Embed presentation




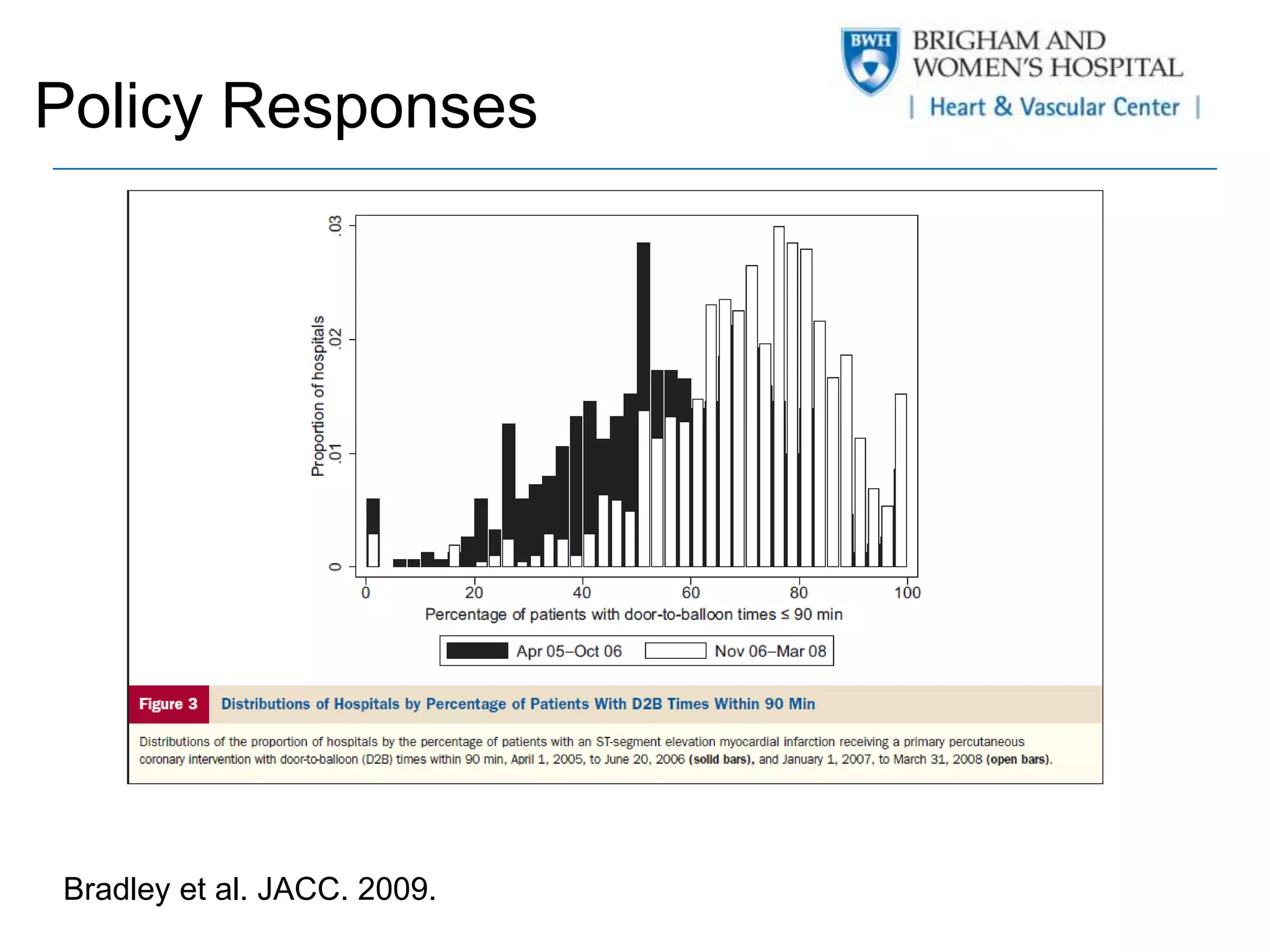

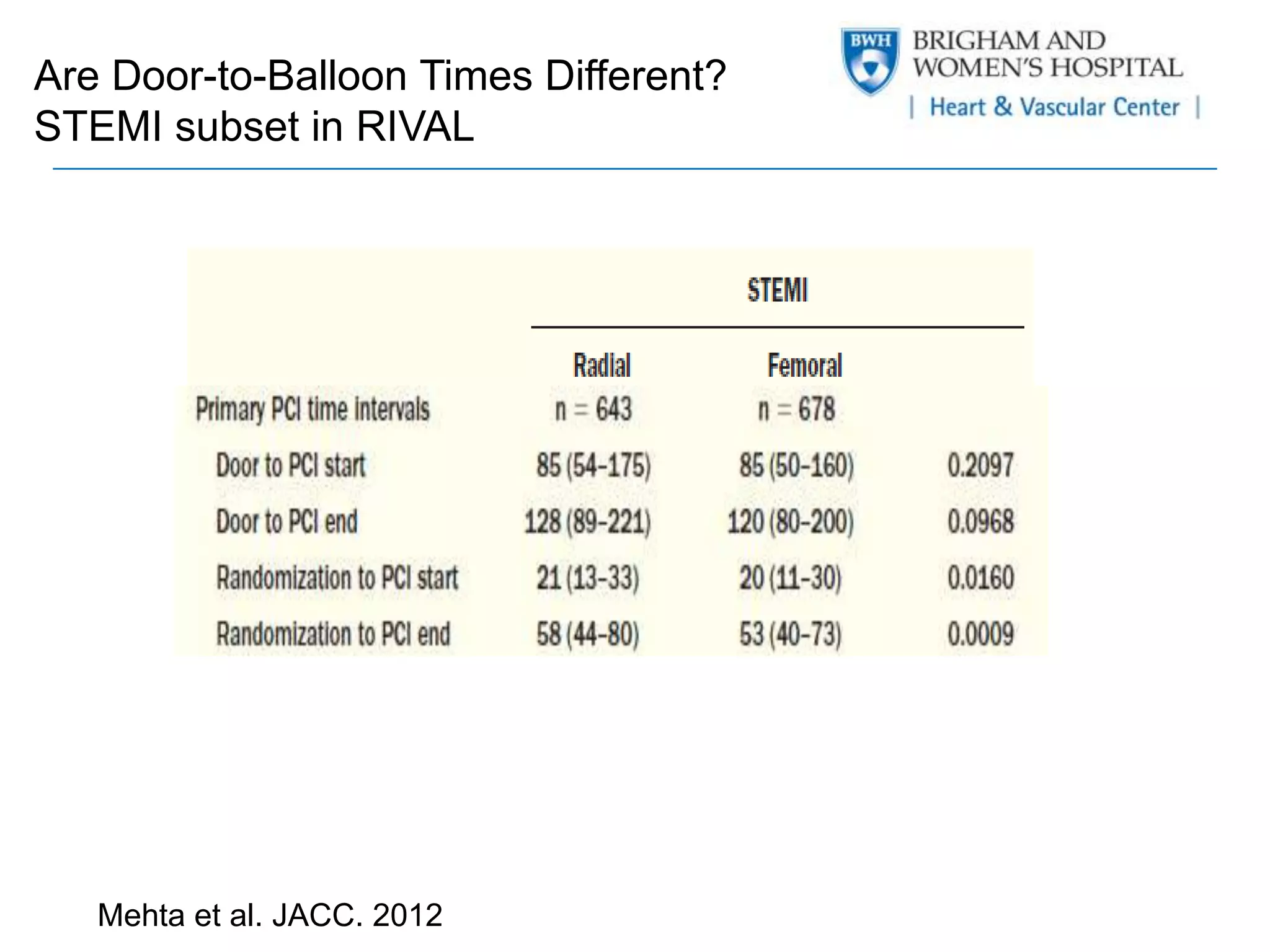



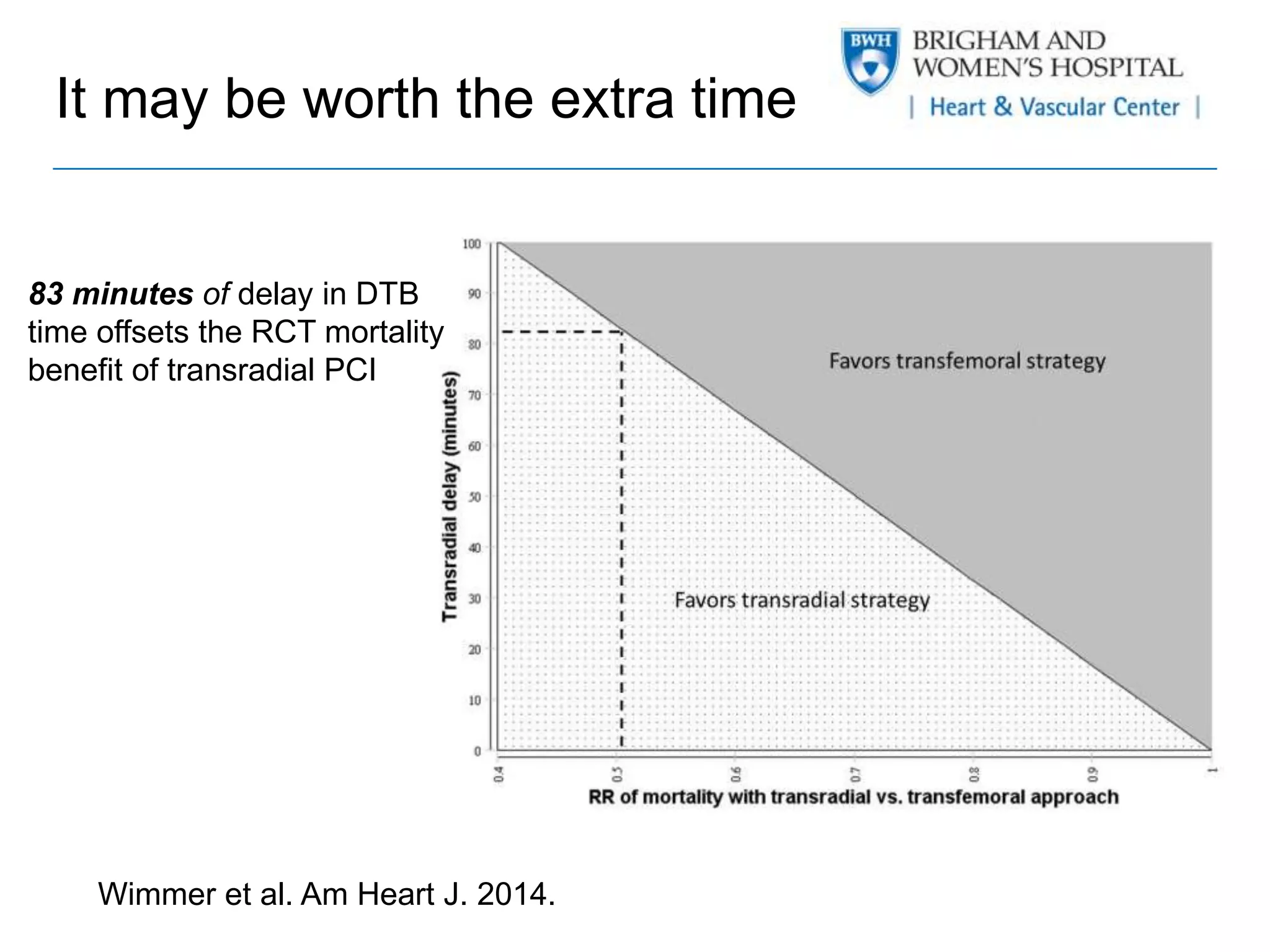
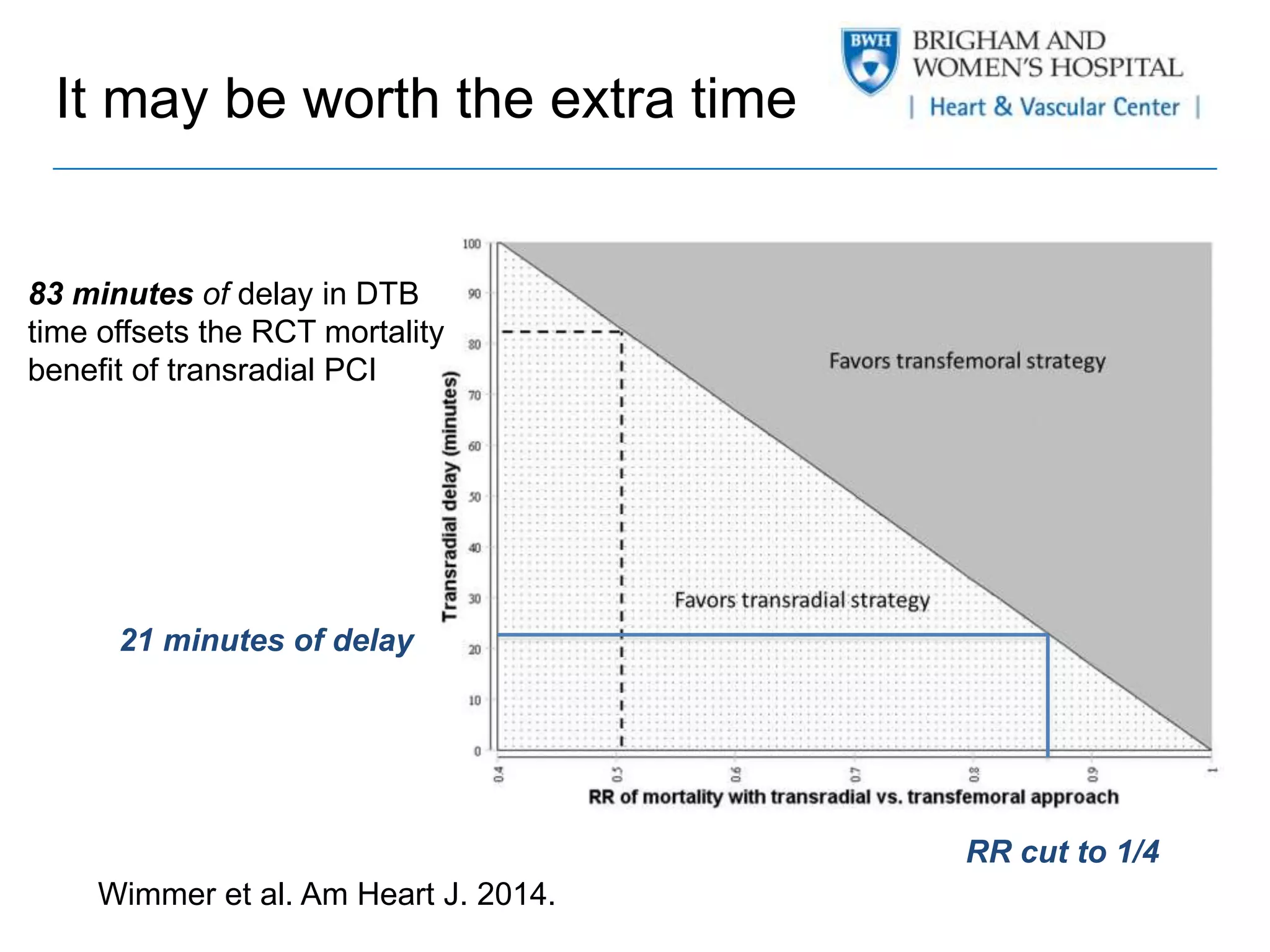


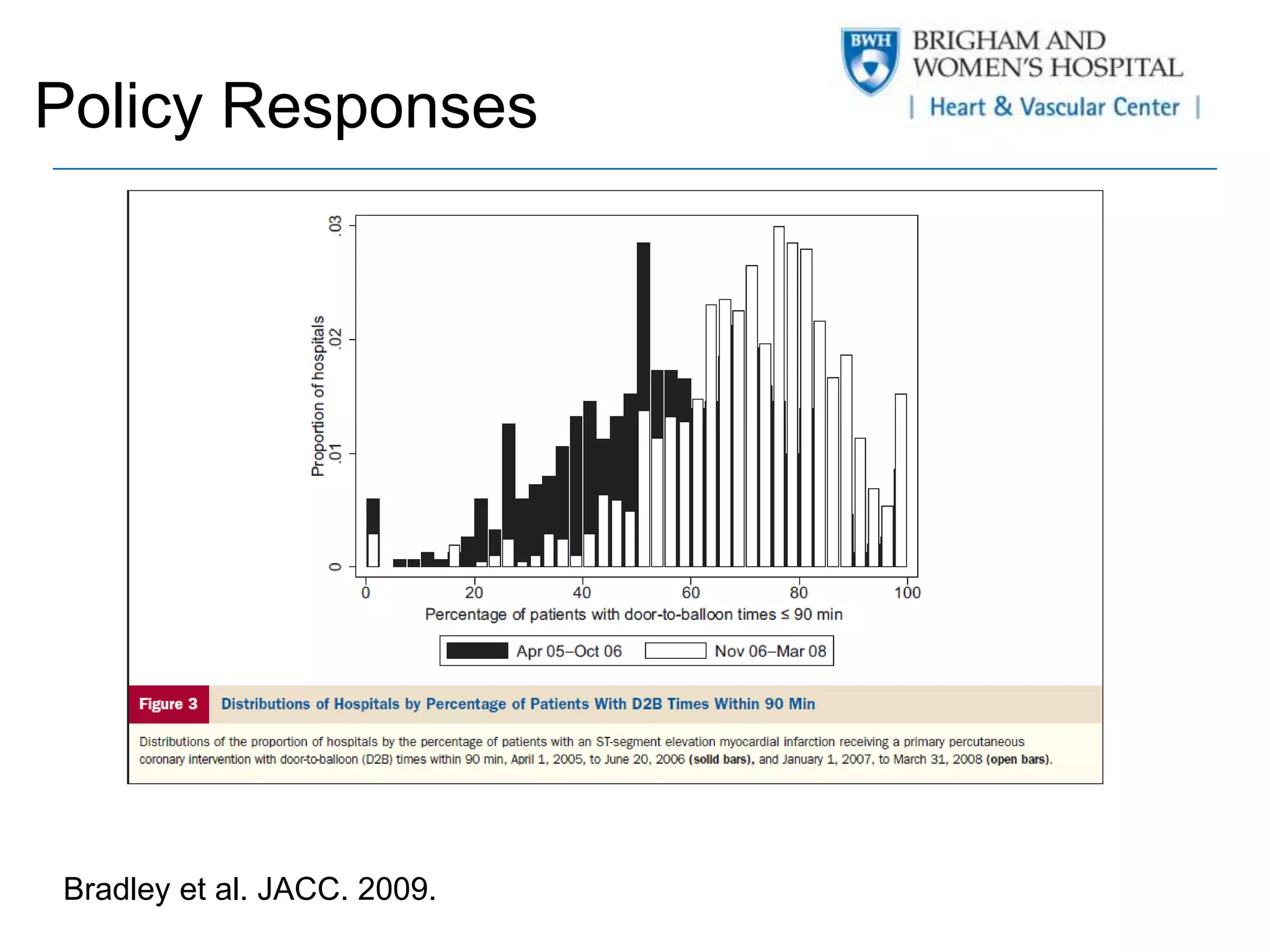
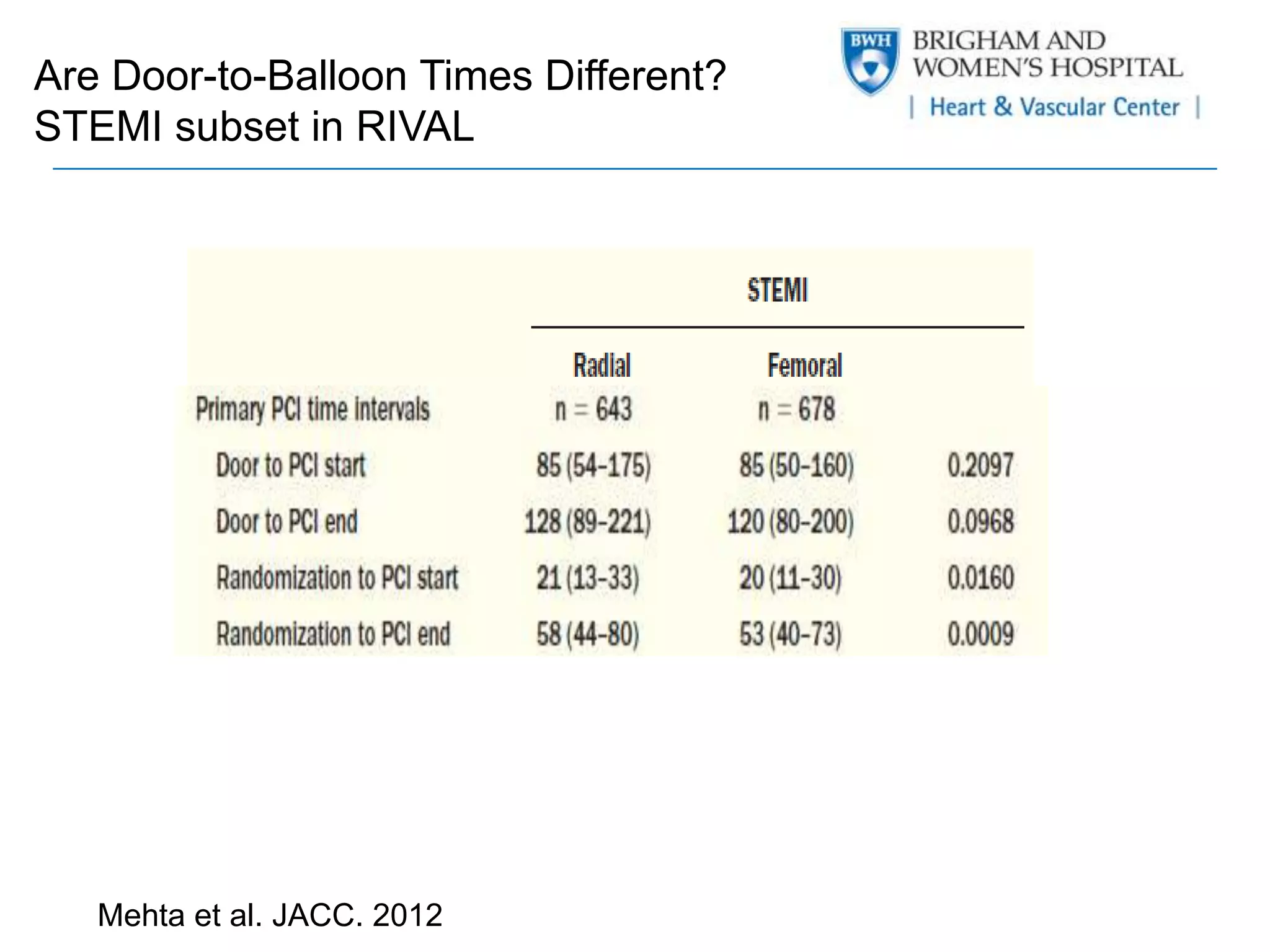
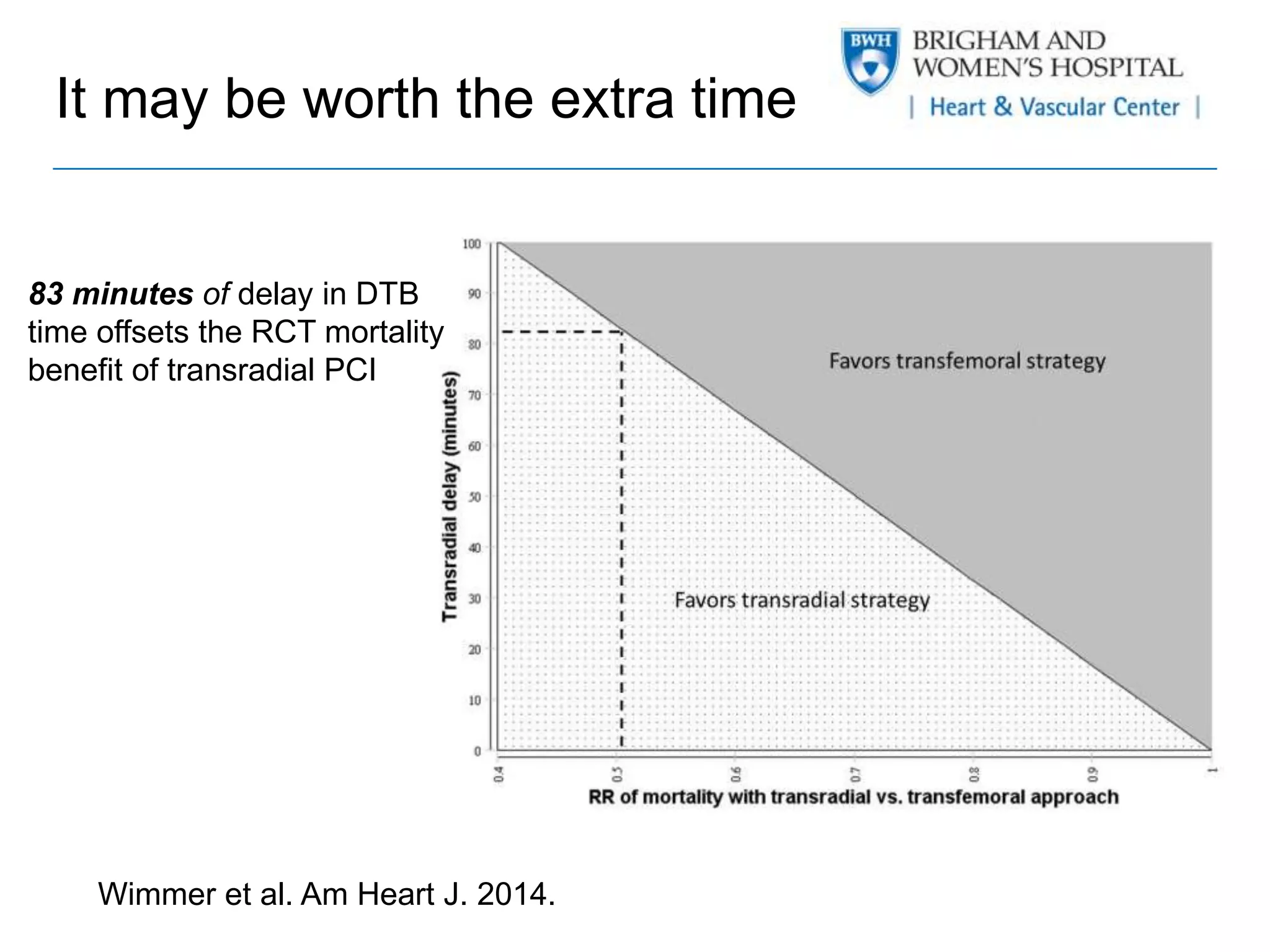
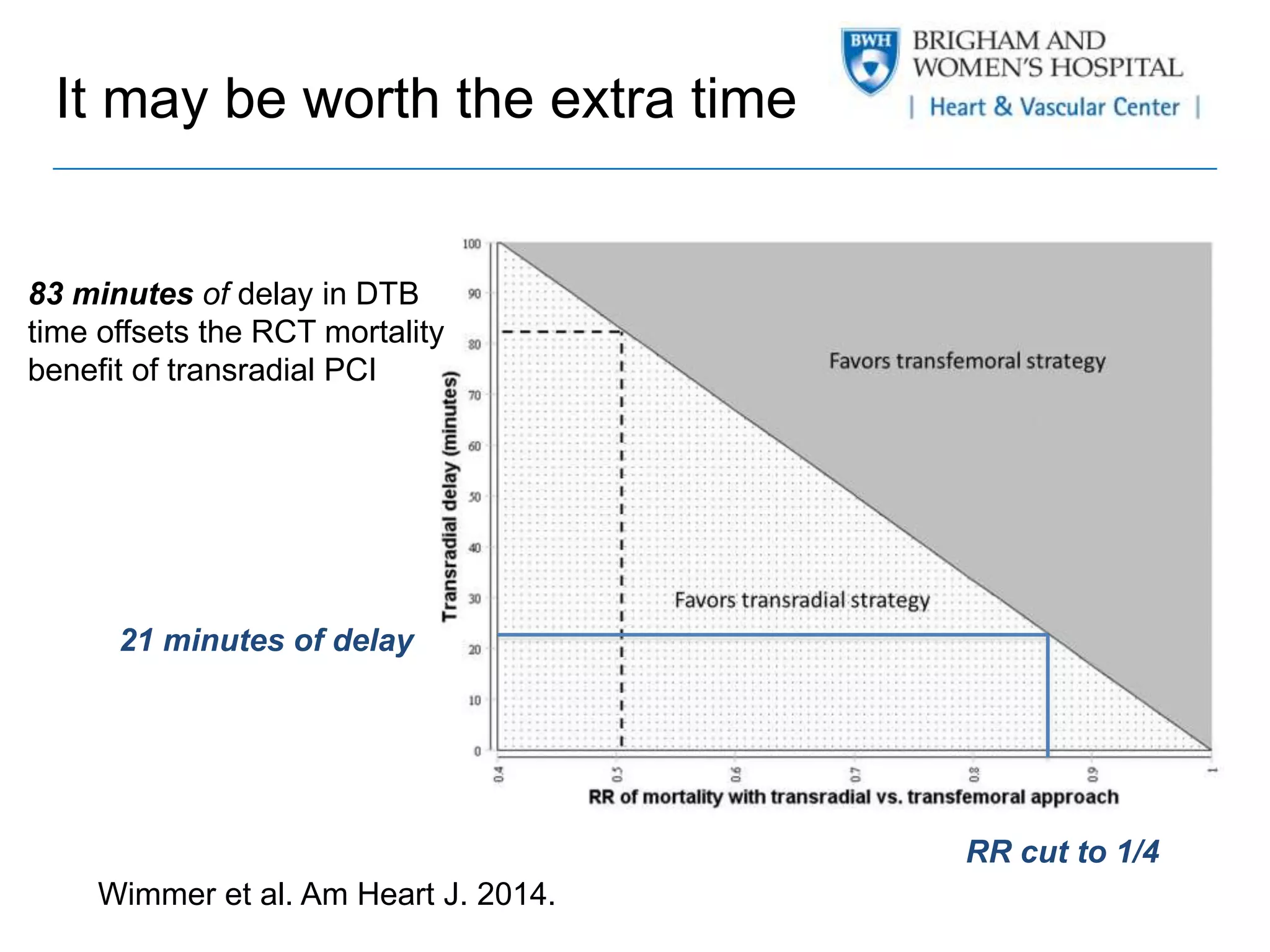
This document discusses radial PCI and door-to-balloon time for STEMI patients. It notes that while radial PCI is associated with less bleeding and faster recovery, it can also lead to longer procedure times. The document summarizes several studies that have looked at the mortality benefits of radial PCI for STEMI. A key study found that even with an 83 minute delay in door-to-balloon time, radial PCI was still associated with lower mortality based on results from randomized controlled trials. The conclusion is that the benefits of radial PCI outweigh the risks associated with potential delays, and radial PCI should be the preferred approach.