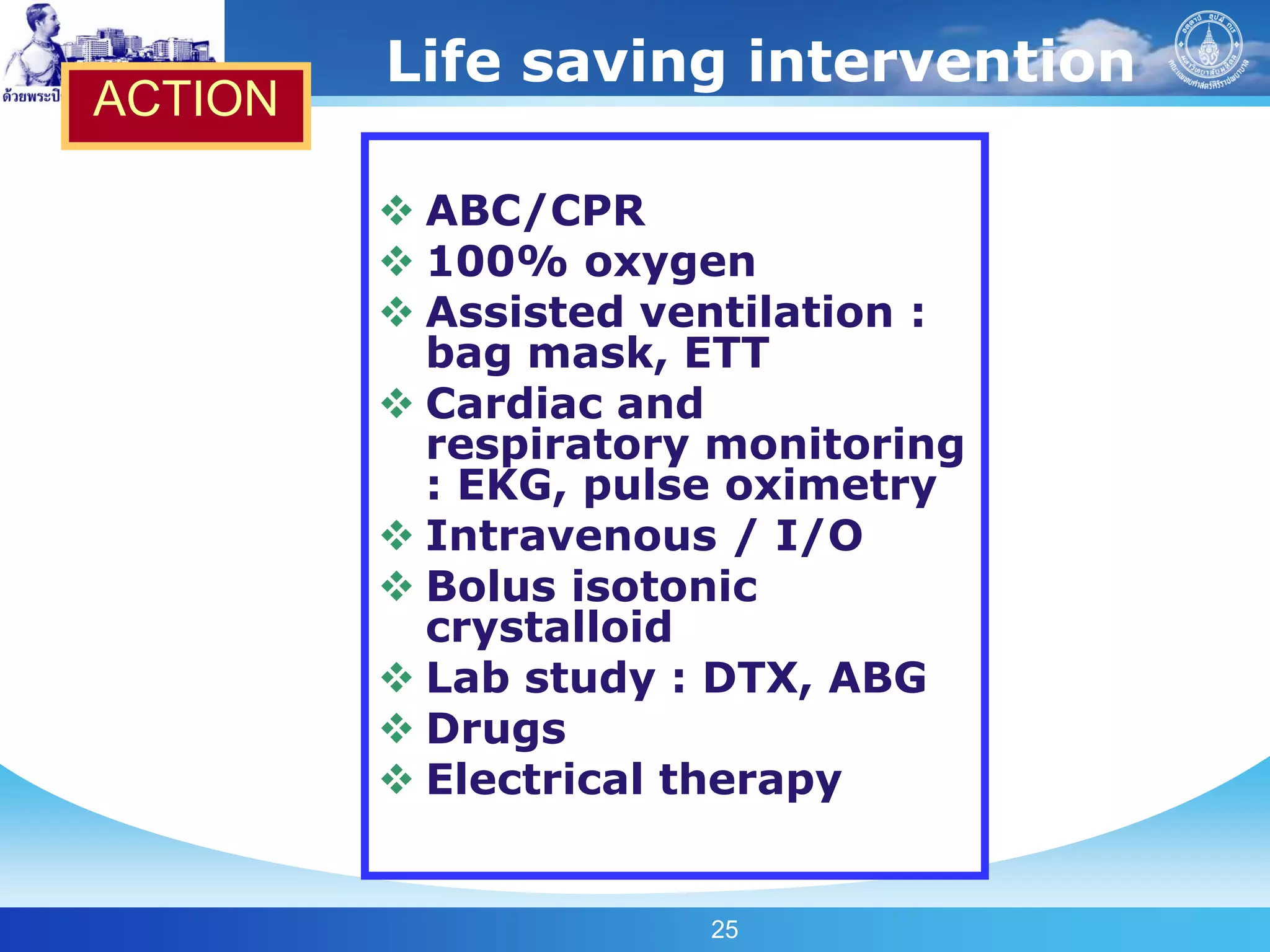
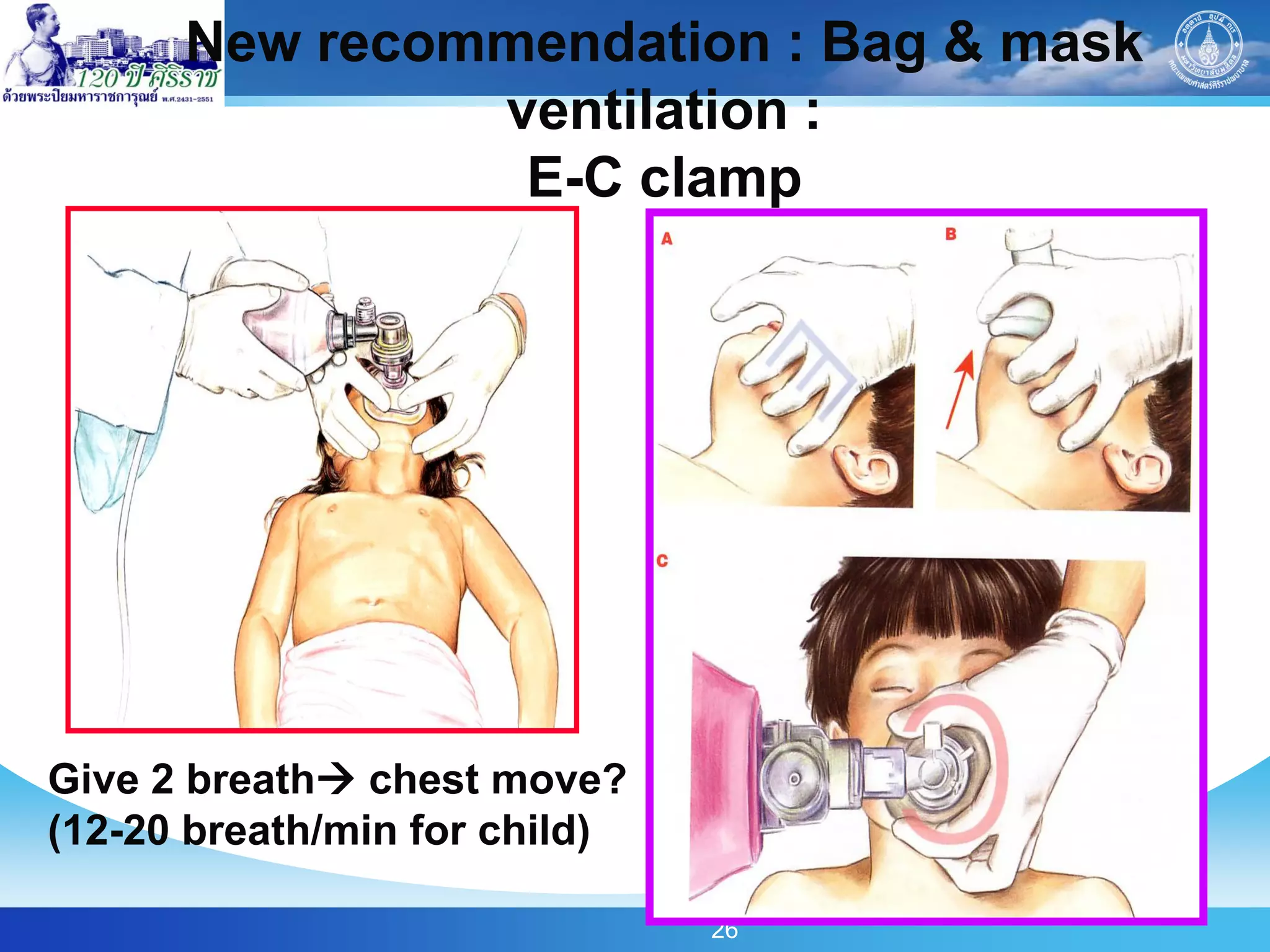
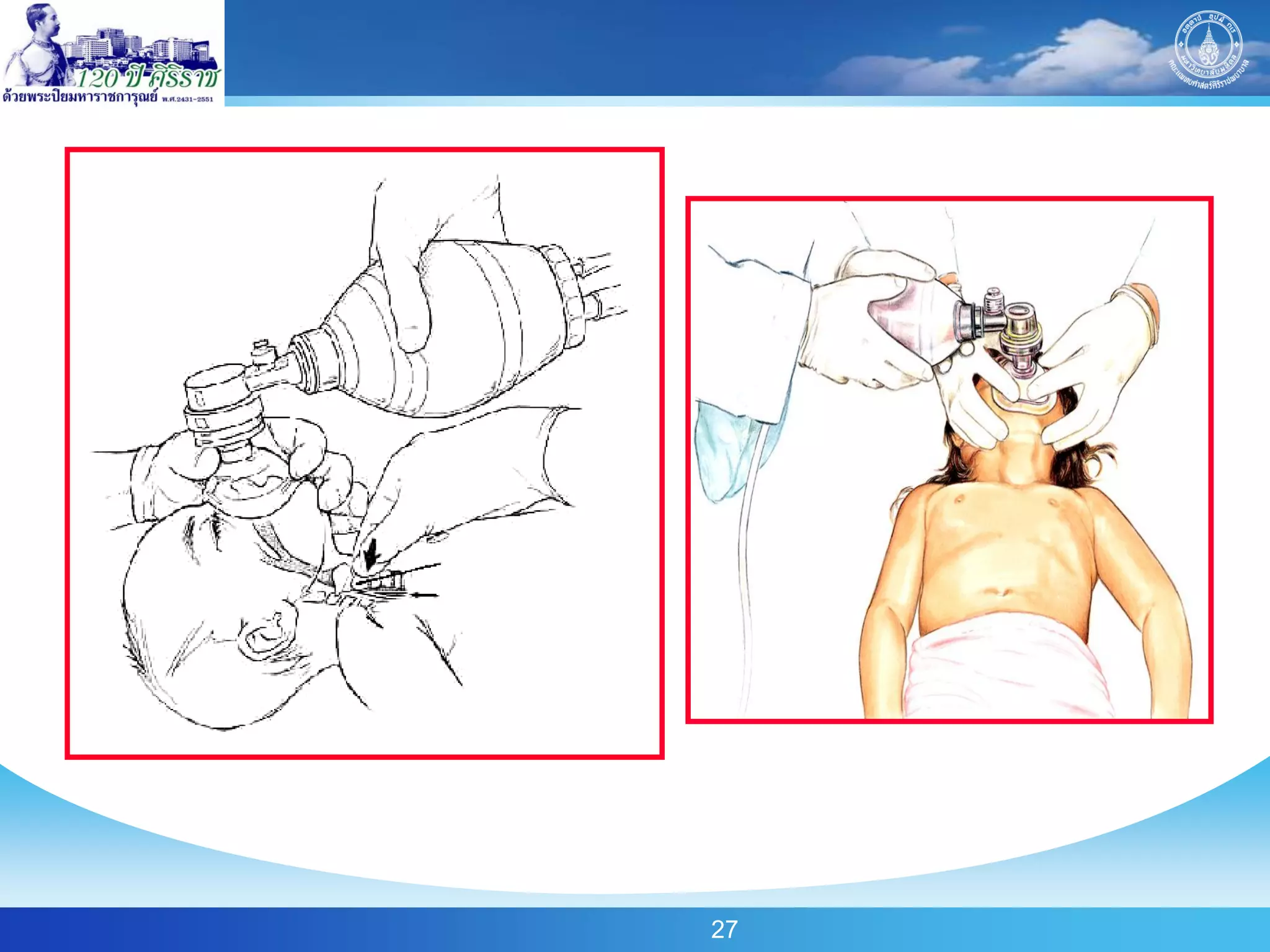
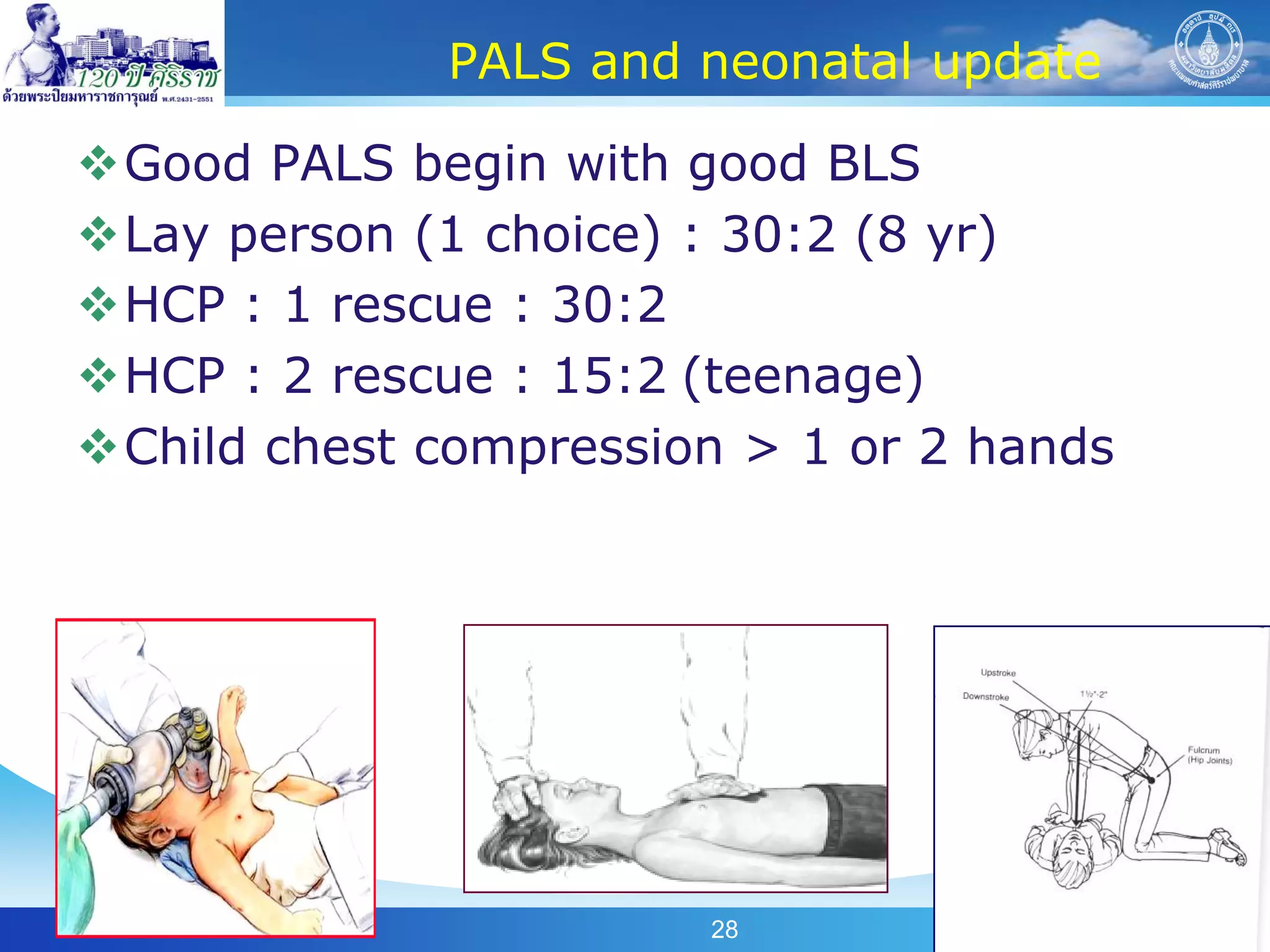
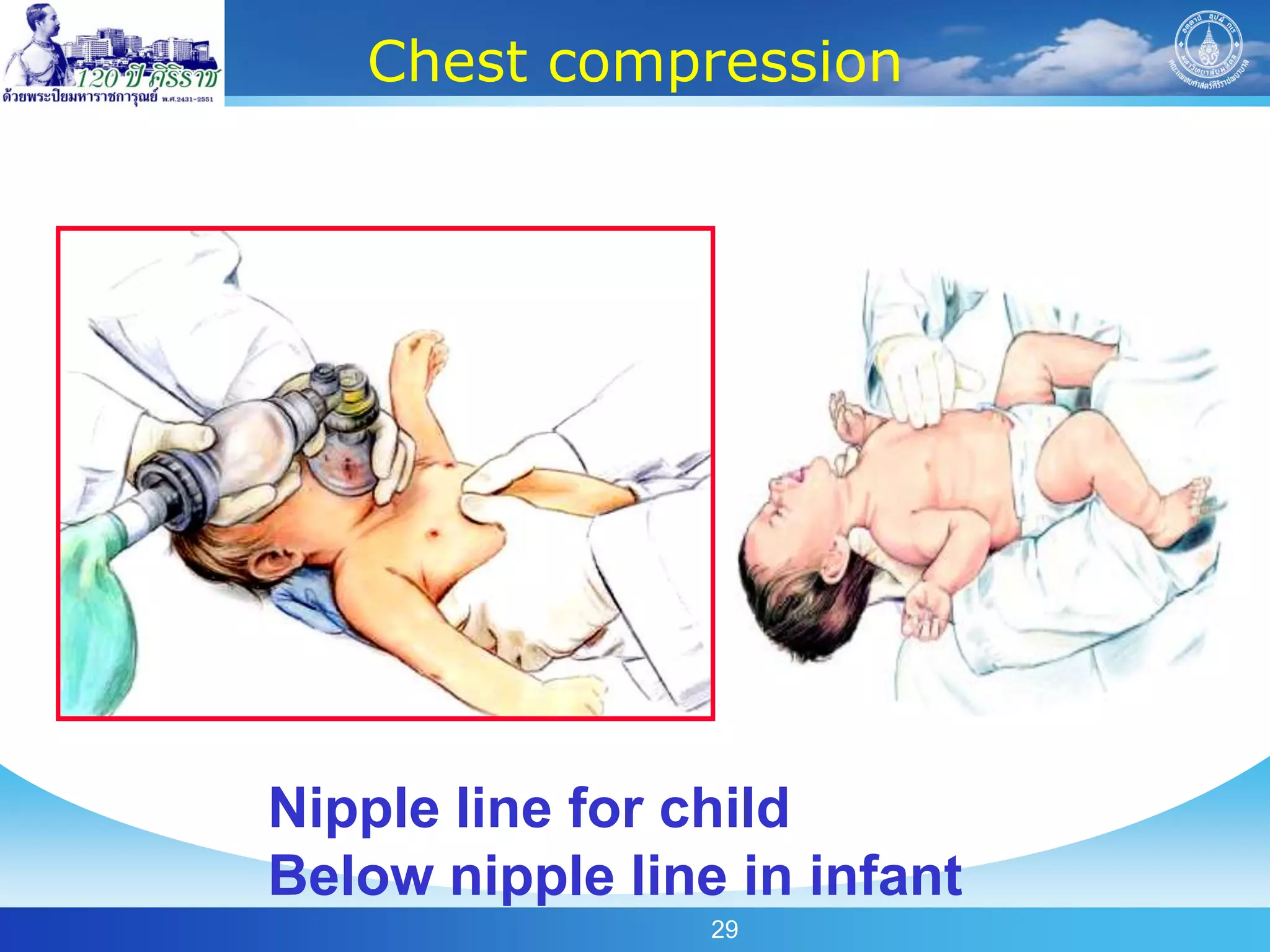
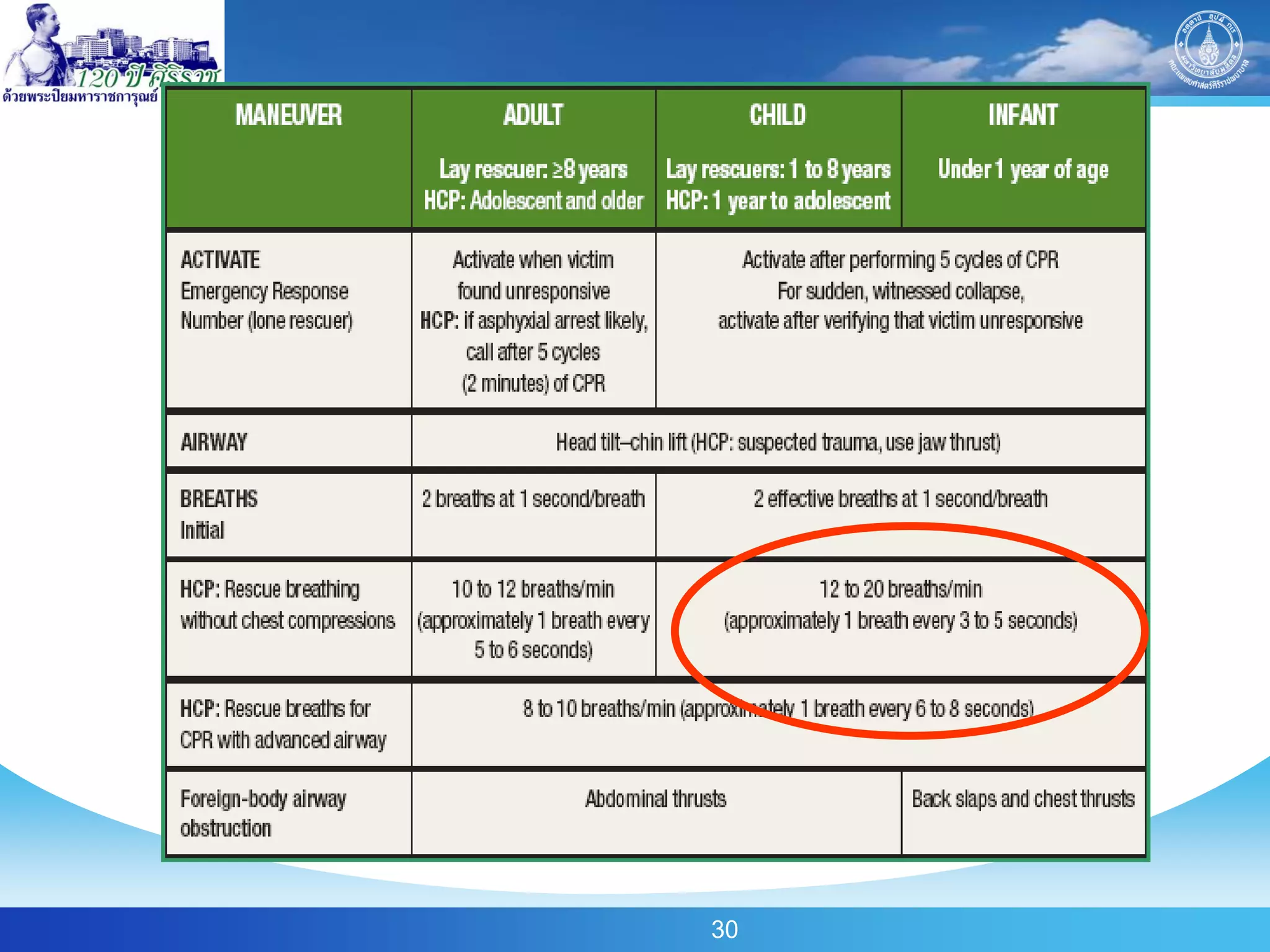
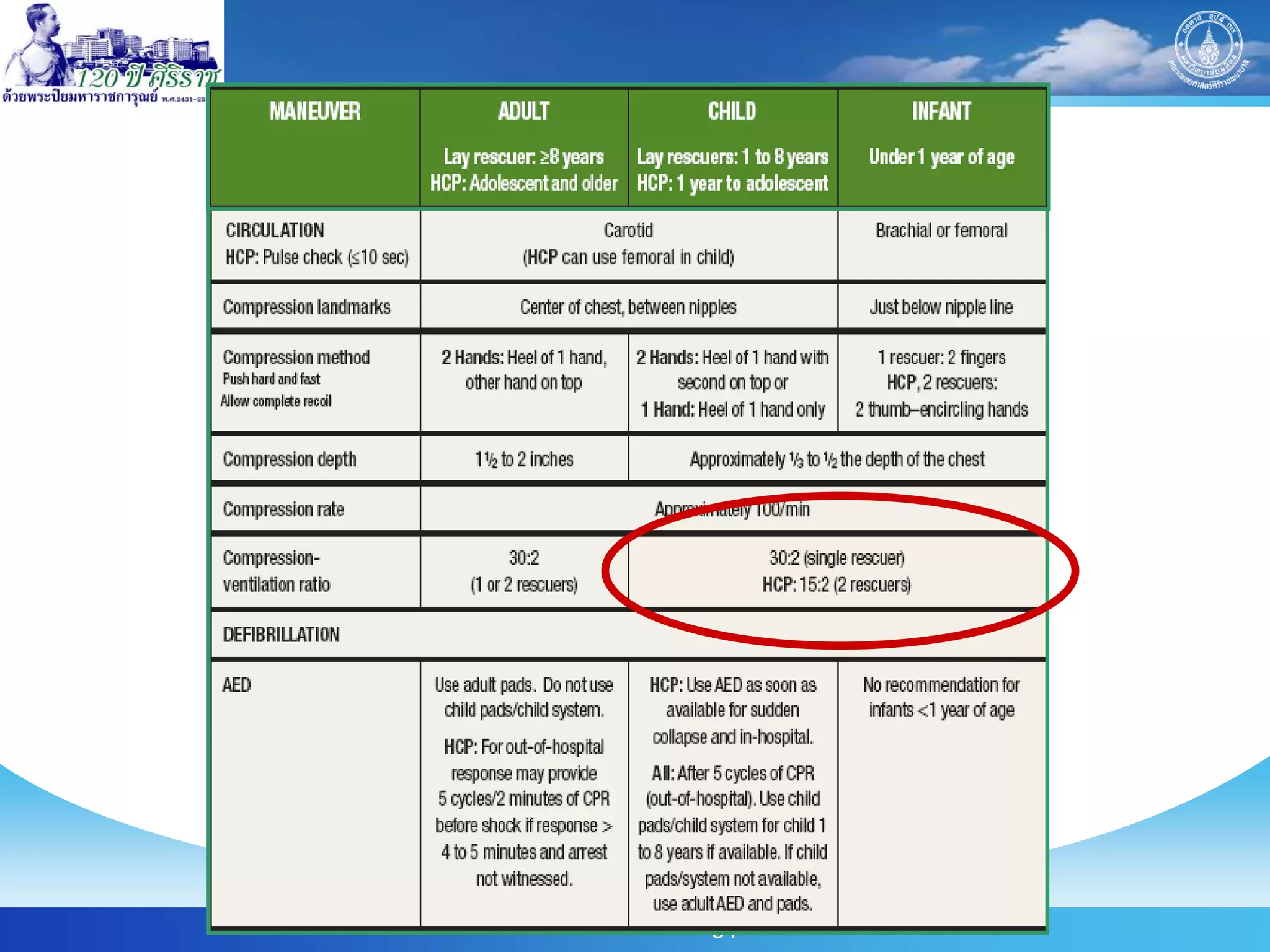
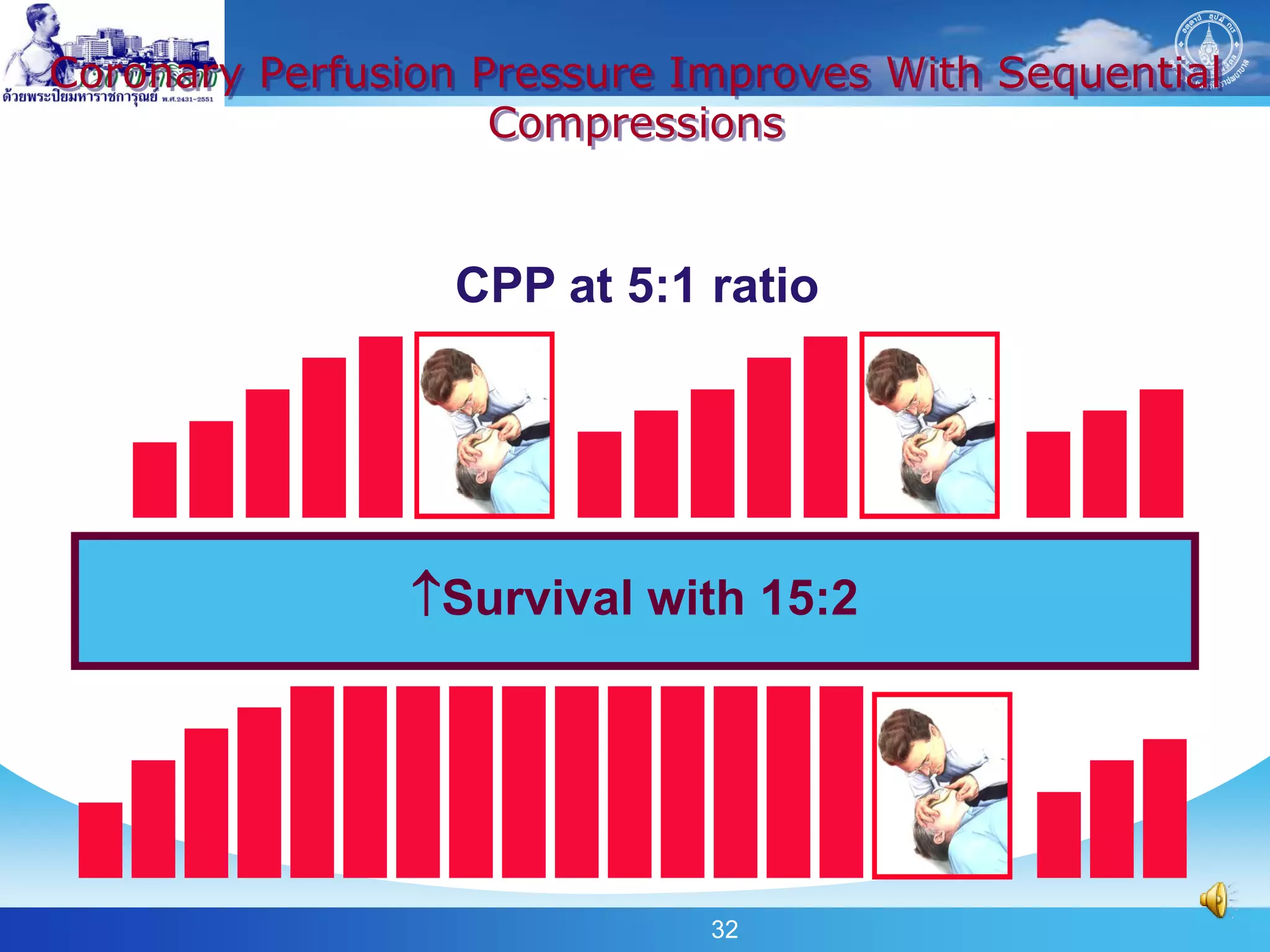
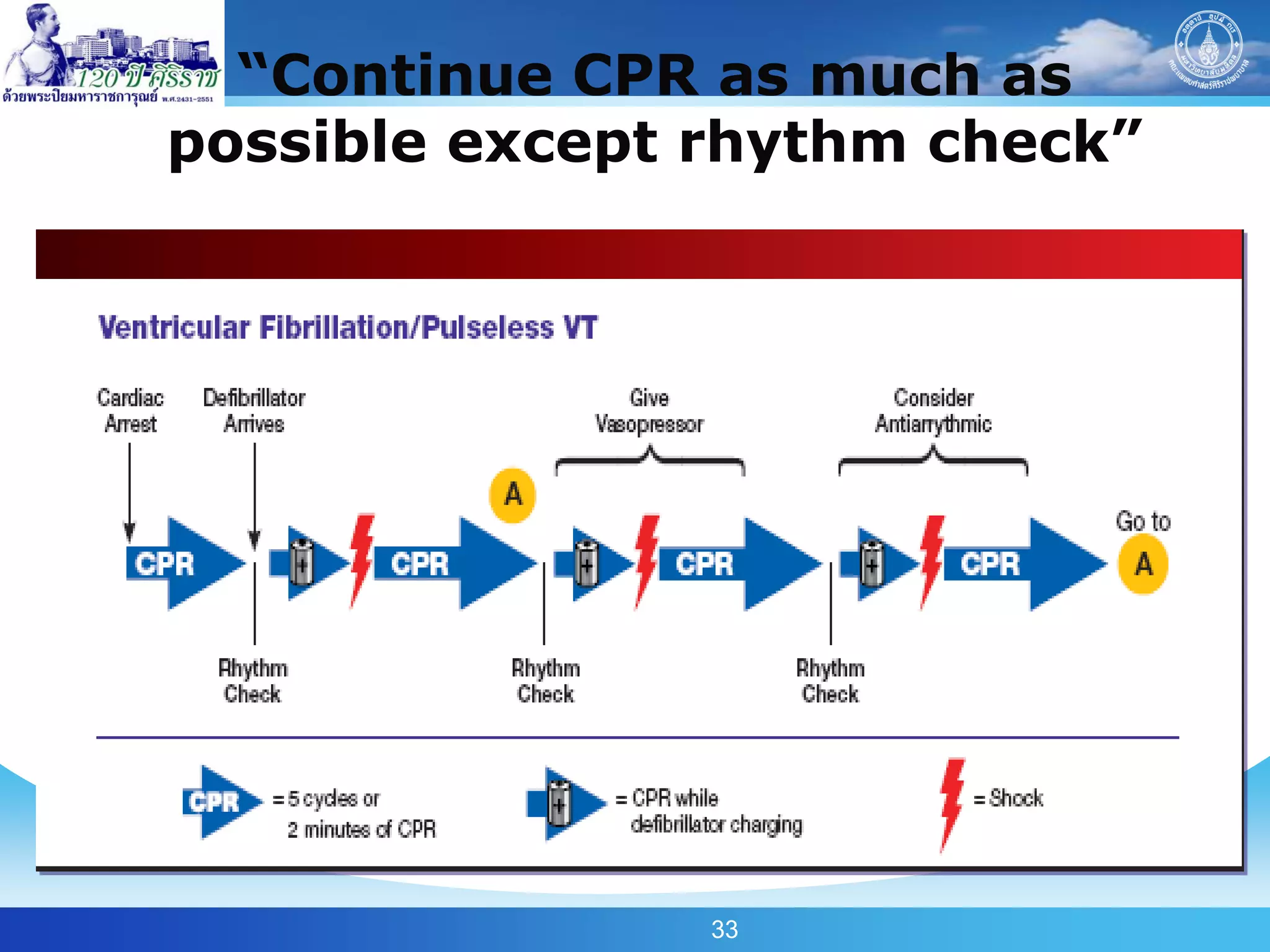
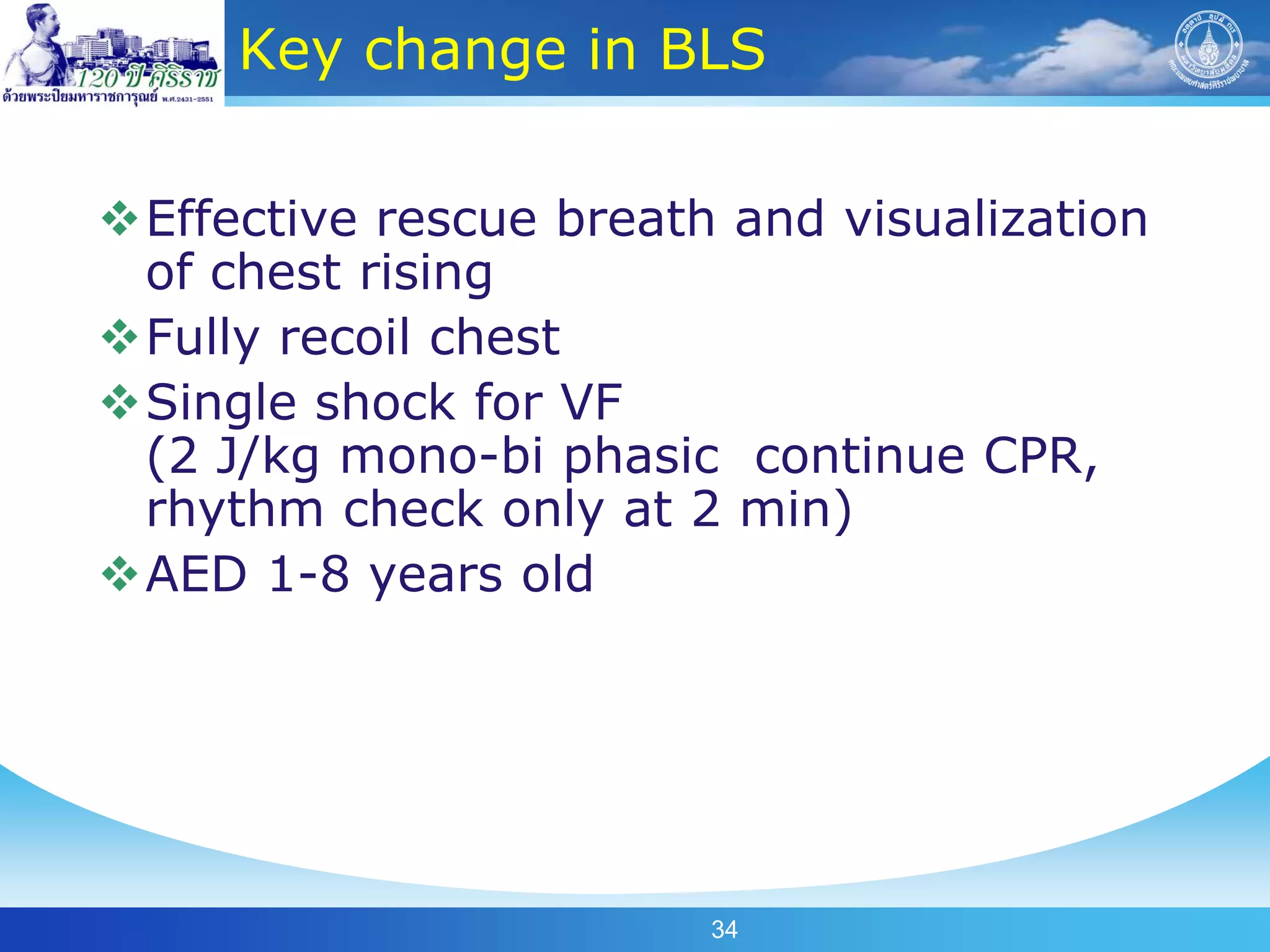
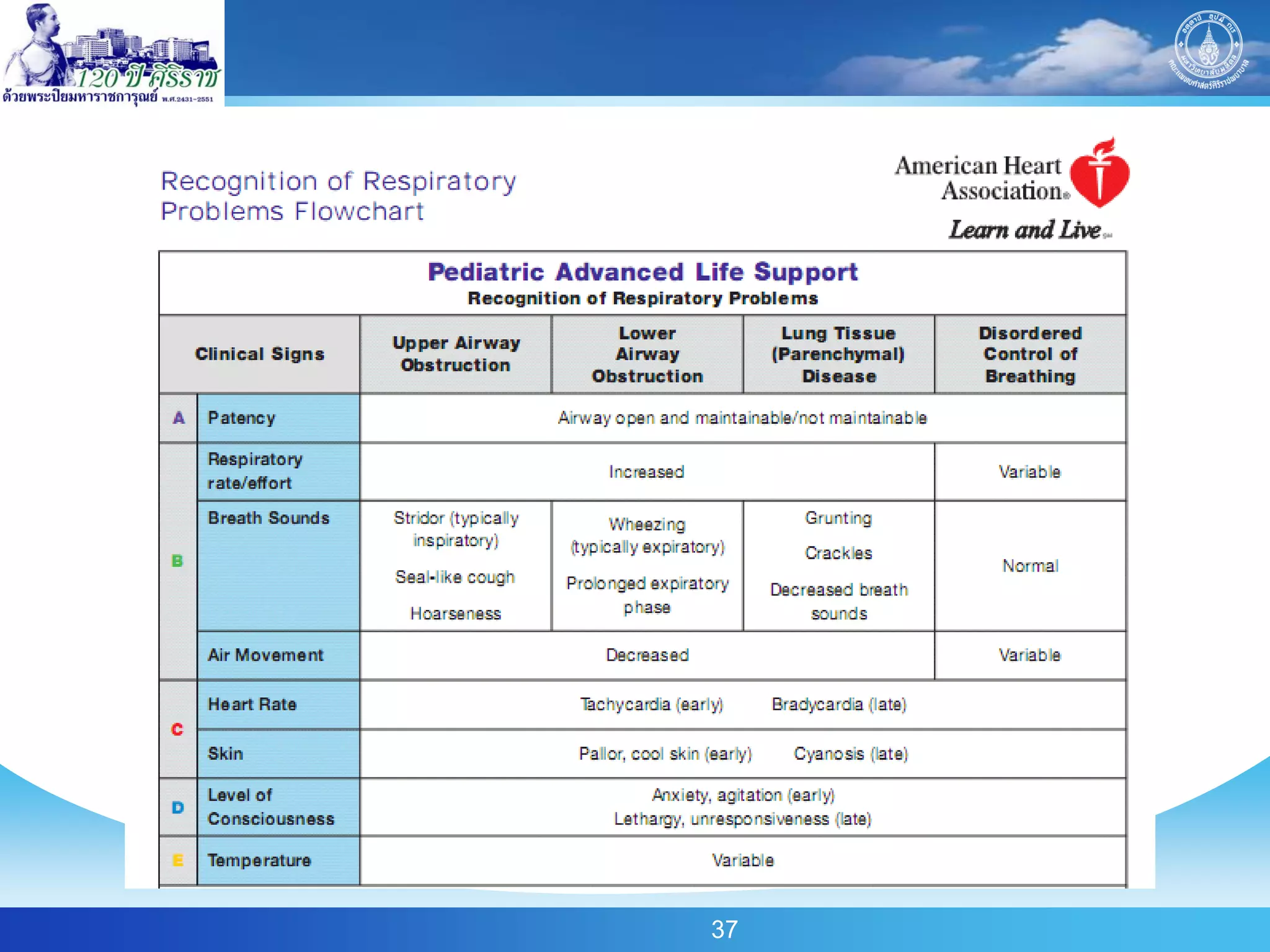
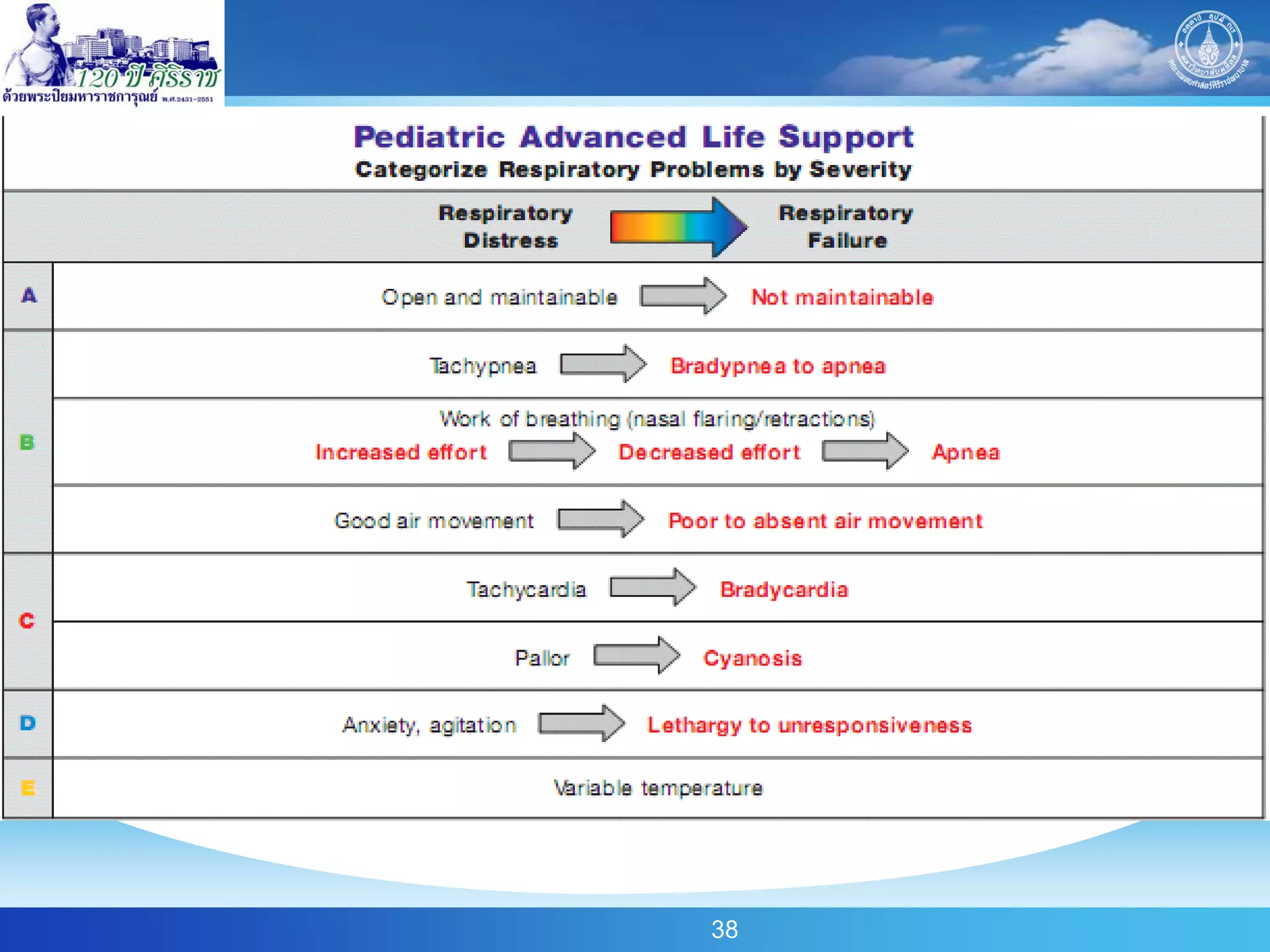
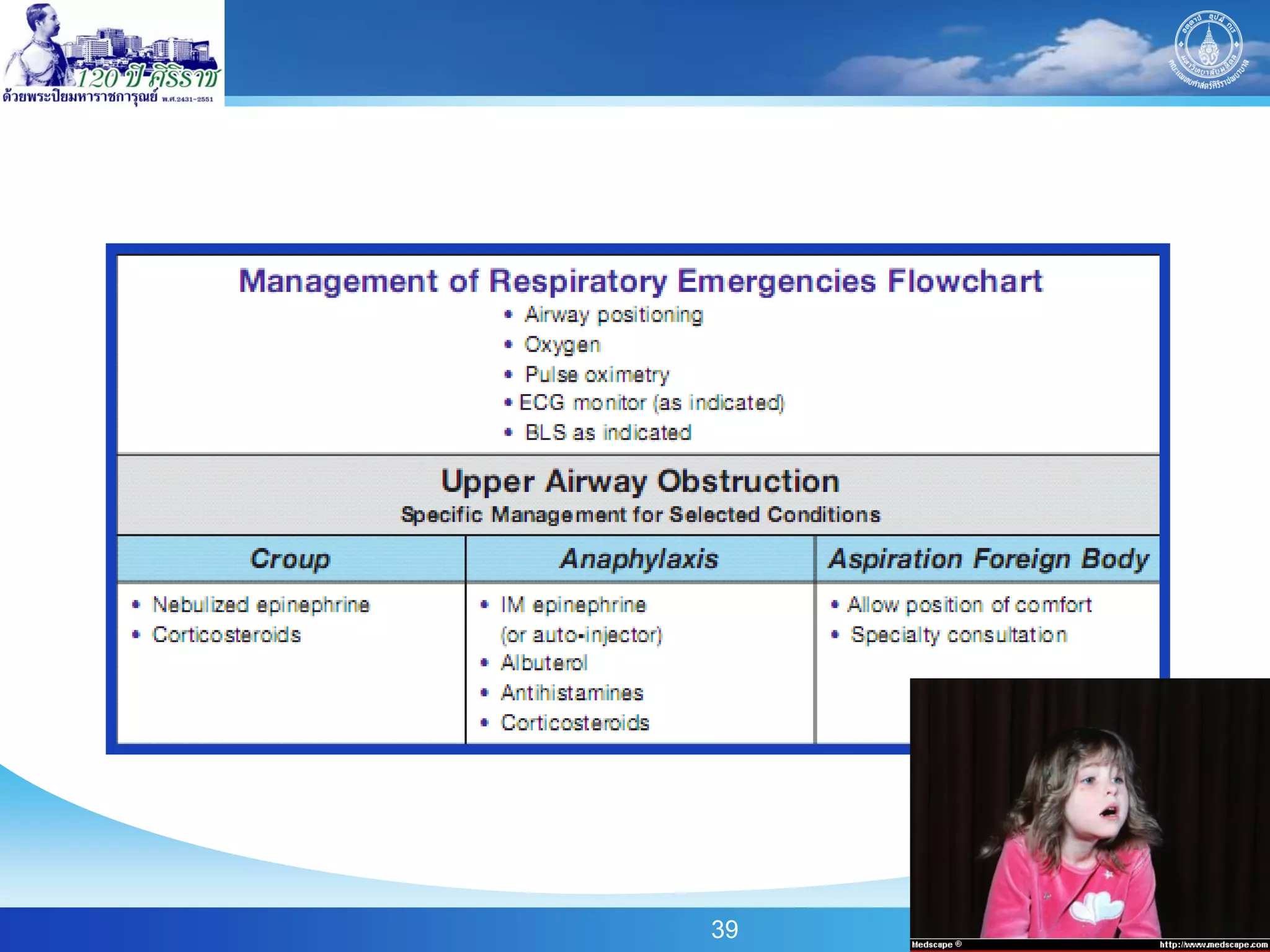
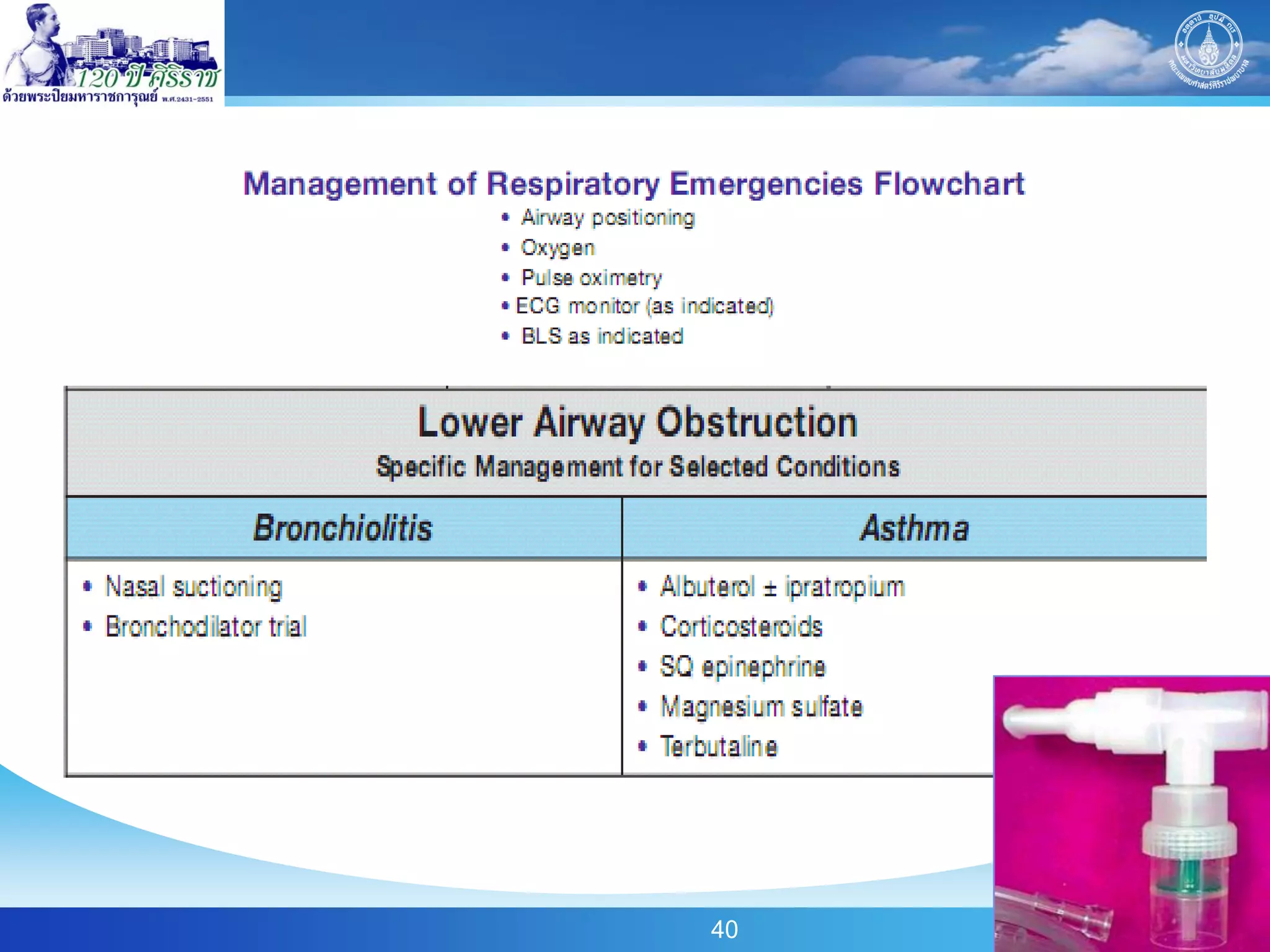
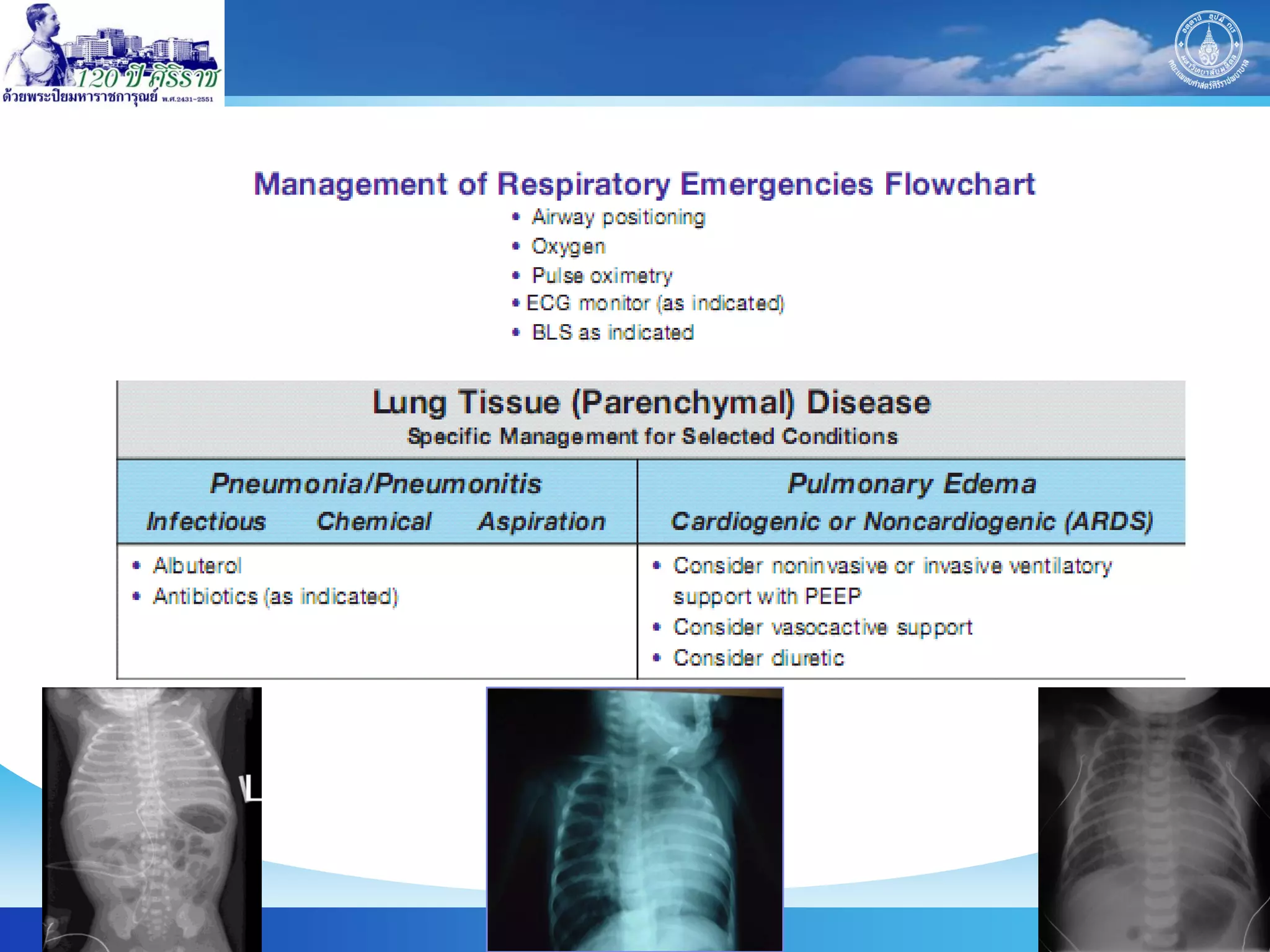
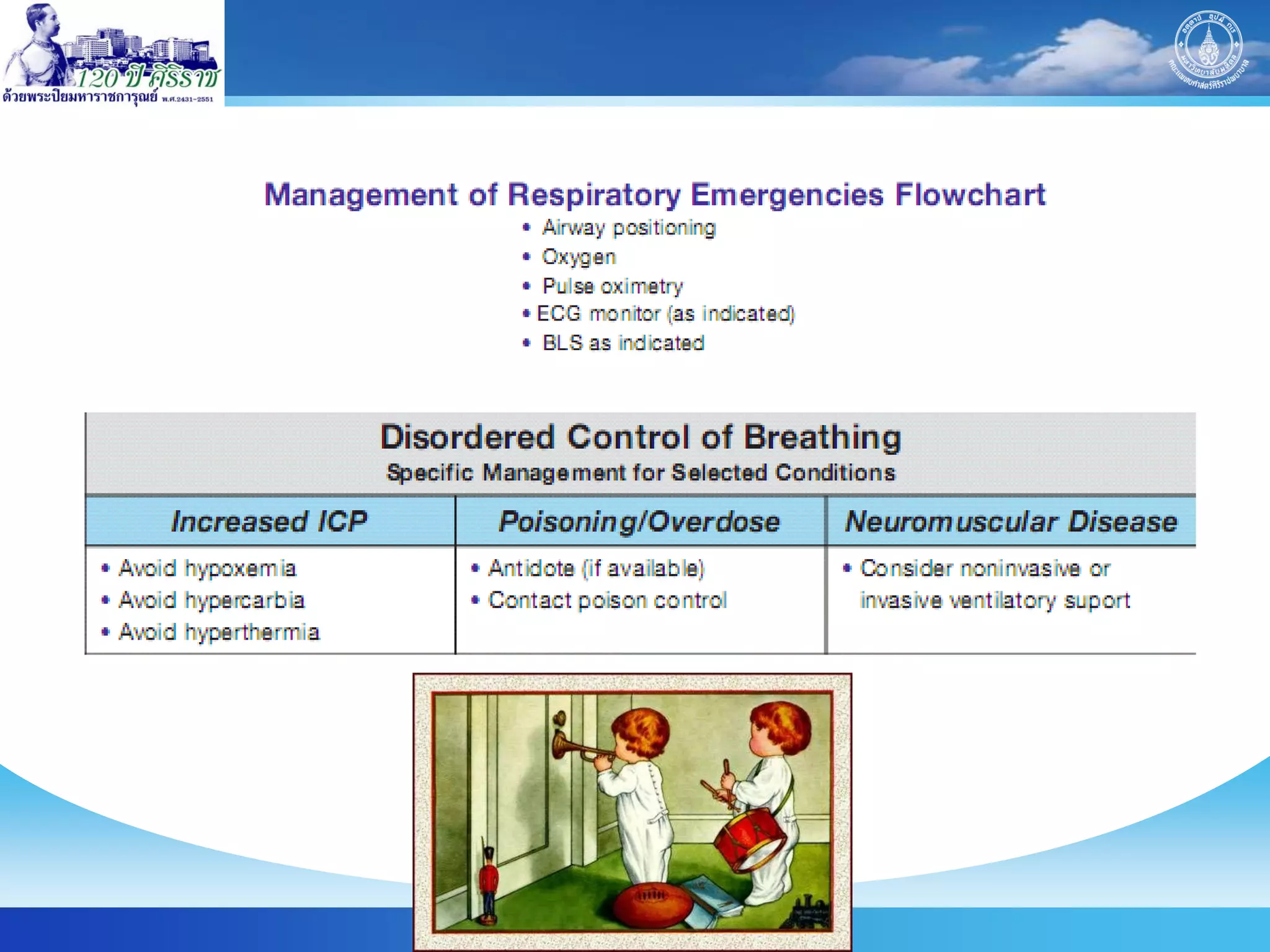
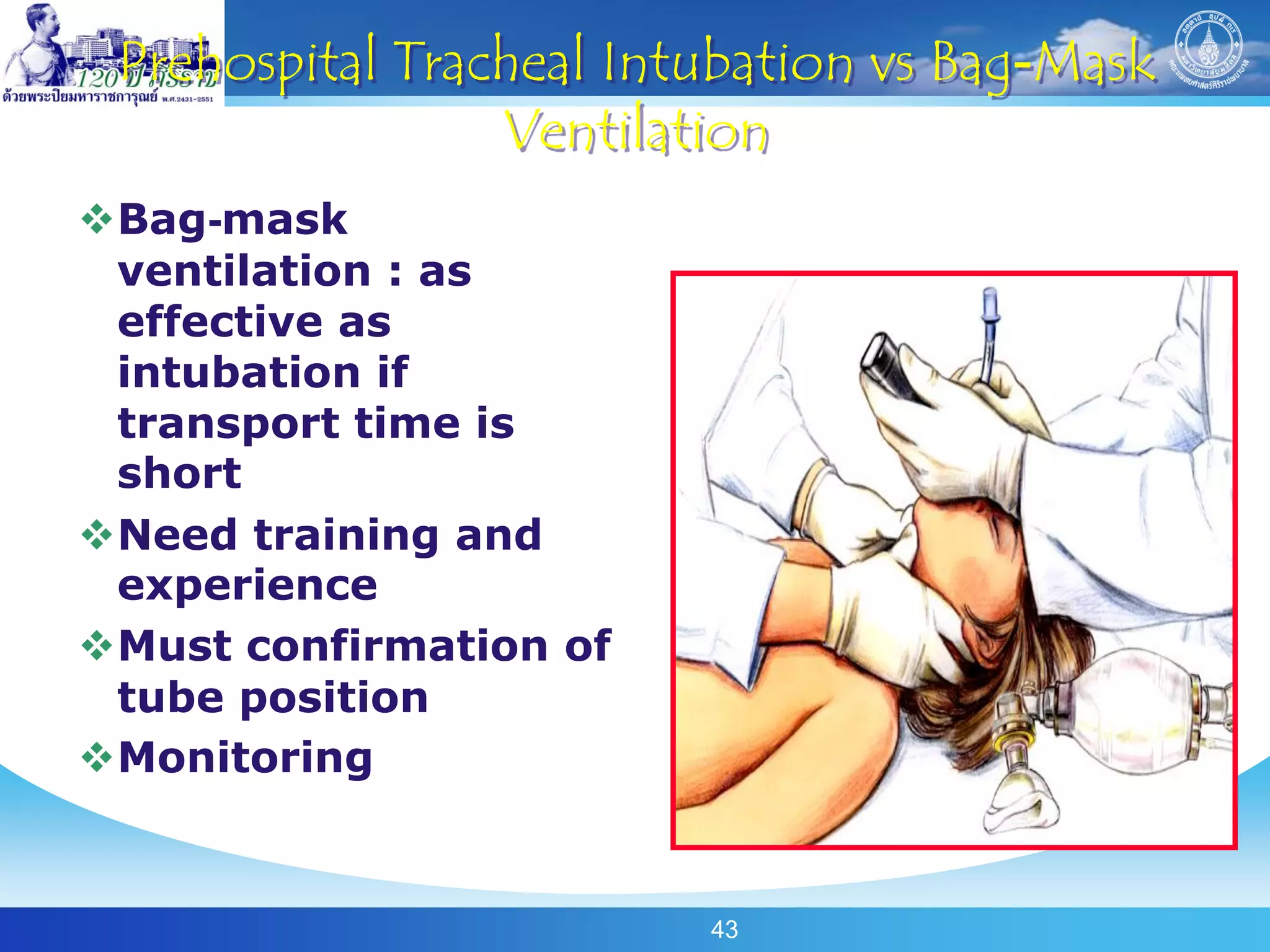
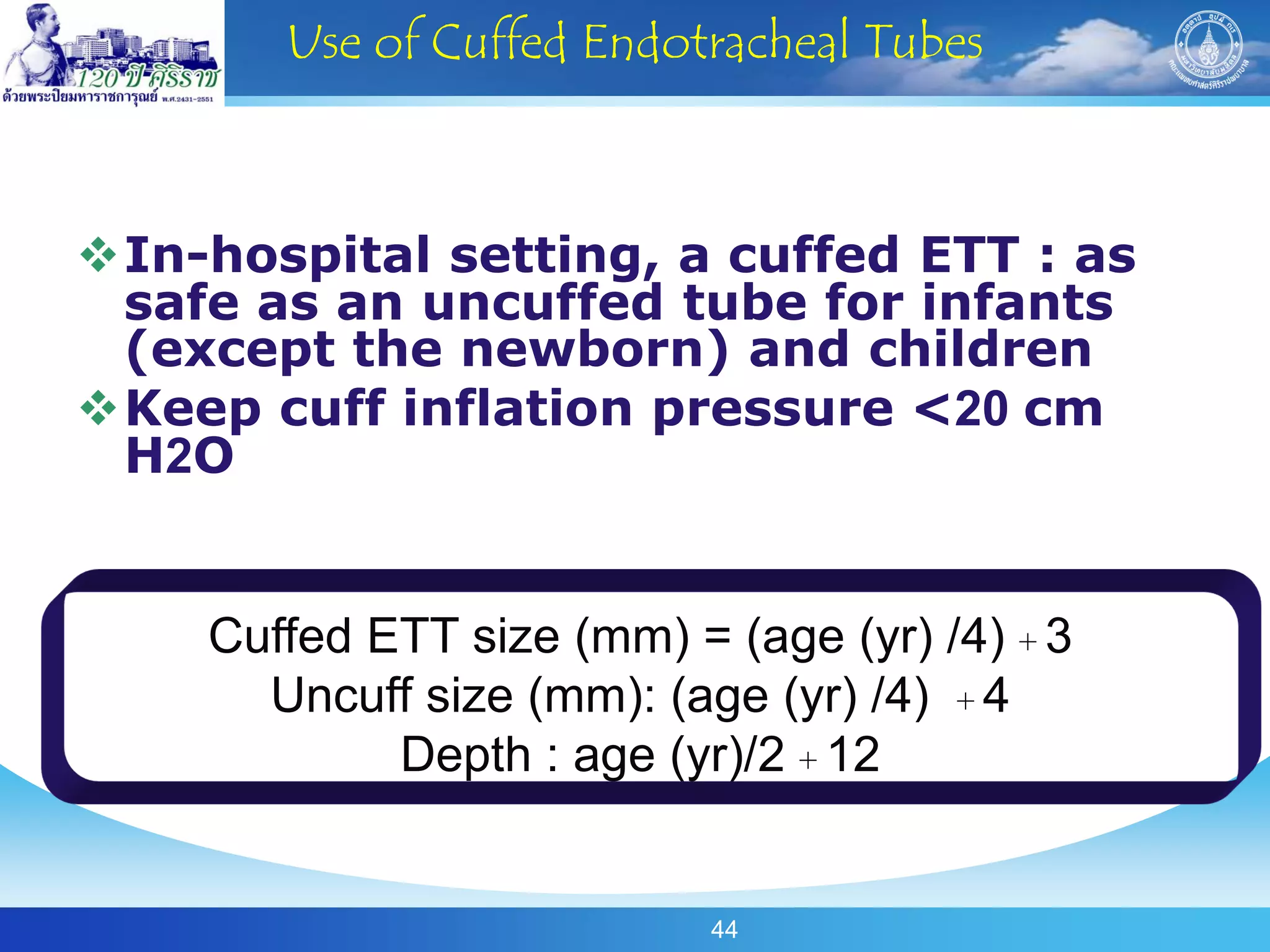
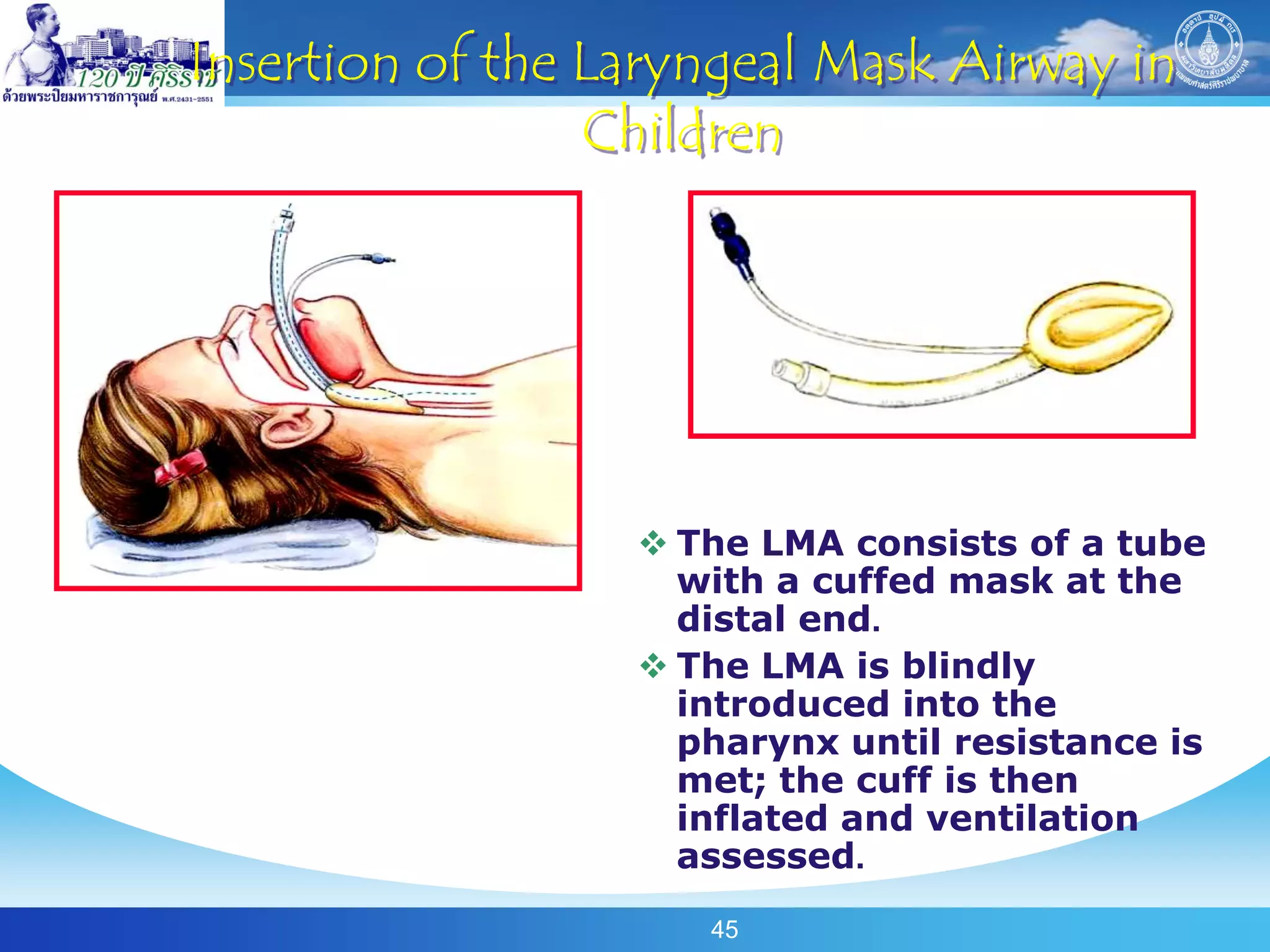
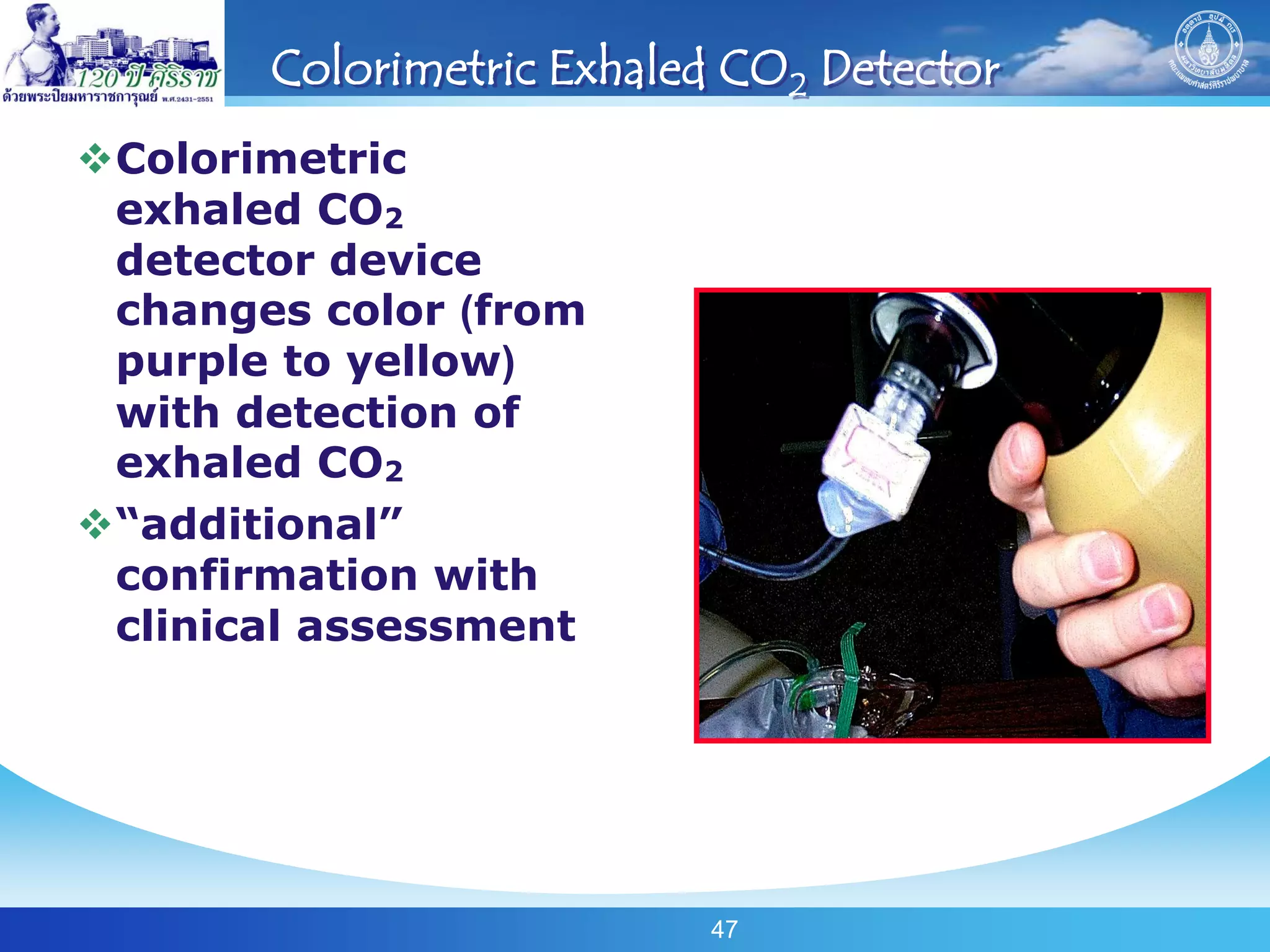
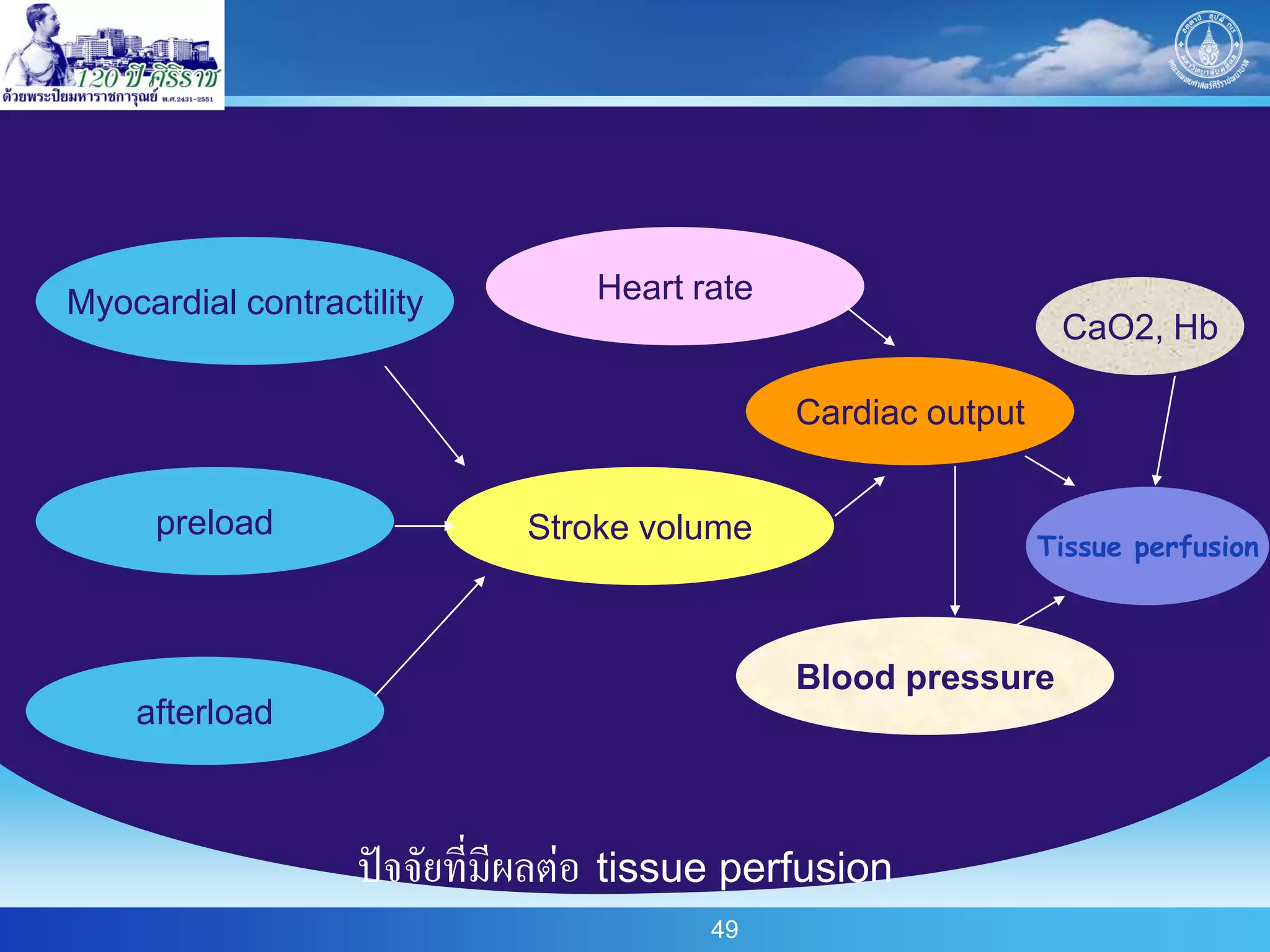
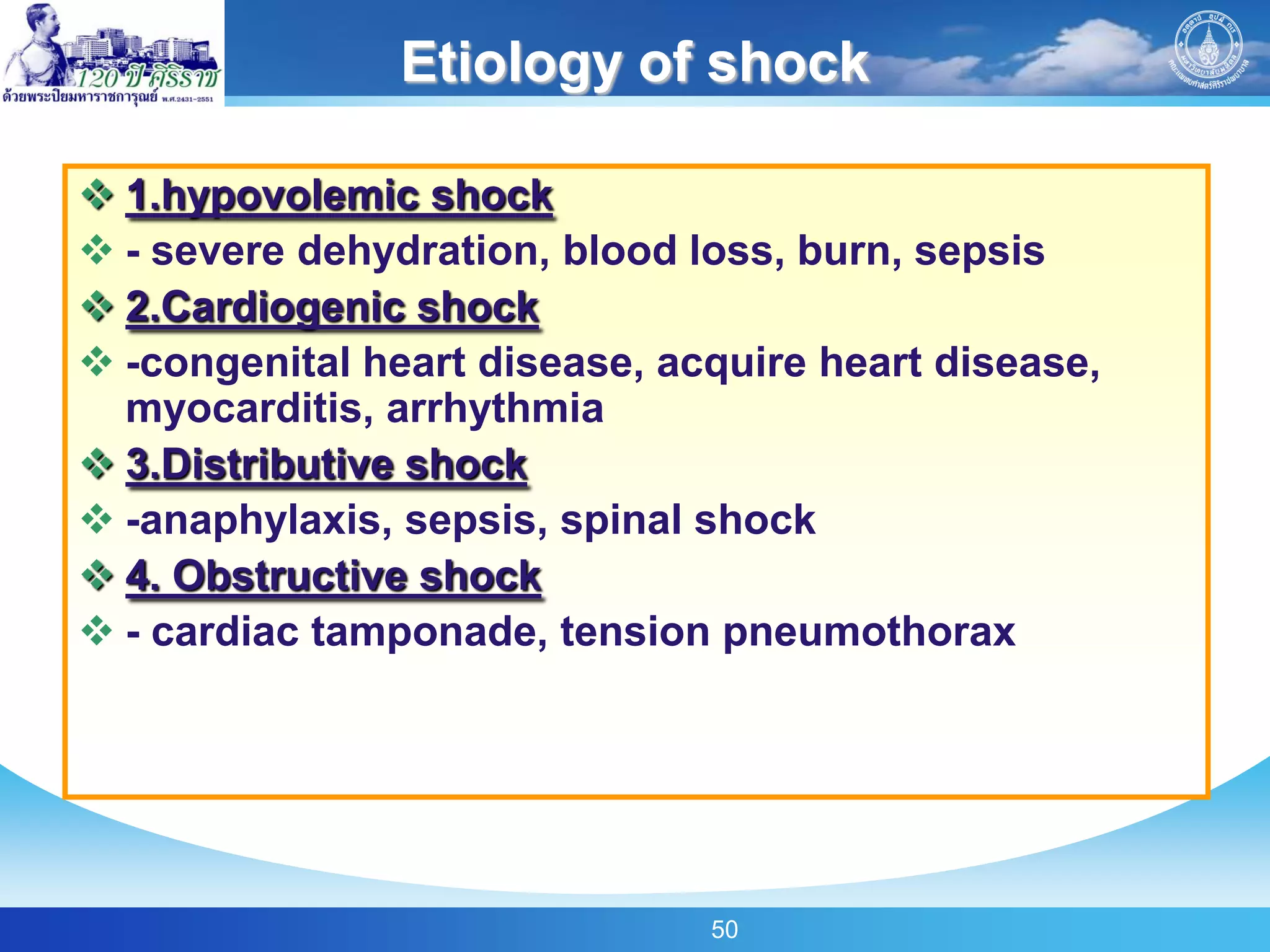
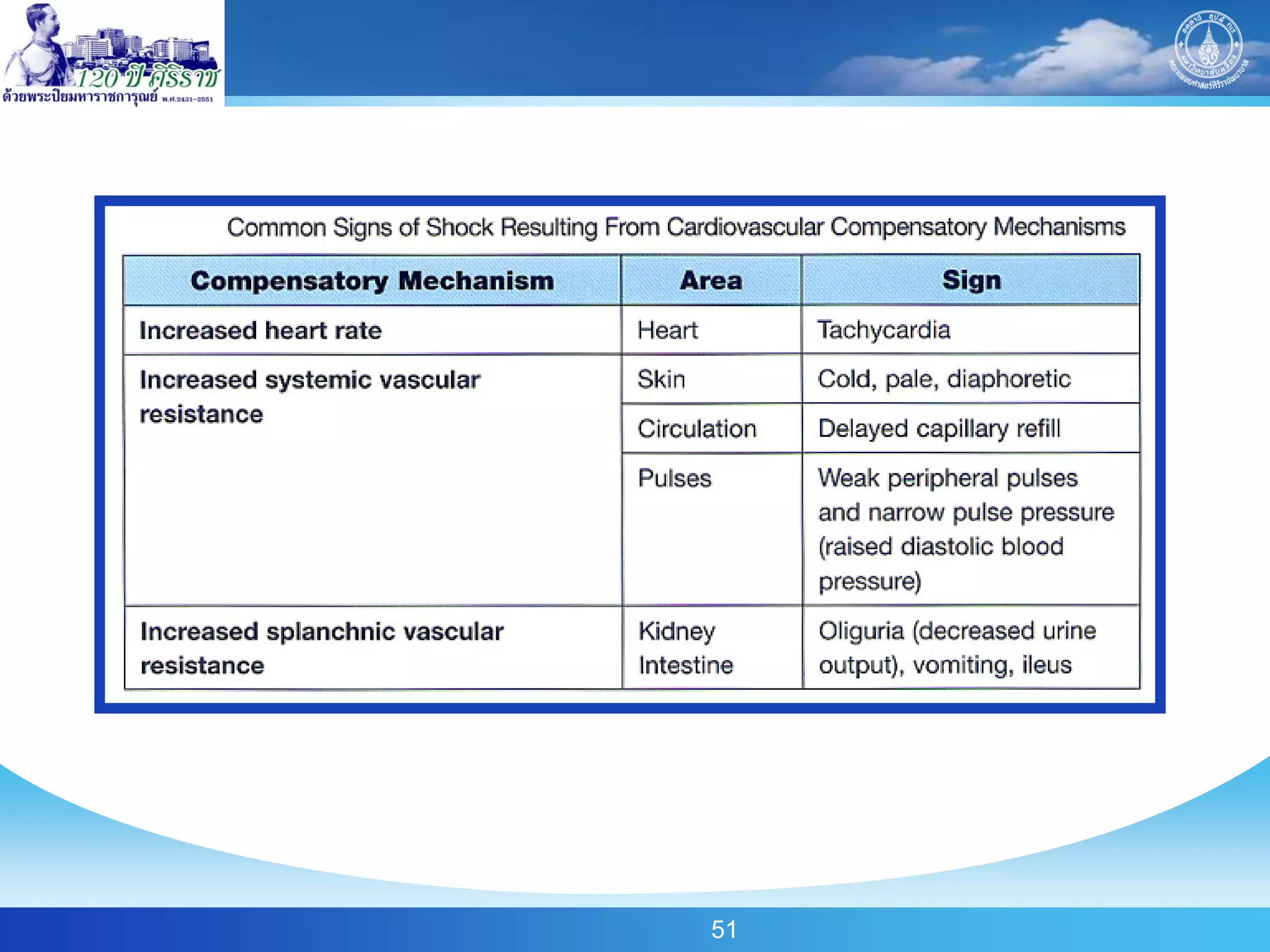
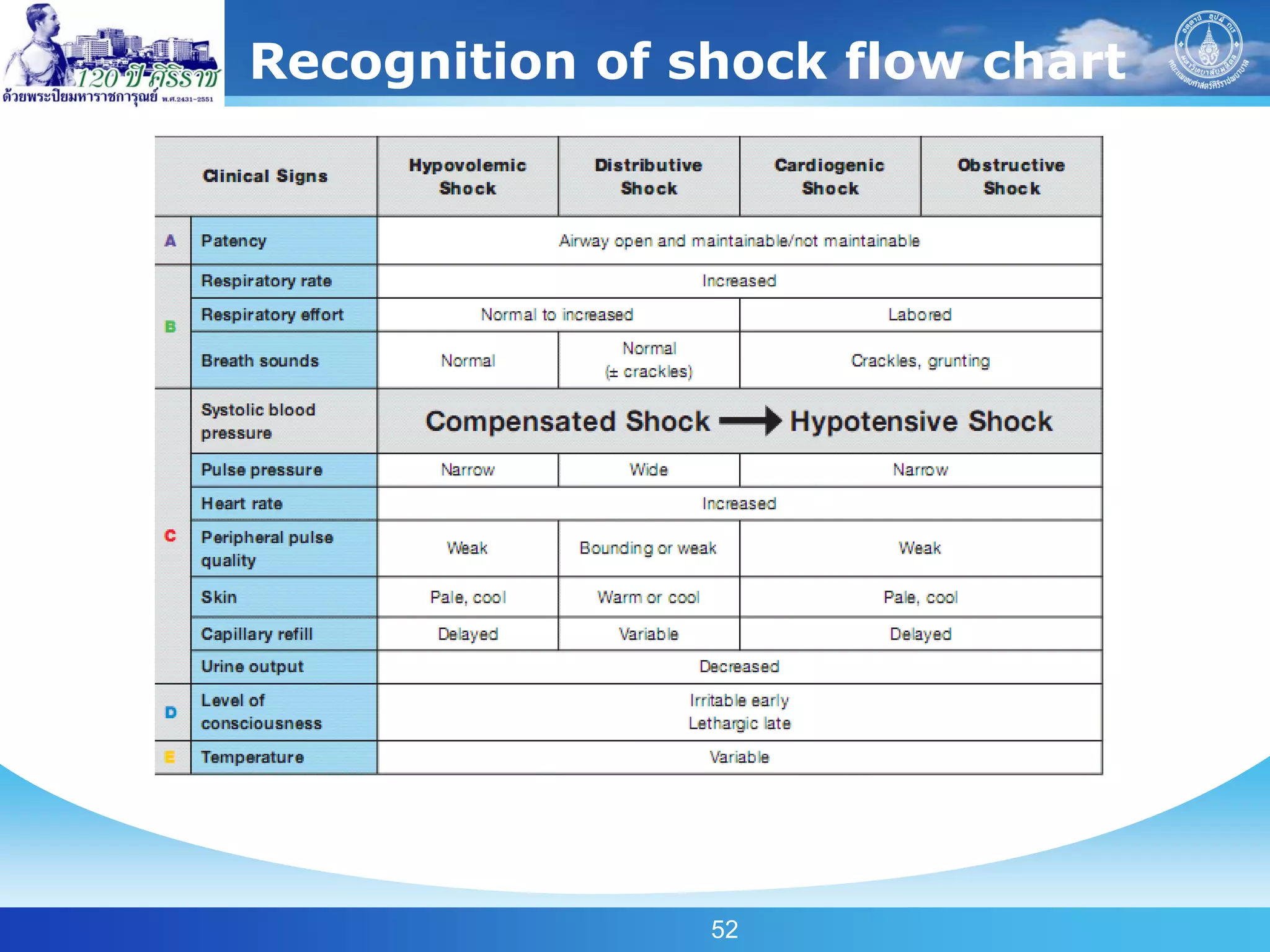
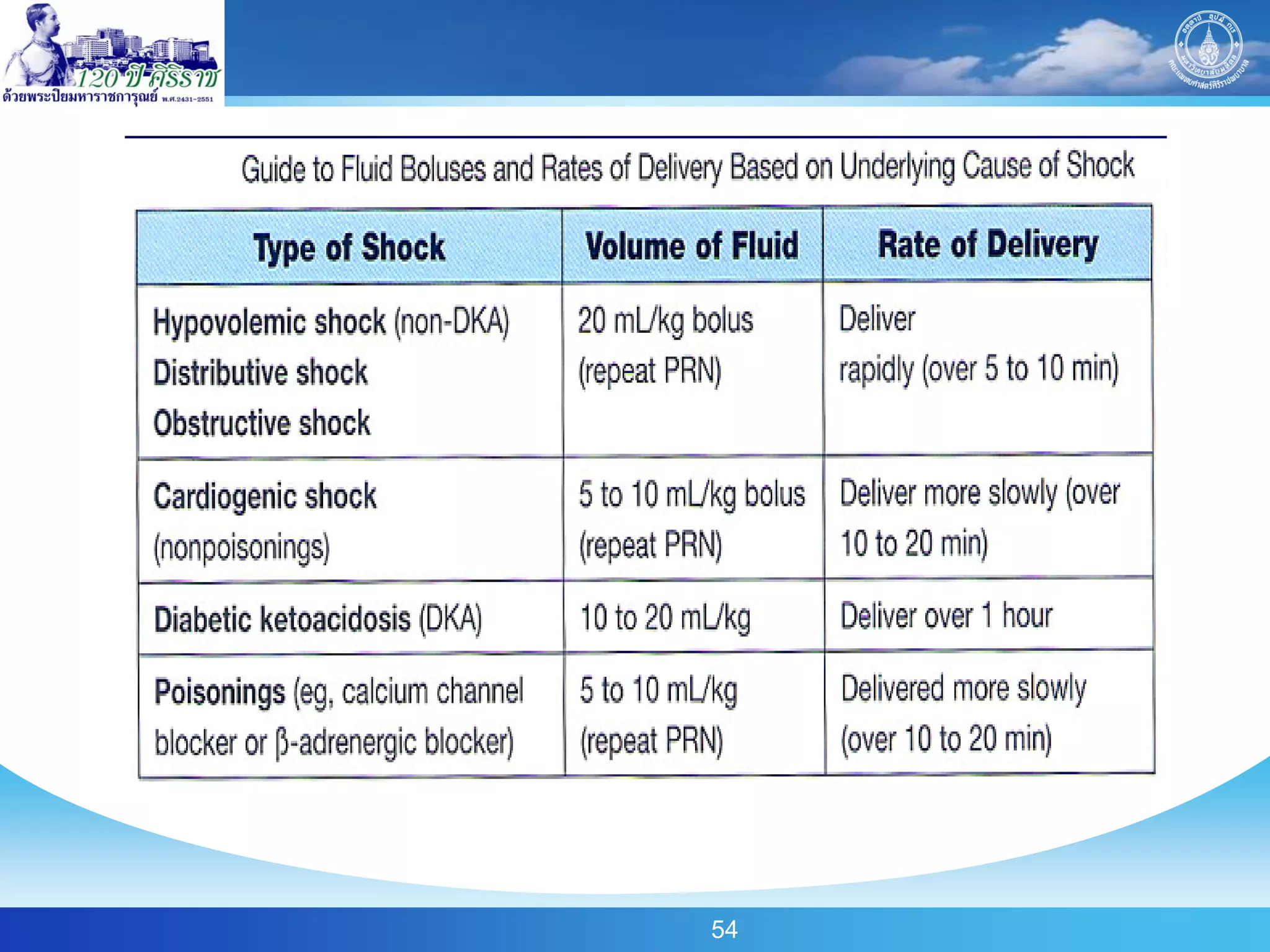
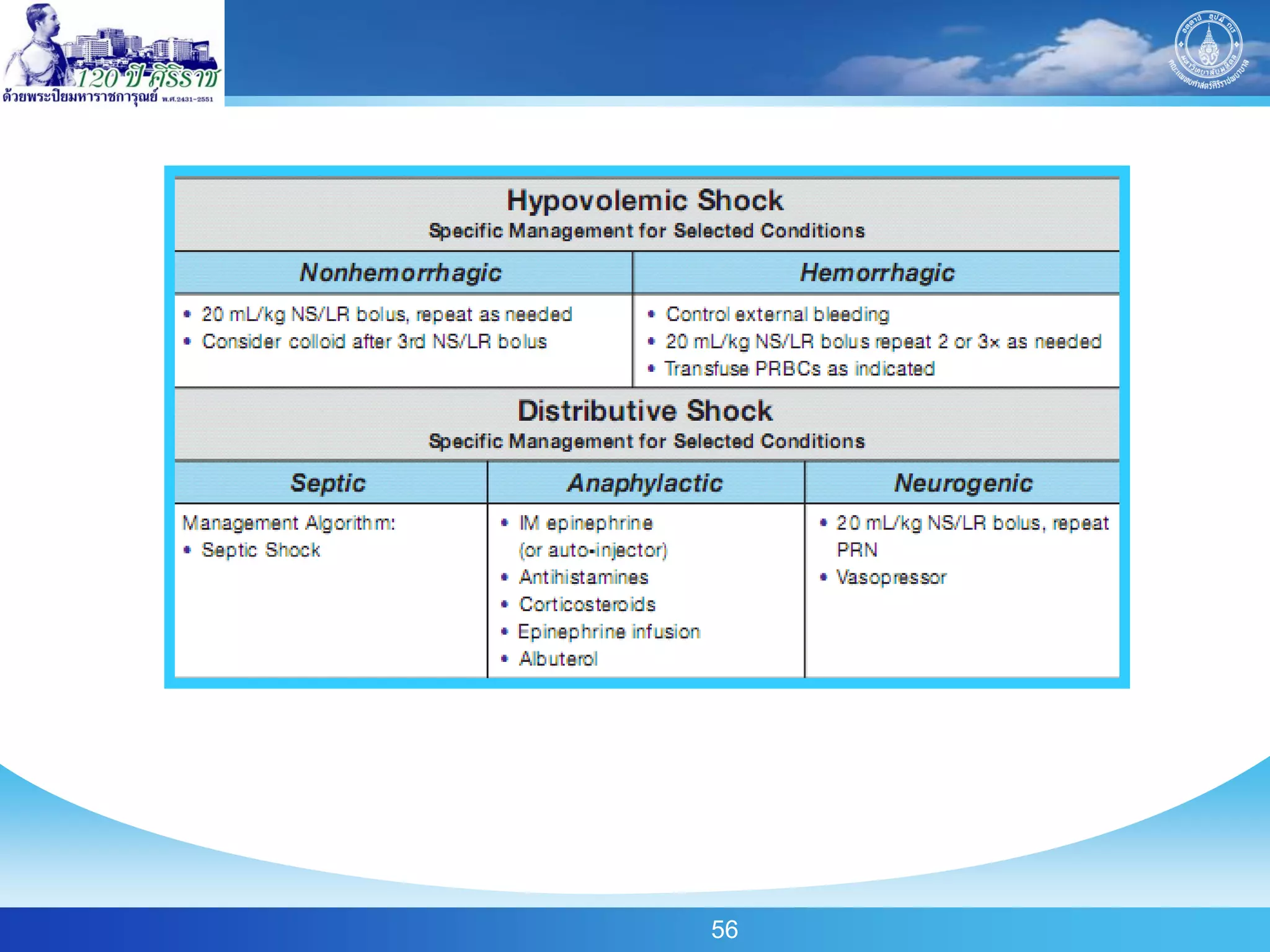
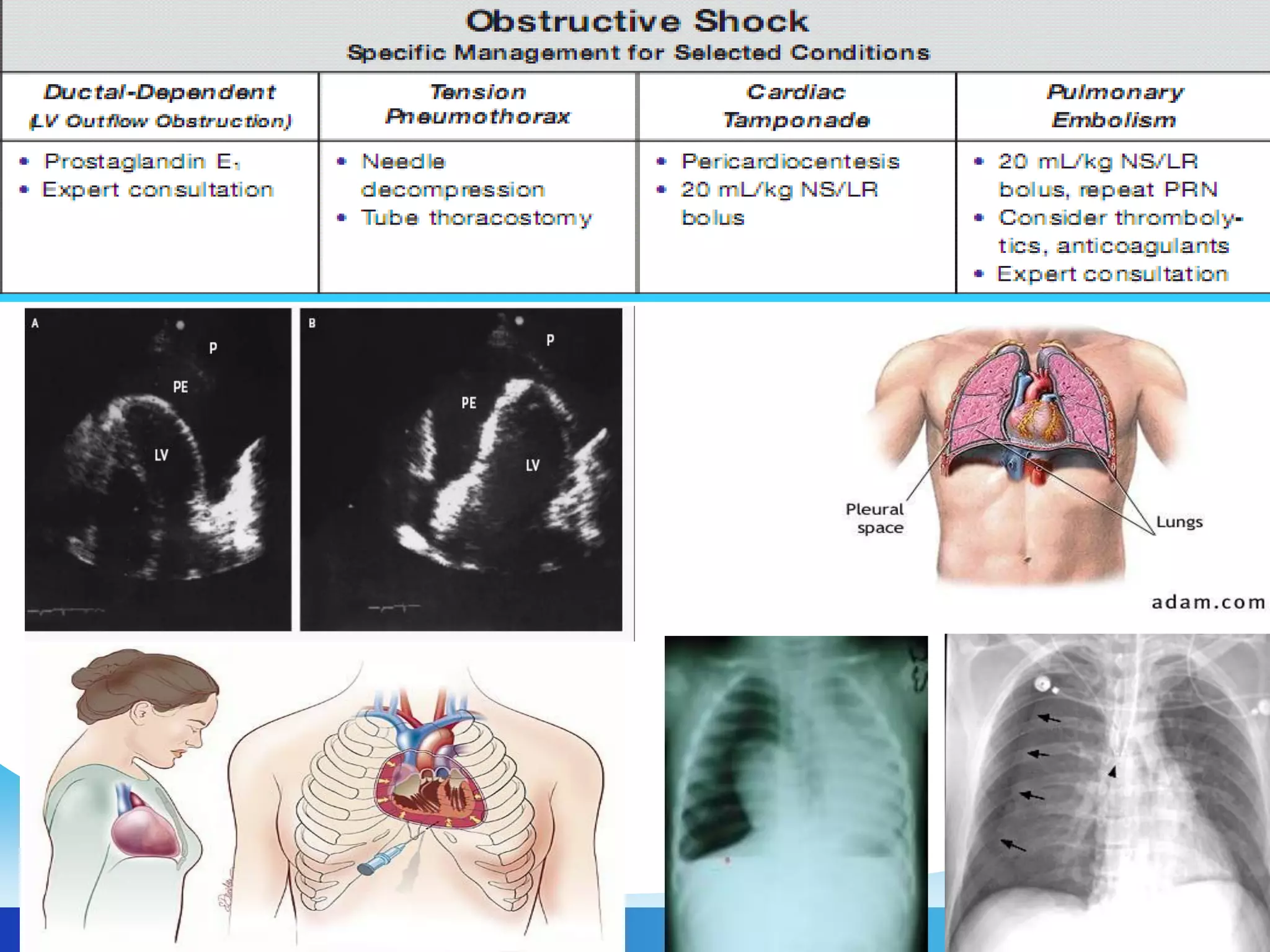
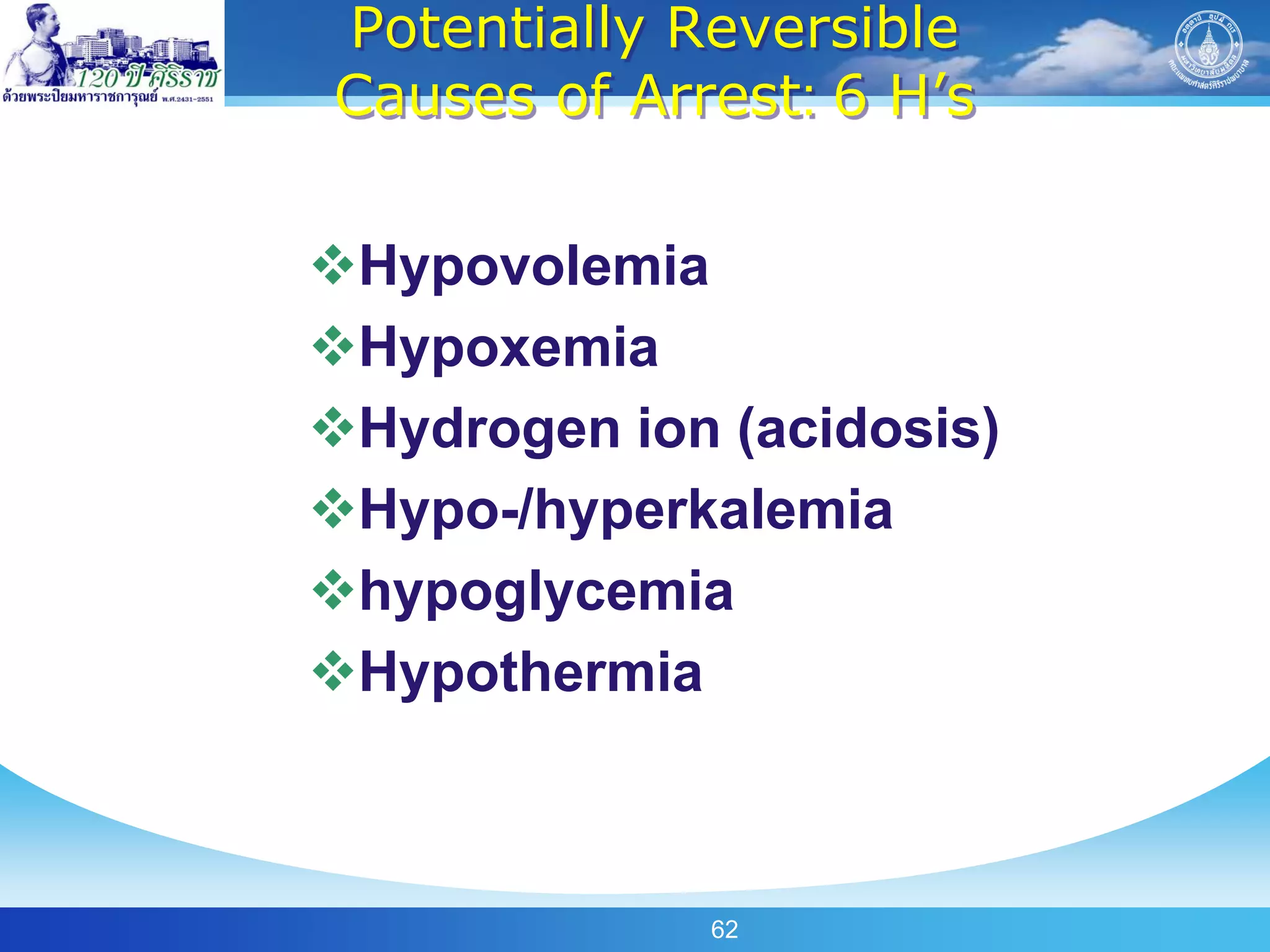
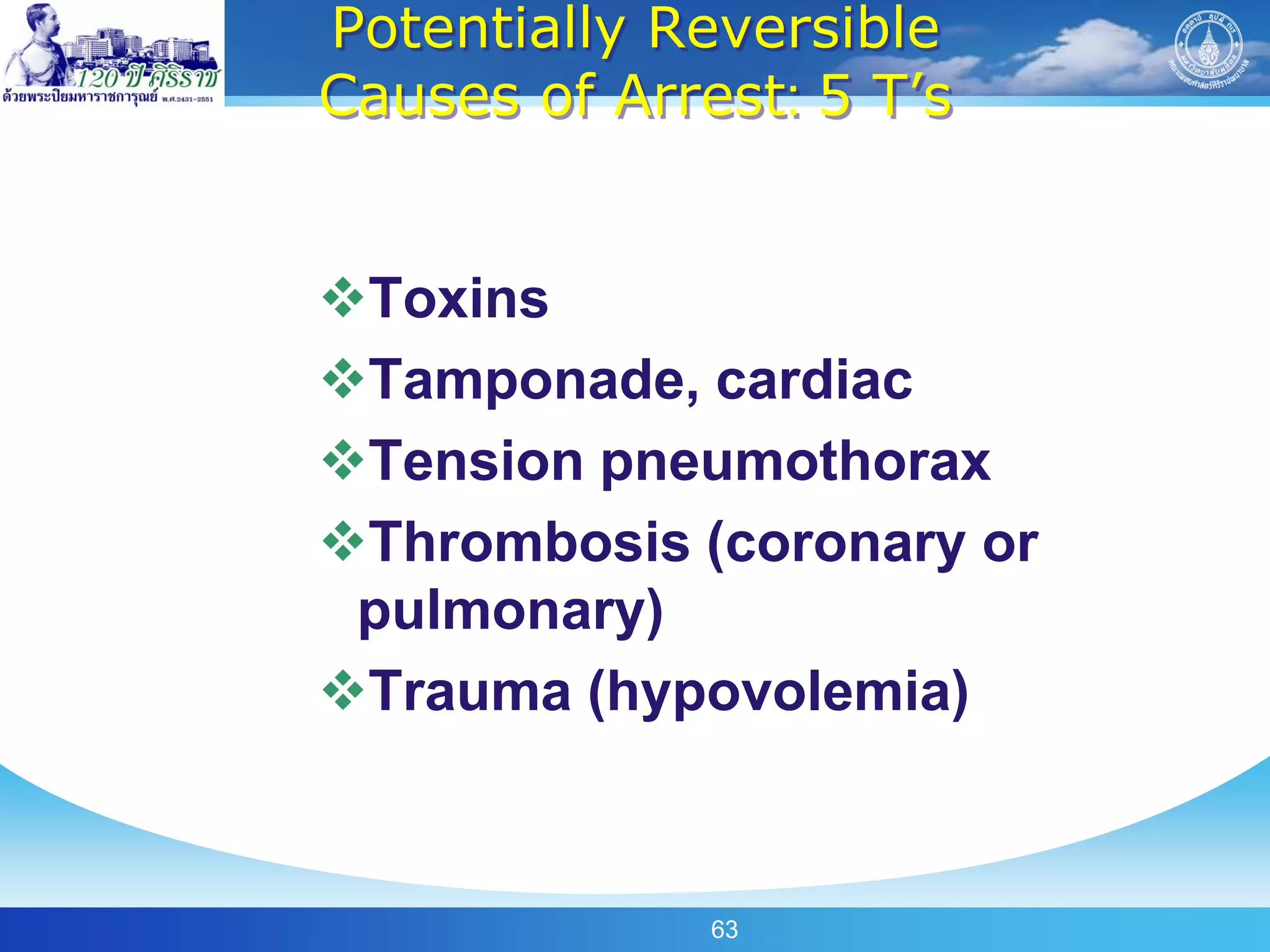
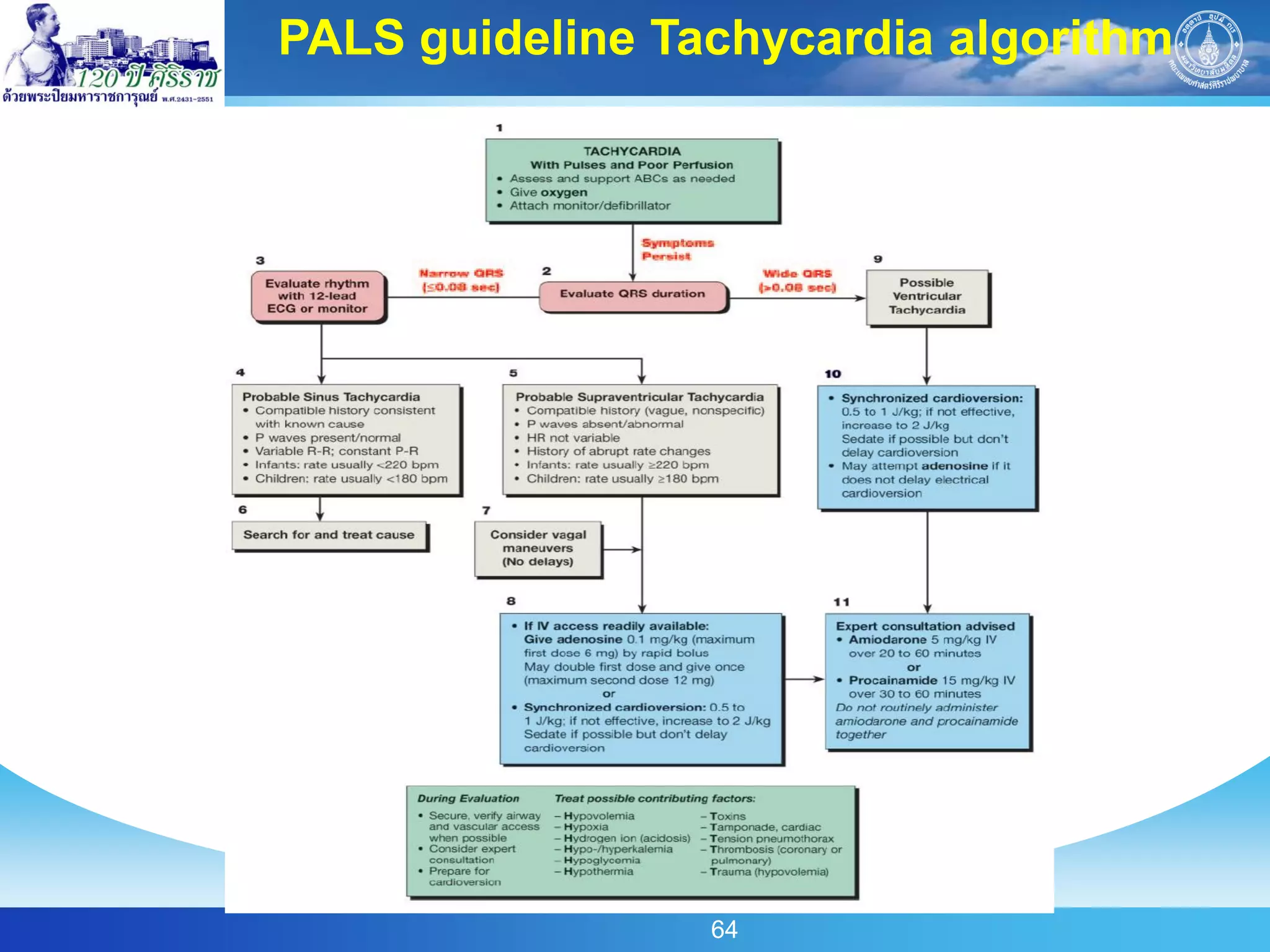
The document summarizes key points from PALS guidelines regarding the assessment and management of pediatric emergencies. It discusses the primary, secondary, and tertiary assessments using ABCDE/SAMPLE approaches. Signs of life-threatening conditions like airway obstruction, respiratory distress, and shock are outlined. The document also reviews recent PALS recommendations for compressions-to-ventilations ratios, use of cuffed endotracheal tubes, laryngeal mask airways, and exhaled CO2 detectors for confirming endotracheal tube placement.