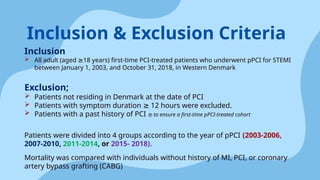
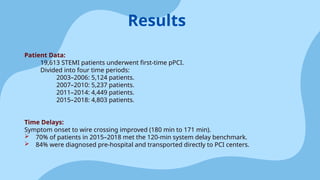
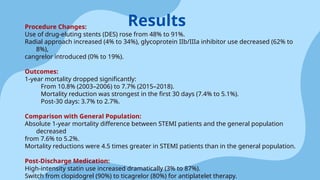
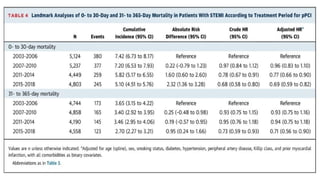
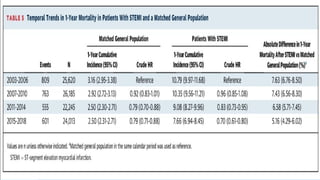
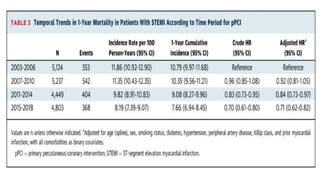
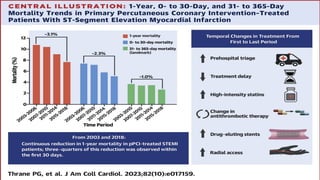
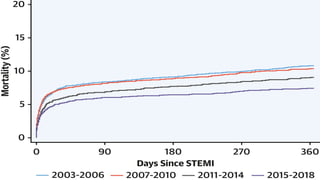
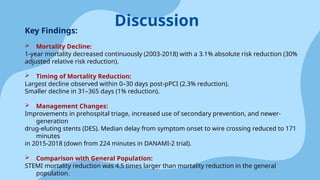
A cohort study conducted in Denmark from 2003 to 2018 examined mortality trends after primary percutaneous coronary intervention (PPCI) for ST-elevation myocardial infarction (STEMI). It found a significant decrease in 1-year mortality rates, dropping from 10.8% to 7.7%, with the most remarkable reduction occurring within the first 30 days post-intervention. Key factors contributing to this decline included improved treatment delays, increased use of drug-eluting stents, and the adoption of newer antiplatelet medications.