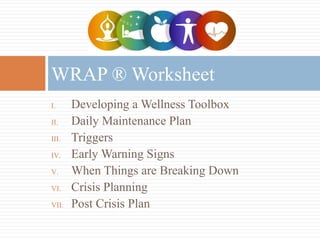
The WRAP® is a self-management and recovery system that helps individuals identify what makes them well and develop an action plan to stay well. It involves creating a WRAP® booklet with sections on developing a wellness toolbox, daily maintenance plans, identifying triggers and early warning signs, crisis planning, and post-crisis plans. The goal is for individuals to be active participants in their care by creating customized wellness tools and plans to manage their mental health in their daily lives and during crises.