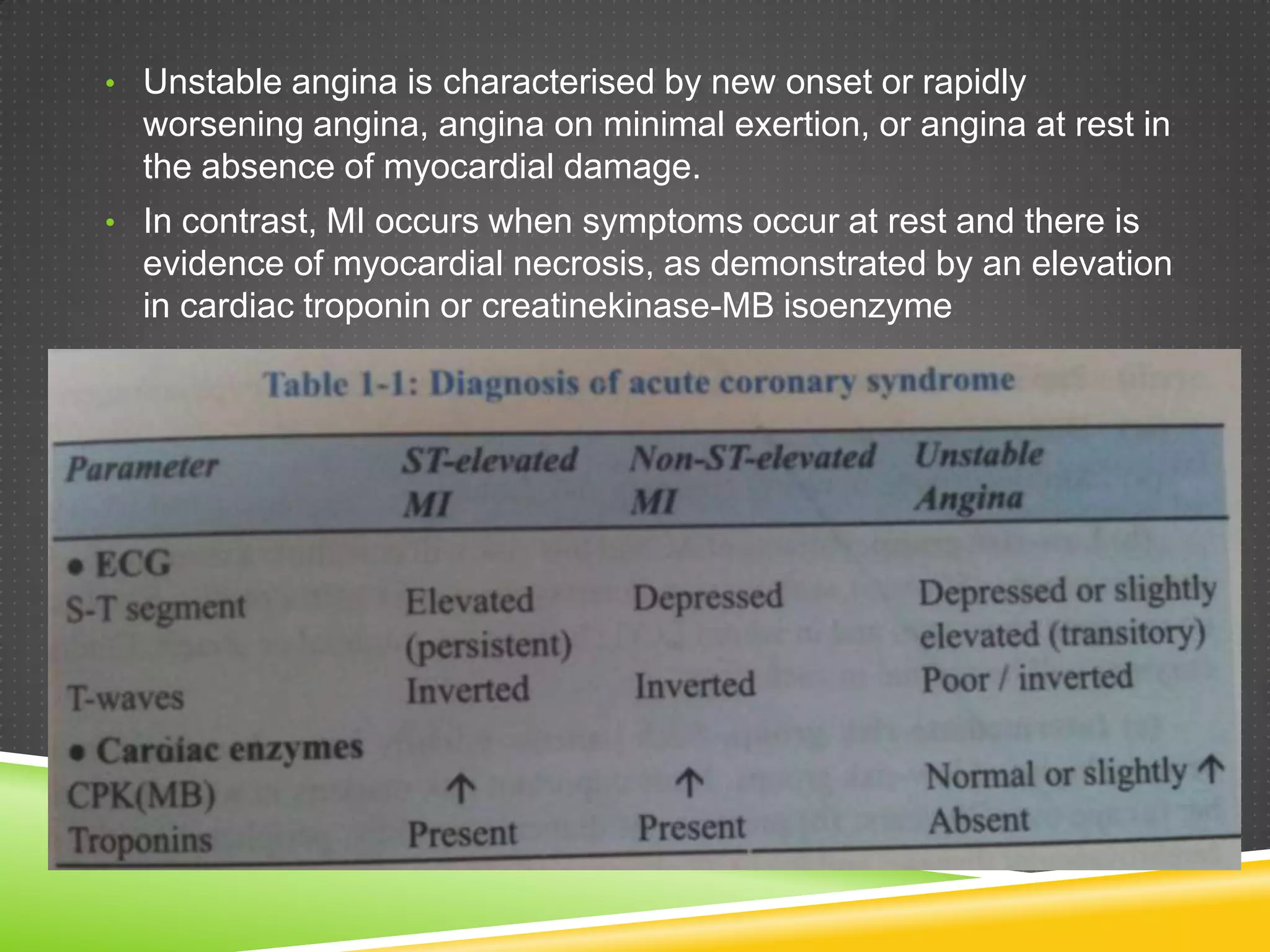
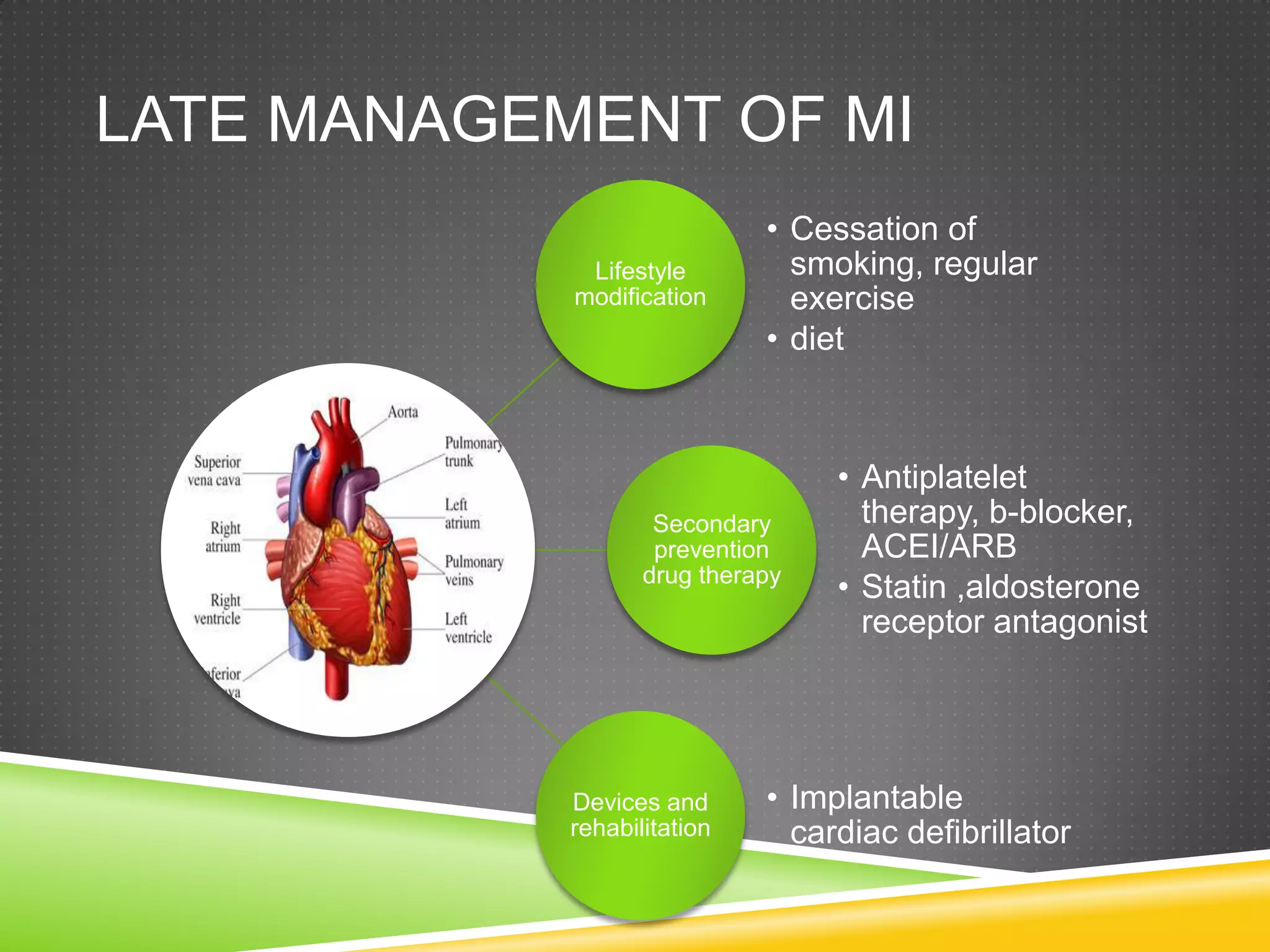
The document provides information on evaluating and managing patients presenting with chest pain and acute coronary syndrome. It discusses how to take a clinical history to determine the nature and cause of chest pain. Differential diagnoses are provided for cardiac and non-cardiac causes. Acute coronary syndrome is described as encompassing unstable angina, NSTEMI, and STEMI, which present with chest pain at rest or minimal exertion due to plaque rupture or erosion in coronary arteries. Immediate management in the first 12 hours and long-term management are outlined.