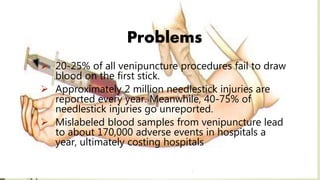
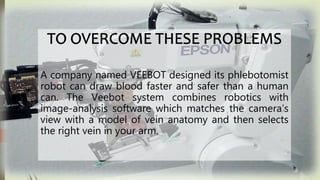
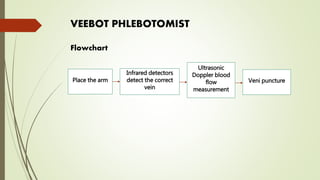
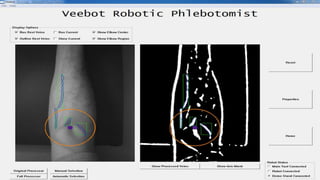
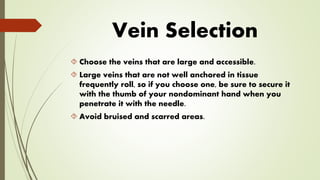
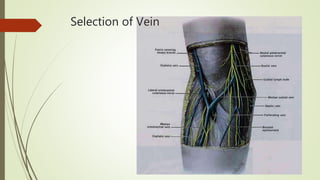
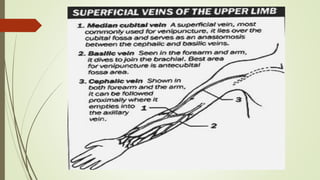
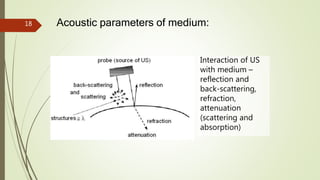
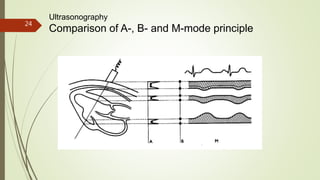
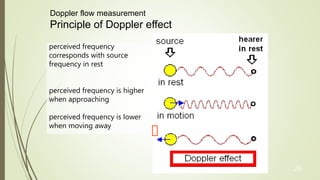
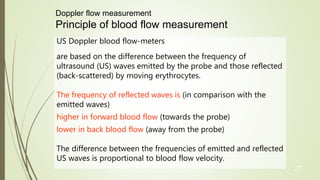
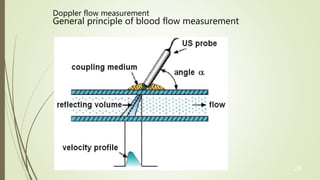
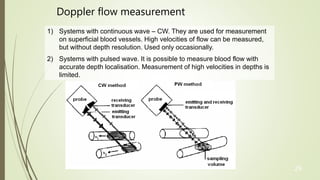
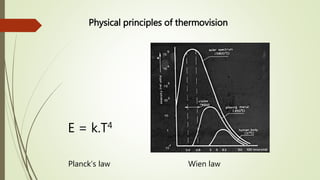
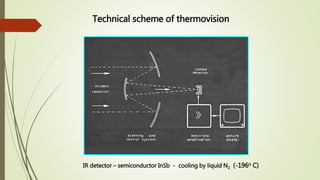
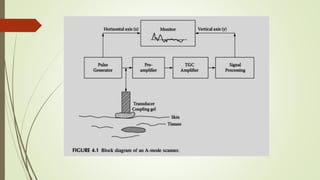
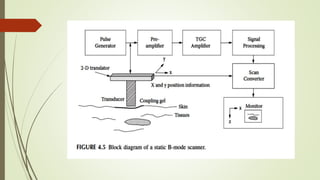
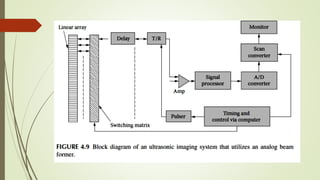
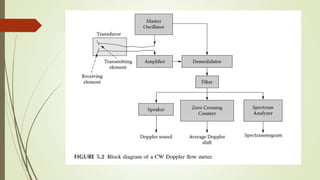
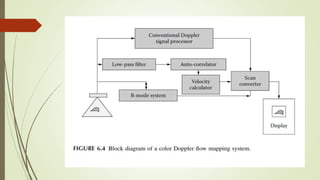
This document discusses the role and training of phlebotomists, highlighting the challenges they face and the introduction of a robotic phlebotomist, Veebot, which aims to automate blood drawing to minimize errors and enhance patient care. It outlines the selection process for veins and describes the Veebot system's functioning, including its use of ultrasound for vein detection. Additionally, the document touches on ultrasound properties and Doppler flow measurement principles, linking them to clinical applications like thermovision and imaging of blood flow.