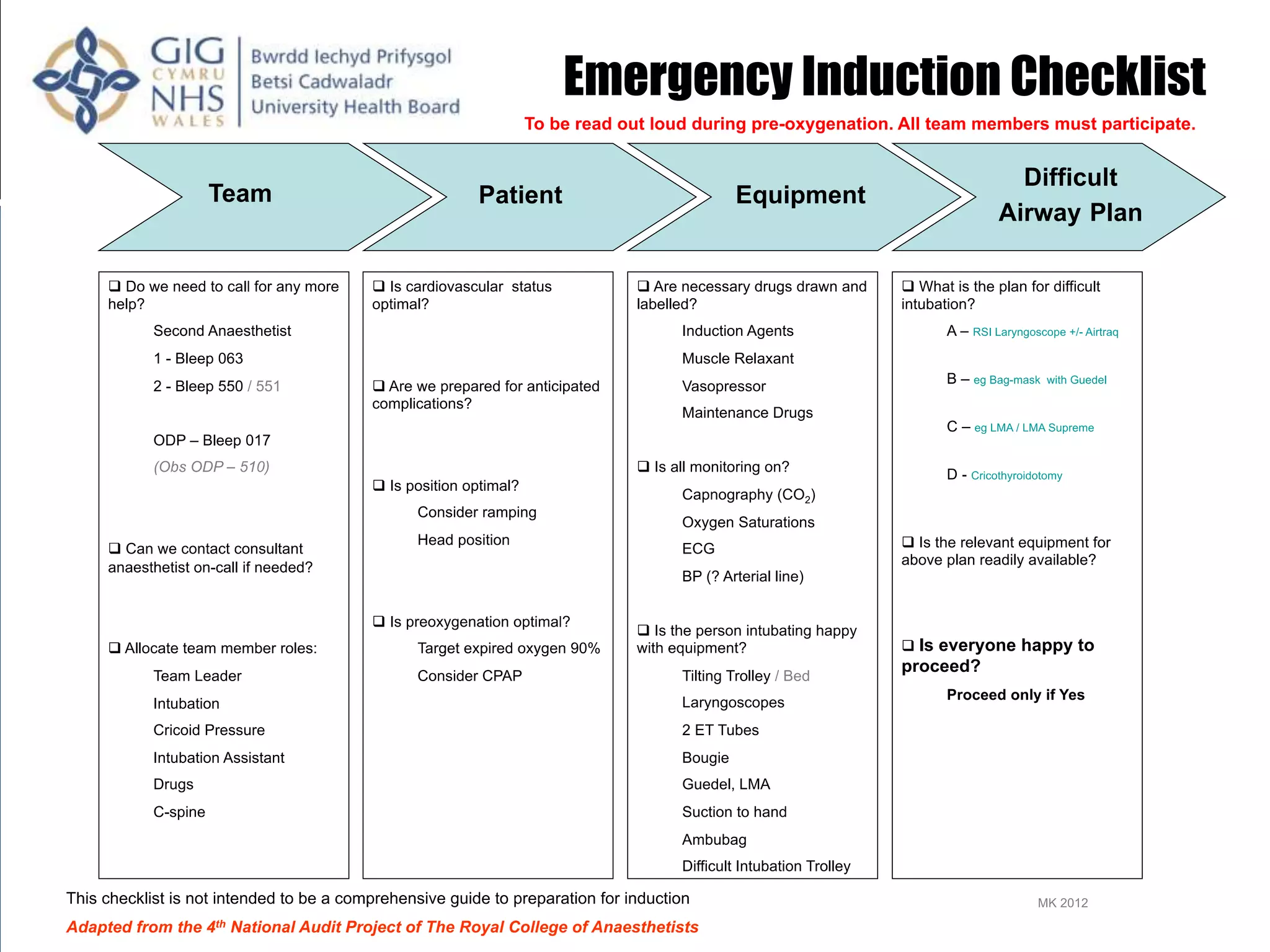
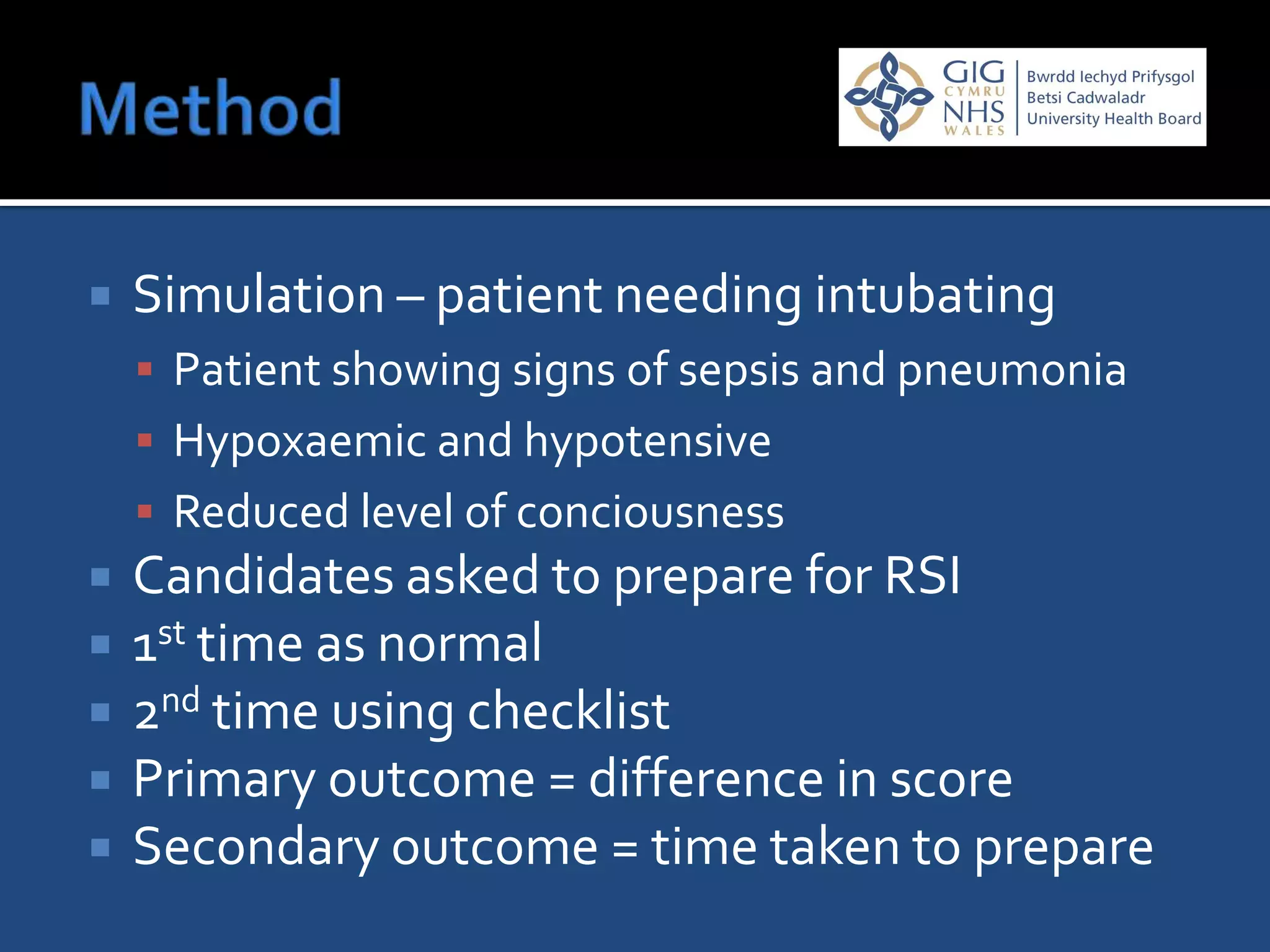
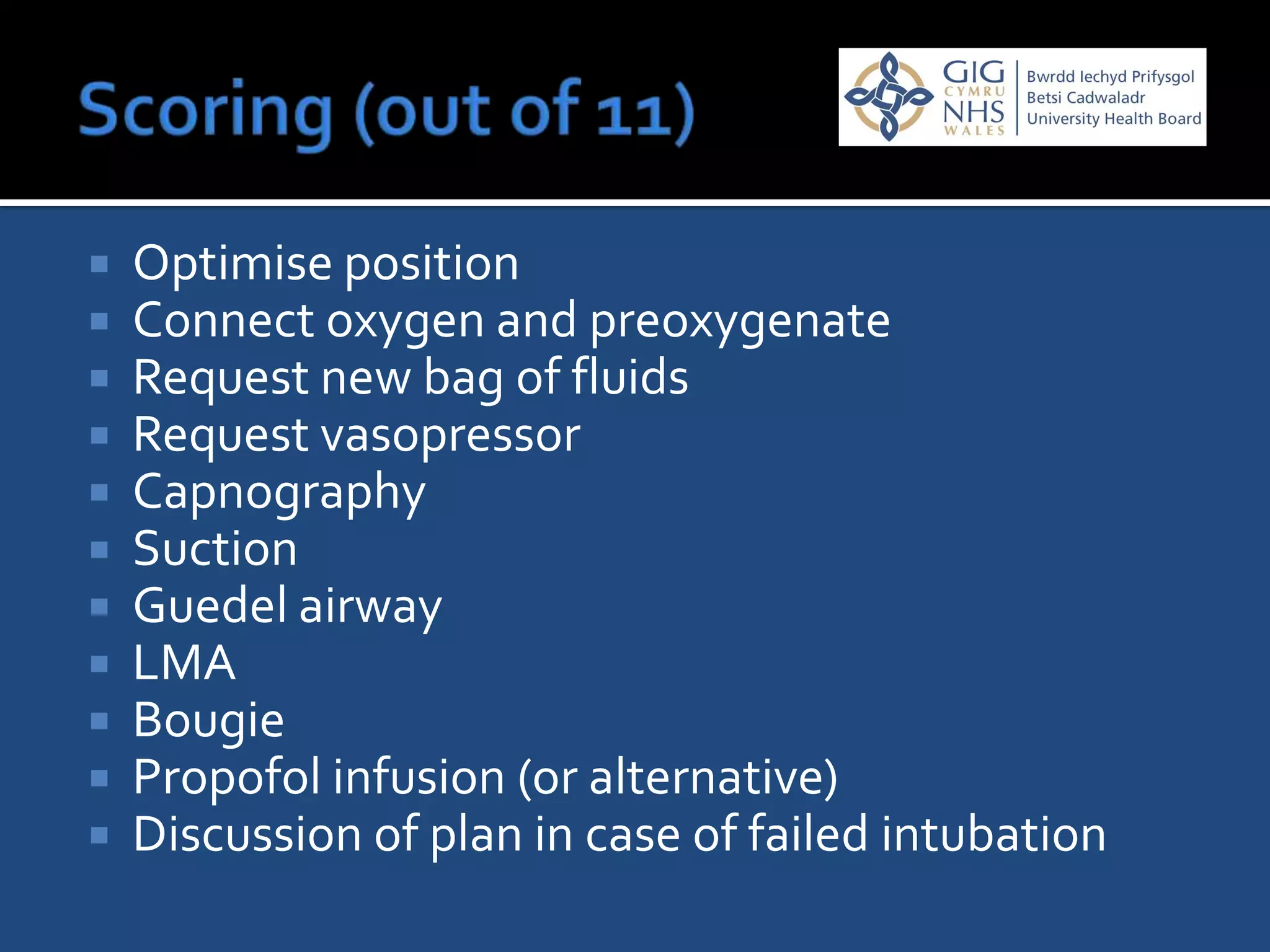
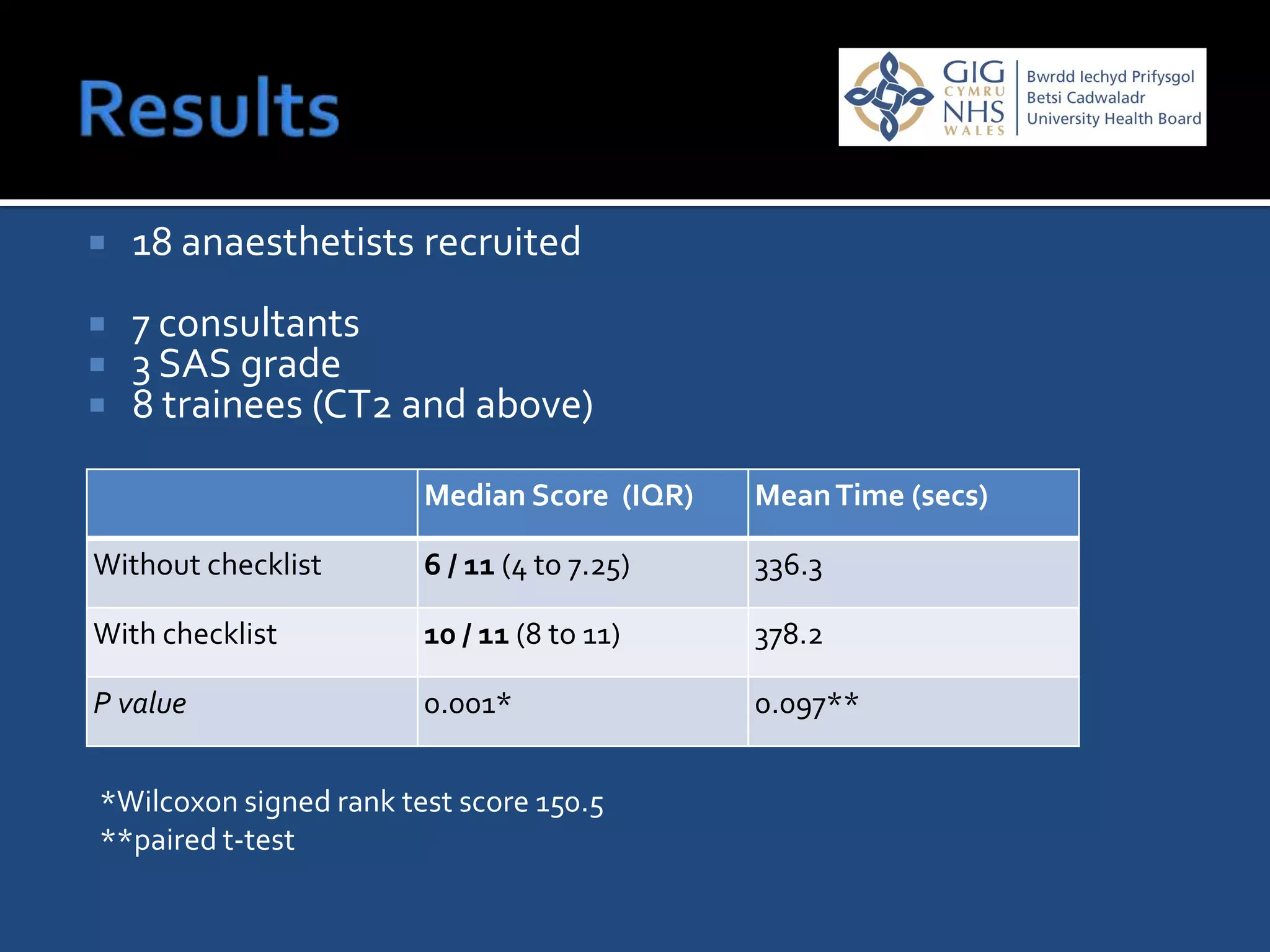
This document presents the findings of a study that tested the use of a checklist for rapid sequence intubations (RSI) in emergency situations. Eighteen anesthetists participated in a simulation where they prepared for an RSI with and without a checklist. The median score for preparation was higher when using the checklist. There was no significant difference in time taken. The checklist significantly reduced errors in preparation and appeared to do so regardless of experience level, suggesting that checklists can improve patient safety during emergency intubations.