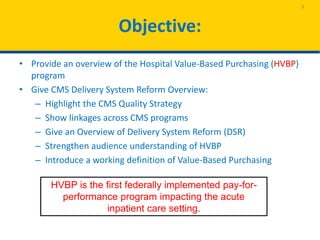
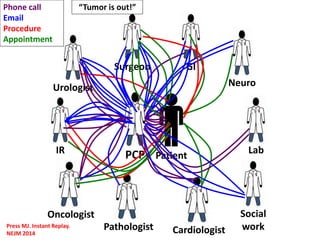
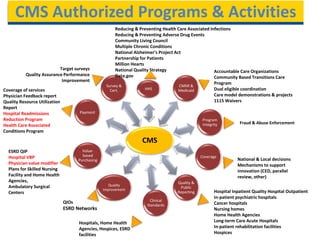
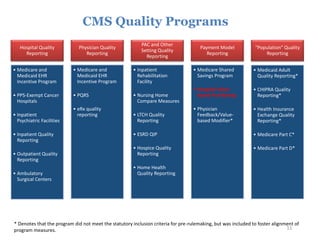
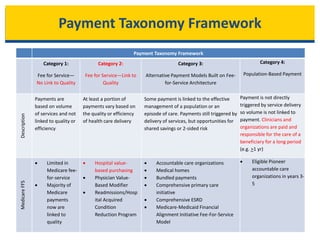
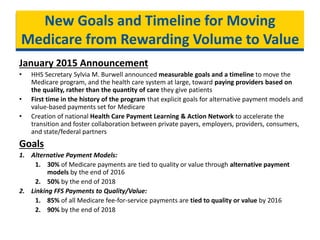
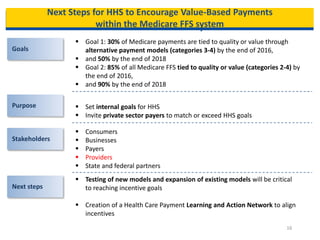
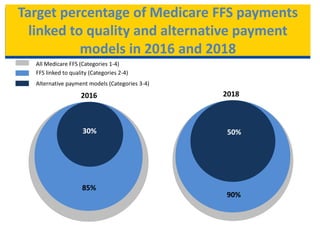
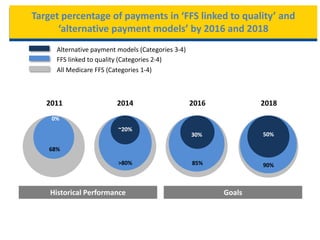
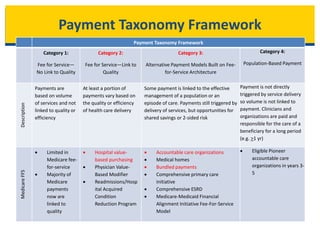
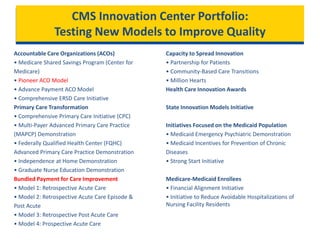
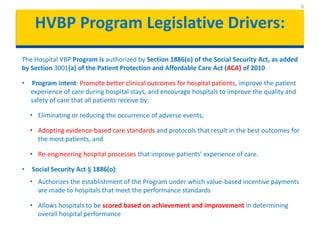
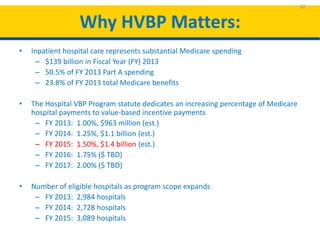
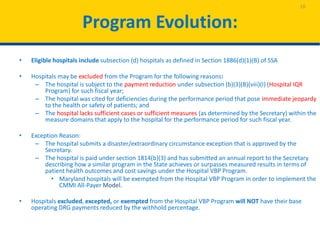
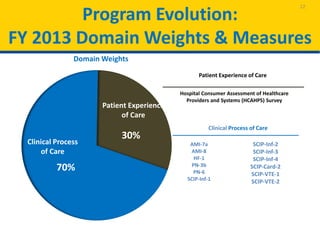
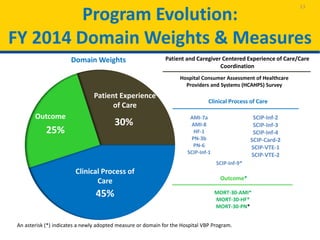
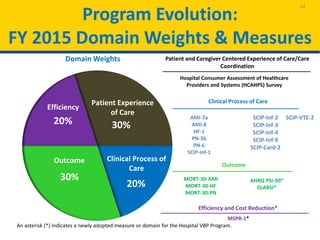
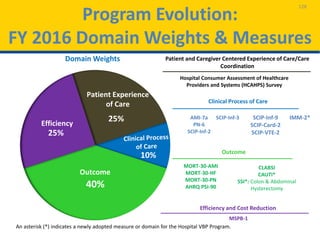
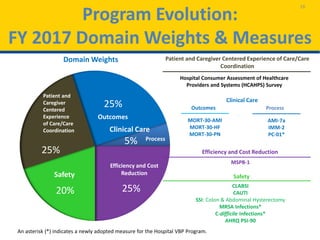
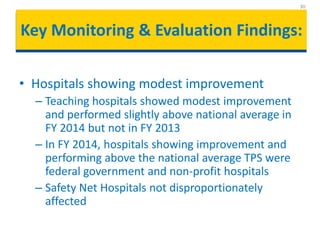
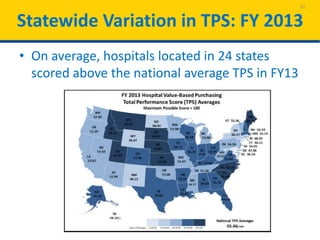
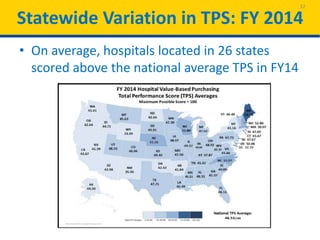
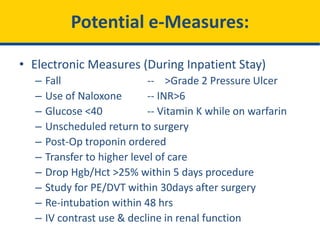
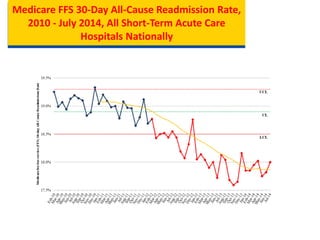
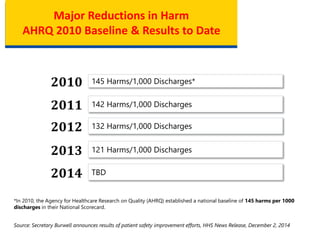
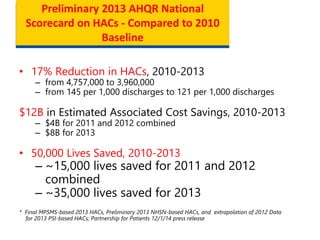
The document provides an overview of the Hospital Value-Based Purchasing (HVBP) program, which aims to enhance patient care quality and safety through value-based payments linked to performance outcomes. It discusses the objectives of the Centers for Medicare & Medicaid Services (CMS) to transition from fee-for-service to value-driven payment systems and highlights legislative drivers that authorize the HVBP program. The document emphasizes the importance of improving clinical outcomes, patient experiences, and hospital processes to achieve better health delivery and cost efficiency.