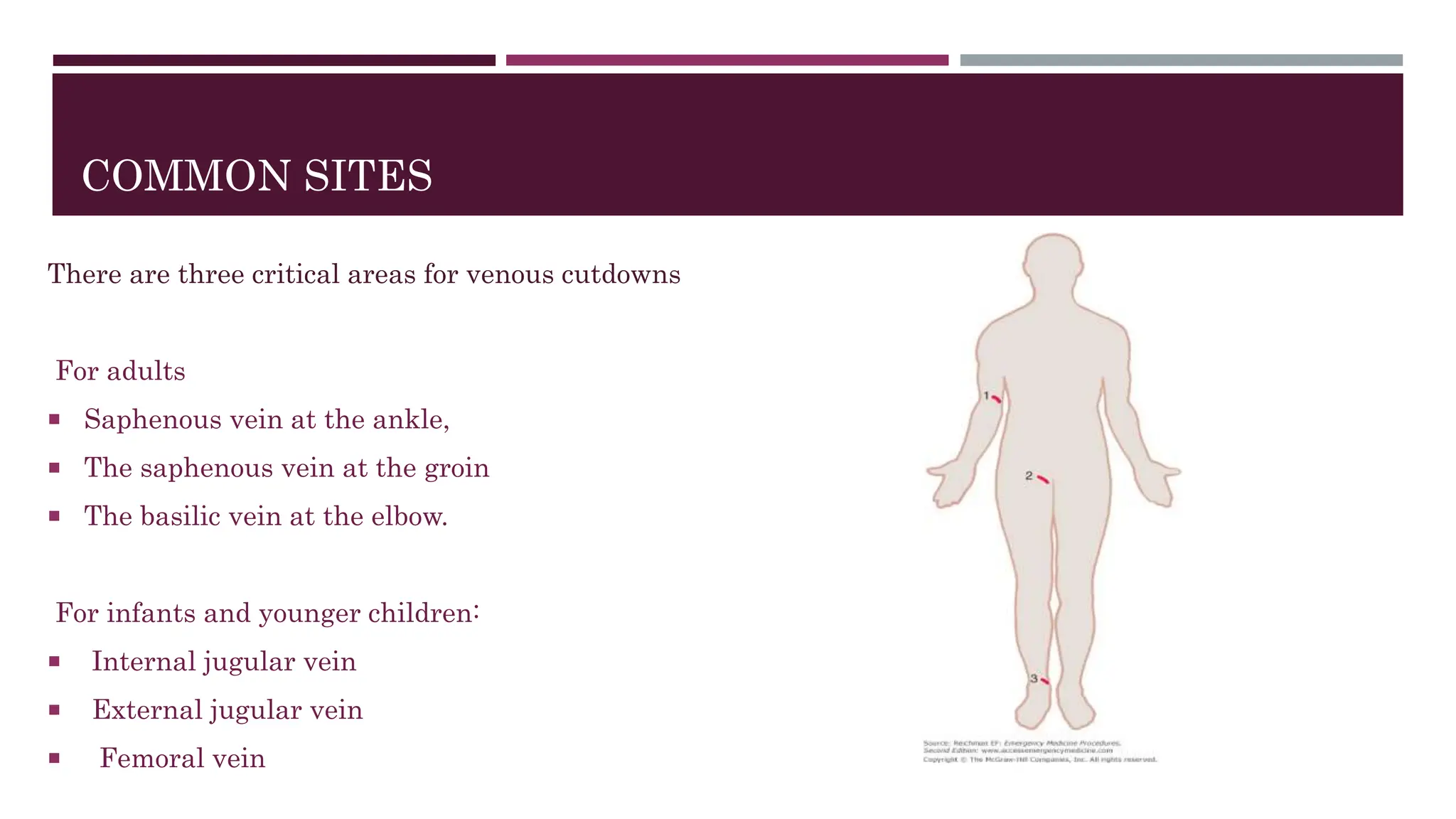
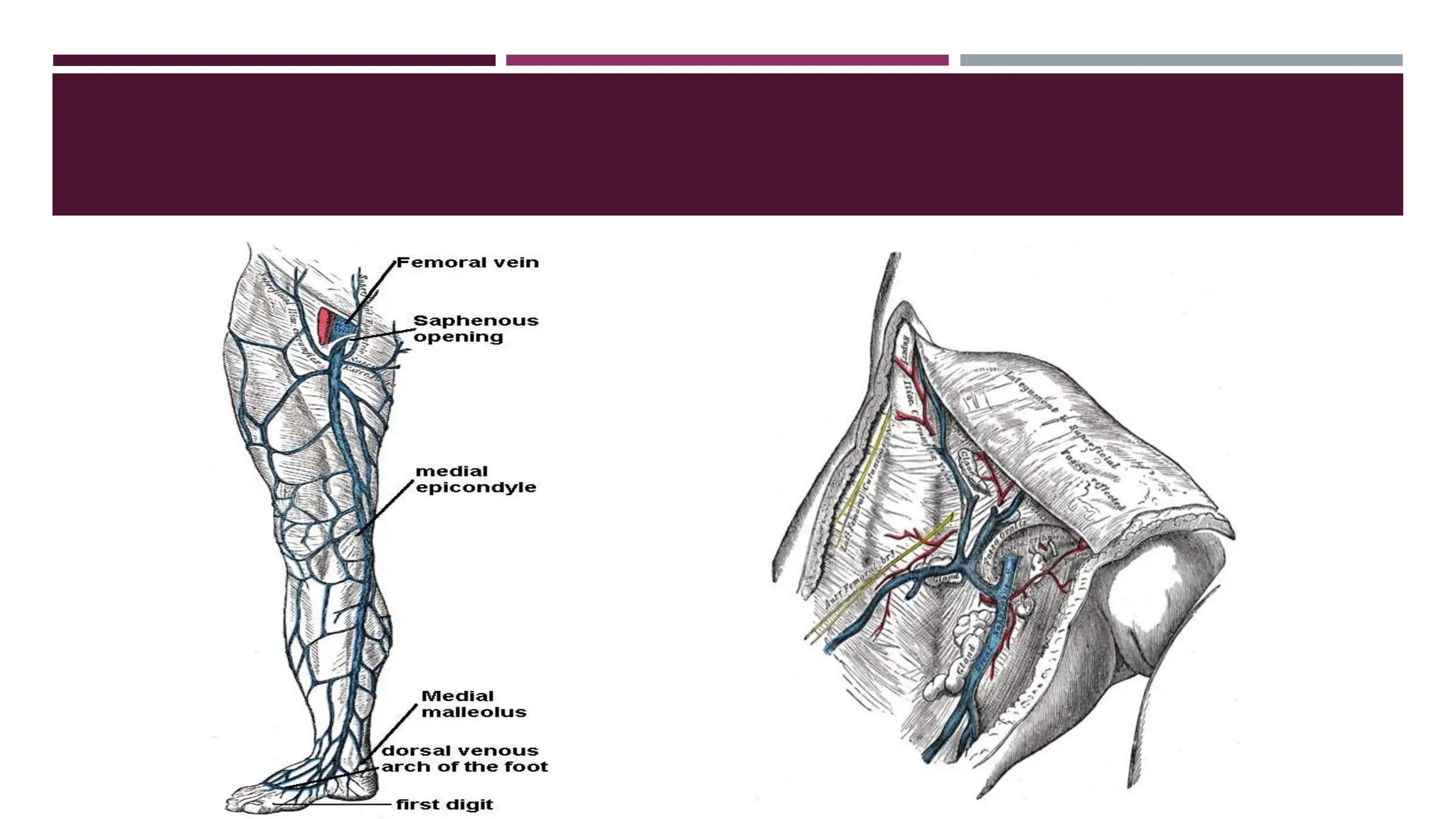
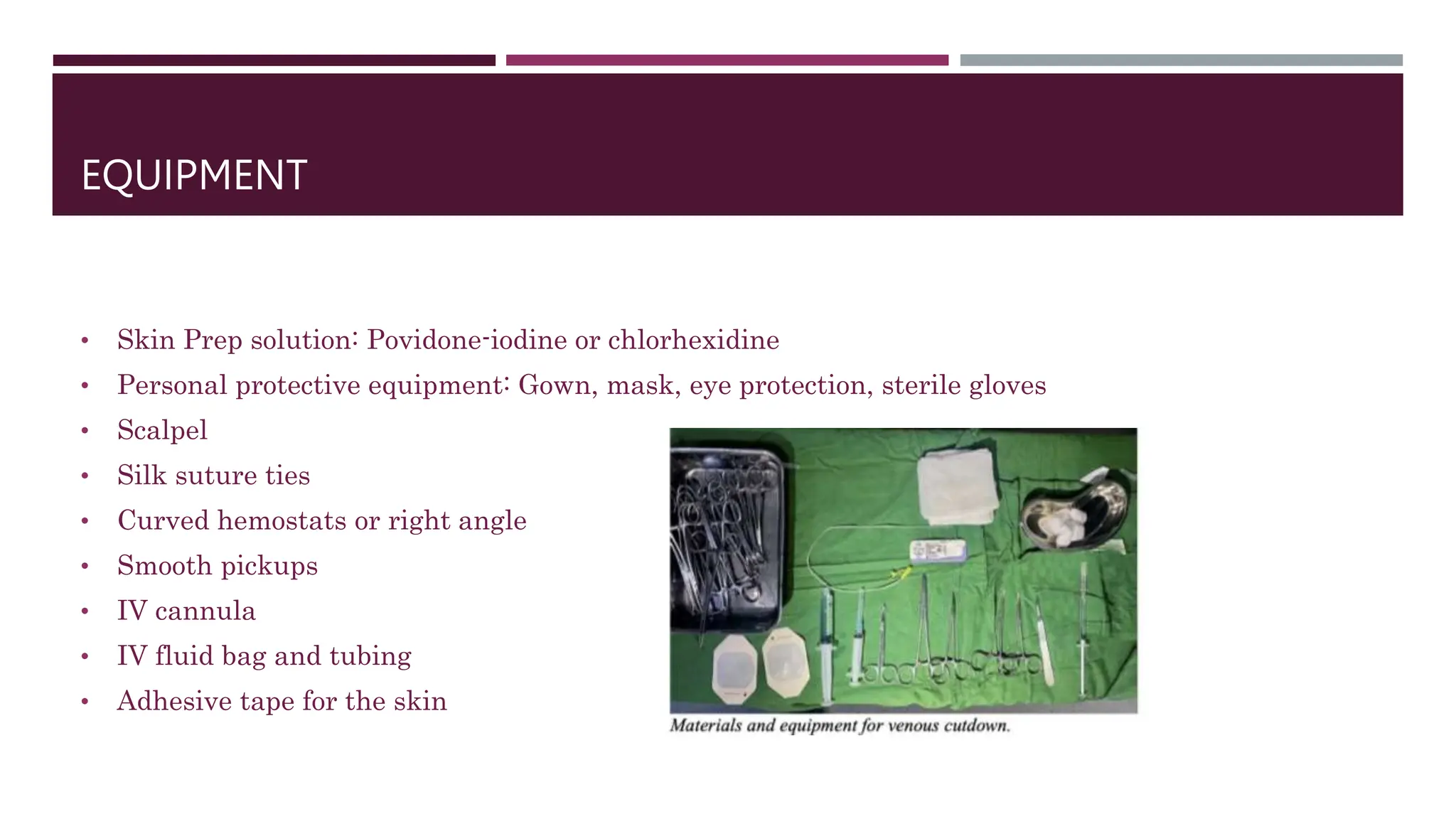
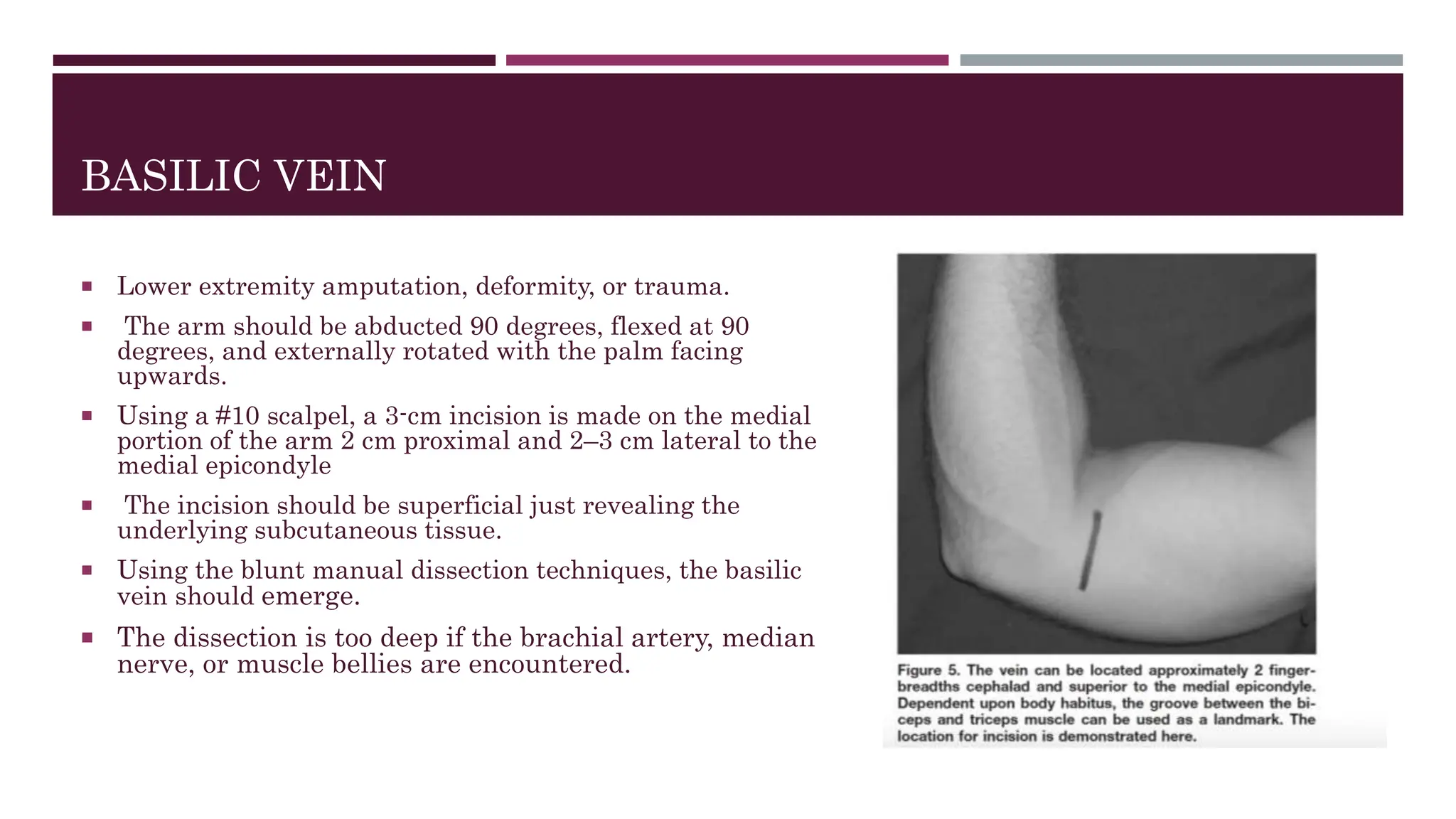
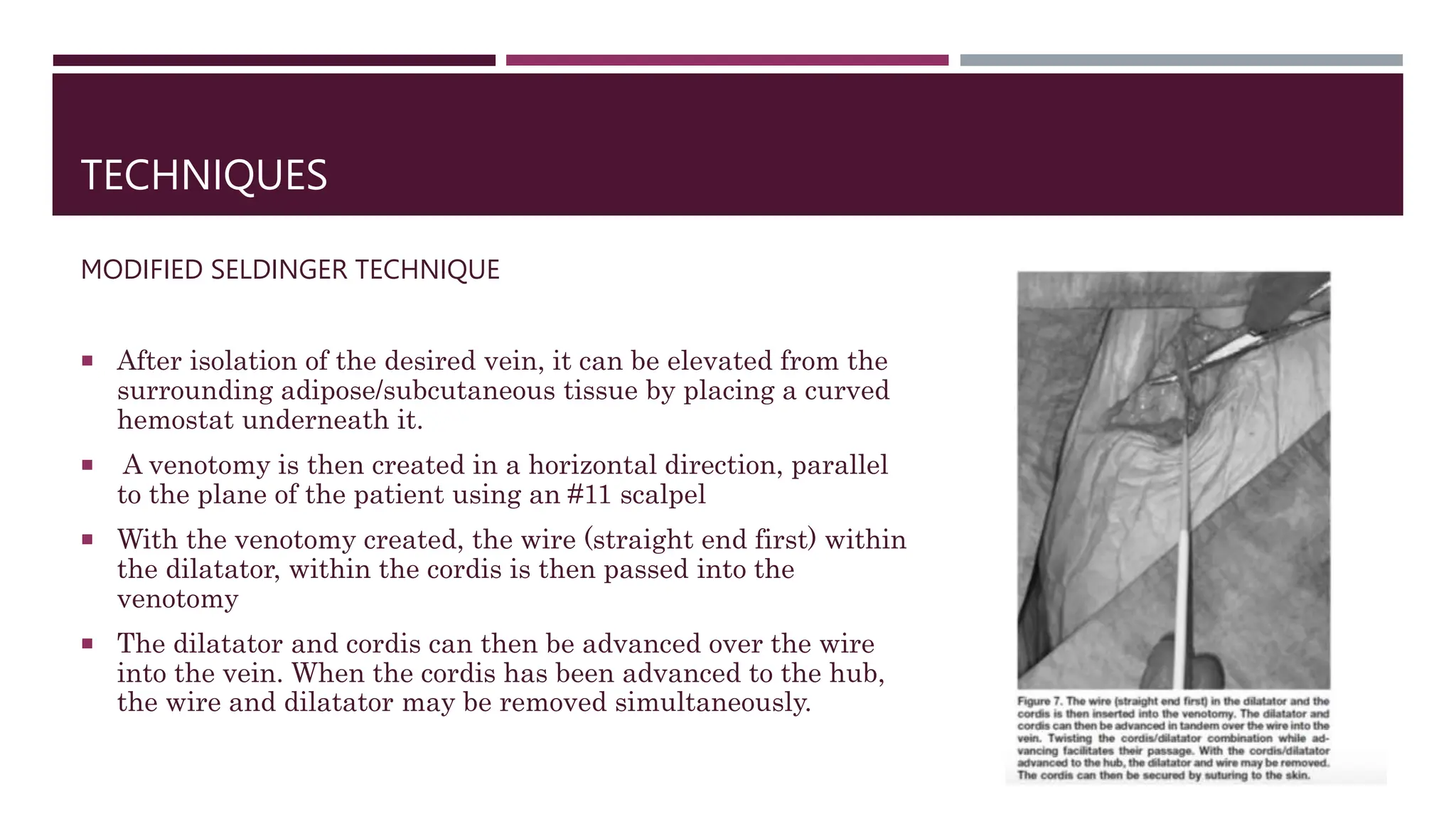
The document provides a comprehensive overview of the venous cutdown technique, essential for medical professionals dealing with critically ill patients where traditional venous access may be challenging. It details indications, contraindications, equipment needed, and step-by-step procedures for accessing the greater saphenous vein at both the ankle and groin. Complications and alternative techniques are also discussed, highlighting the importance of this method in emergency situations.