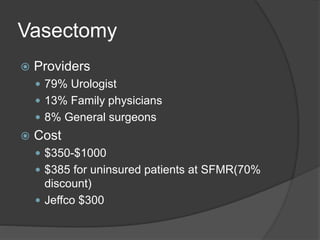
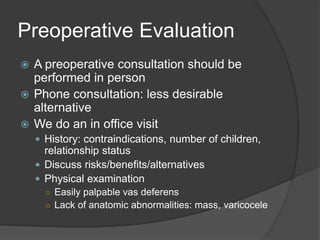
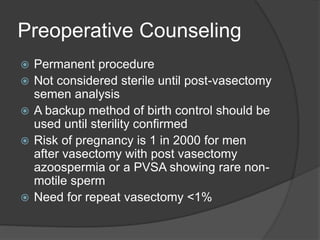
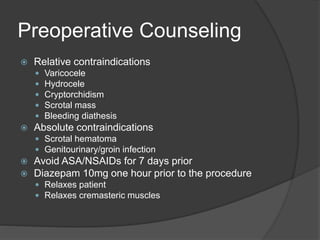
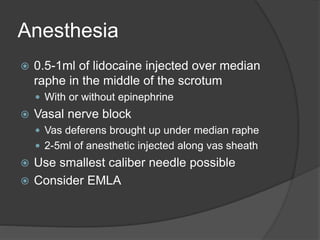
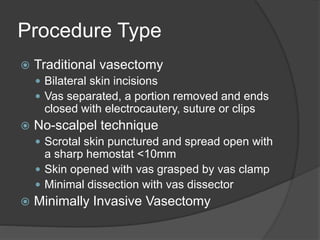
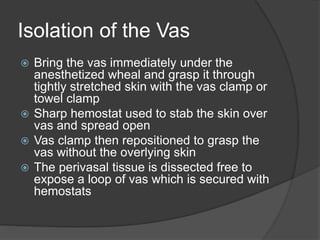
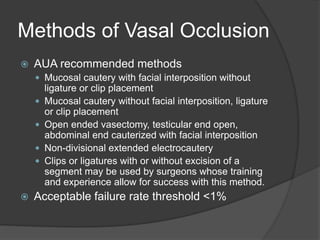
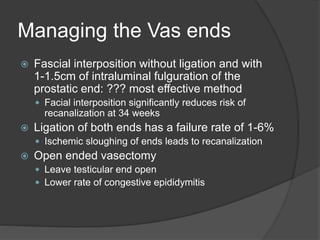
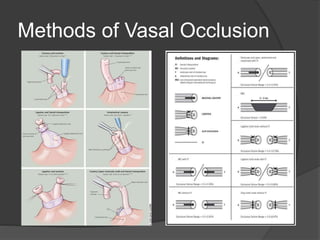
This document provides guidance on performing vasectomies, including preoperative evaluation and counseling, the no-scalpel technique, managing the vas ends, follow-up care, and complications. It emphasizes the importance of thorough patient selection, counseling, and use of the minimally invasive no-scalpel method to reduce risks and optimize outcomes.