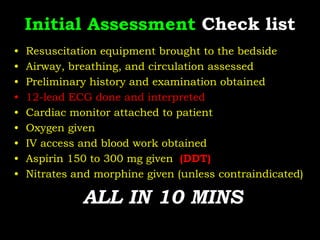
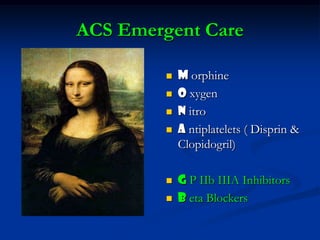
1. A patient presented to the emergency room with chest pain. Initial assessment included ECG, cardiac monitoring, bloodwork, oxygen, aspirin, and morphine if not contraindicated.
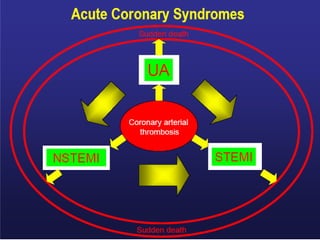
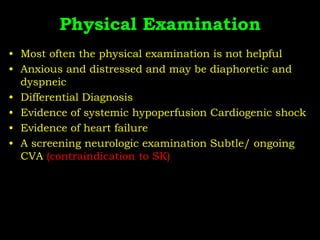
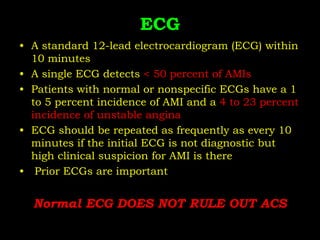
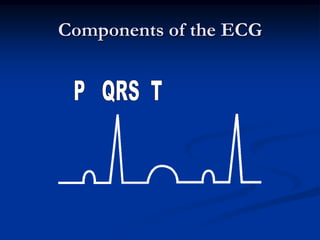
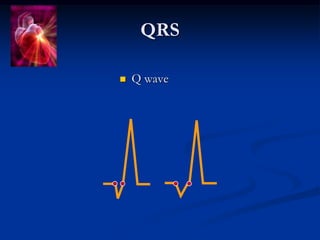
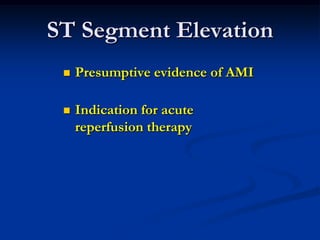
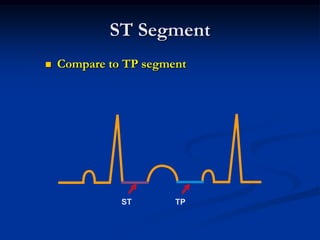
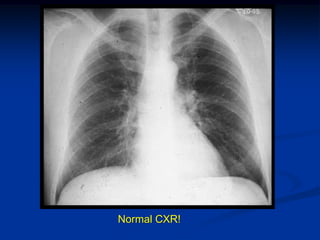
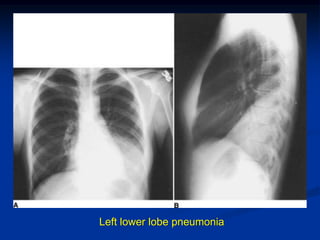
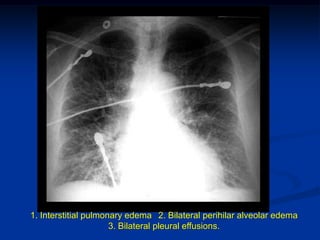
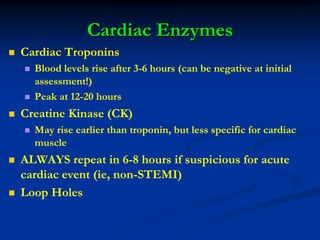
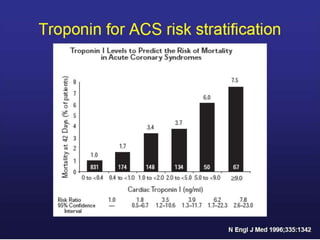
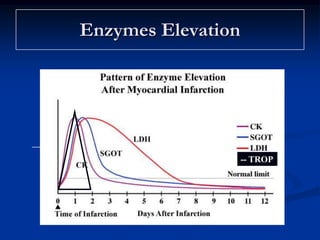
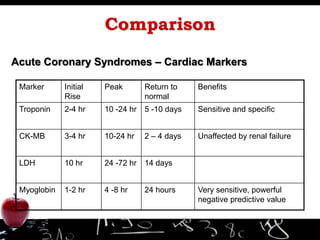
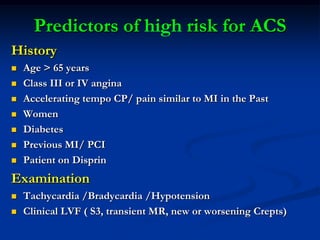
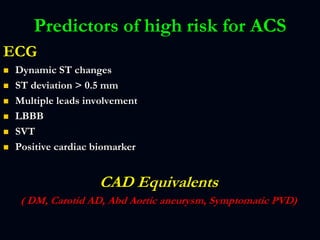
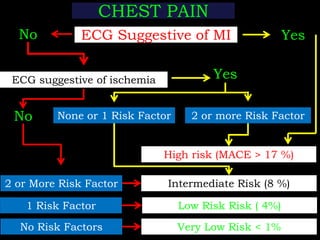
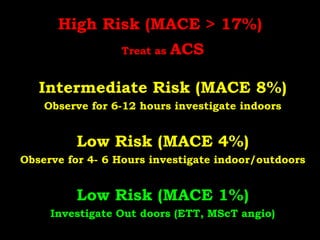
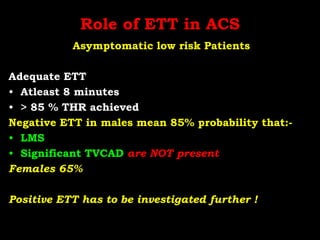
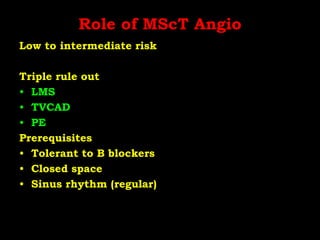
2. Further evaluation depended on risk level based on history, exam, ECG findings, and cardiac enzymes. Low risk patients could be evaluated as outpatients, while higher risk patients required inpatient monitoring and treatment for acute coronary syndrome.
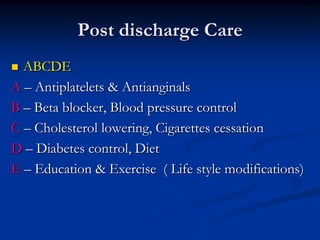
3. Ongoing management after discharge focused on lifestyle modifications like smoking cessation, exercise, diet, and medication adherence to control risk factors and prevent future events.