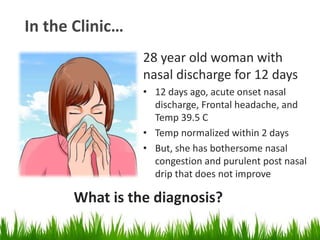
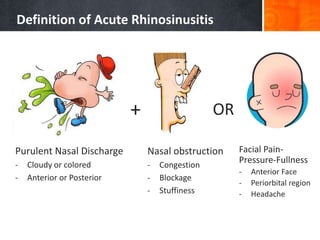
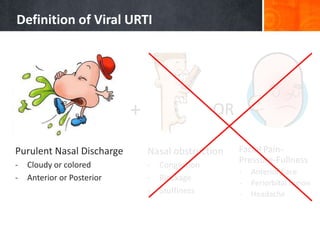
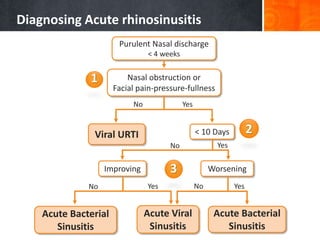
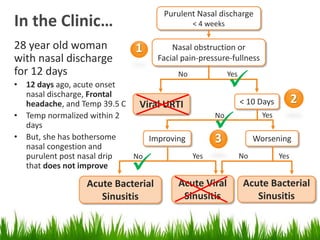
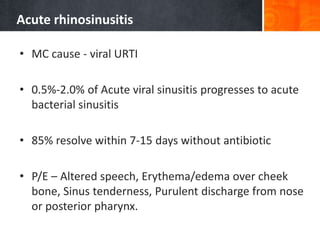
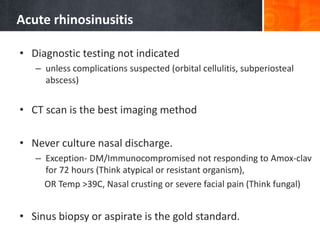
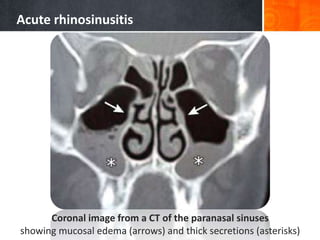
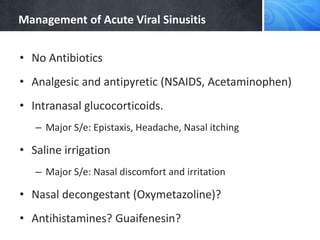
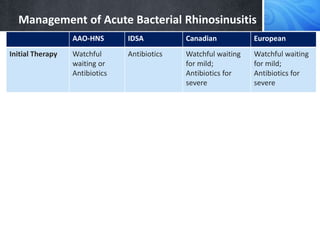
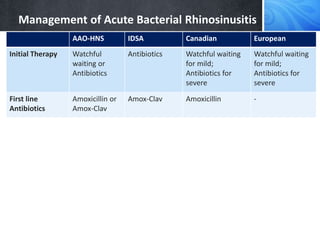
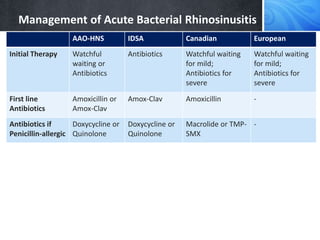
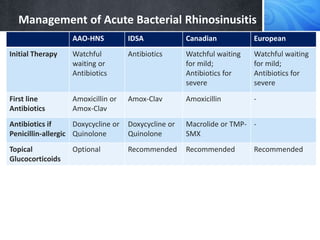
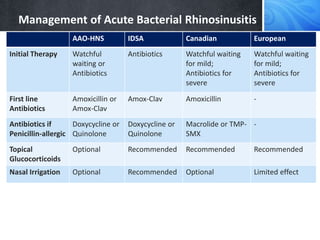
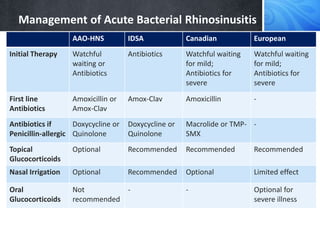
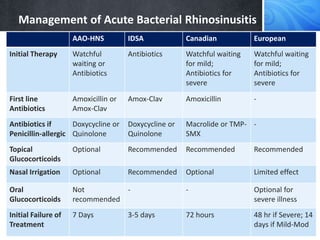
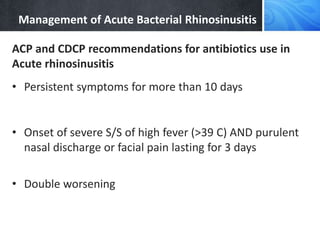
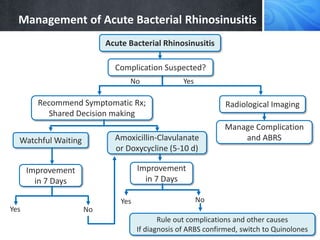
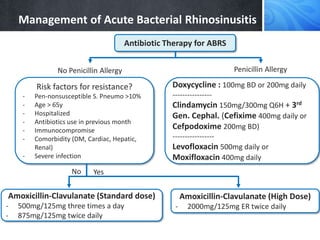
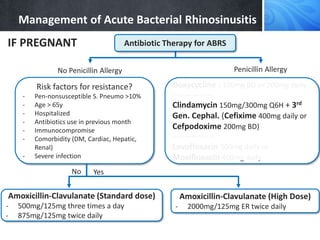
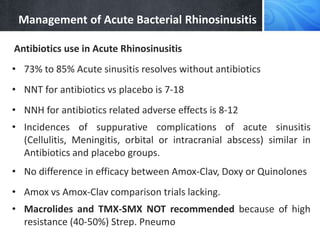
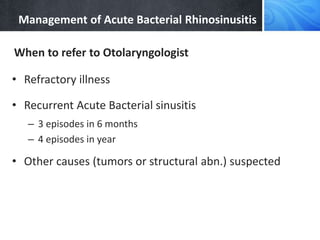
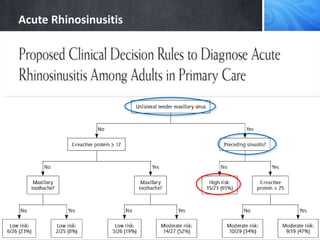
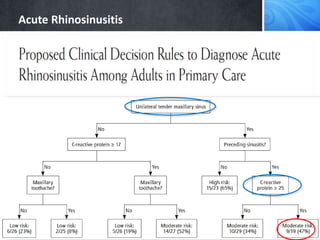
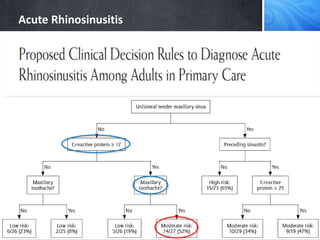
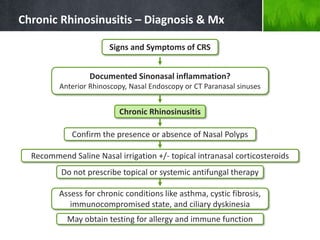
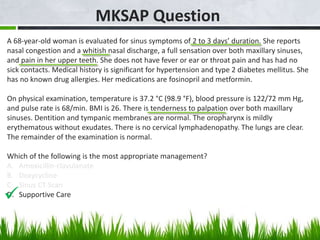
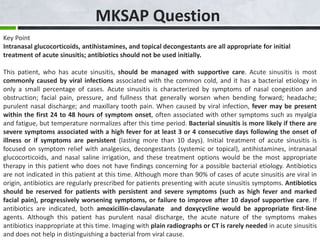
The document discusses the diagnosis and management of acute bacterial rhinosinusitis, defining the classification and diagnosis of rhinosinusitis. It provides guidelines from various medical organizations on the initial treatment of acute bacterial rhinosinusitis with antibiotics such as amoxicillin-clavulanate, as well as the use of nasal irrigation and intranasal corticosteroids as adjunctive therapies. Failure to improve within a week of initial antibiotic therapy may require changing to a quinolone or other alternative antibiotic based on risk factors for antibiotic resistance.