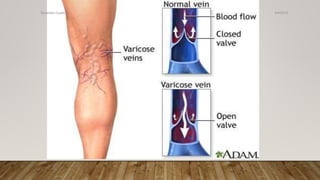
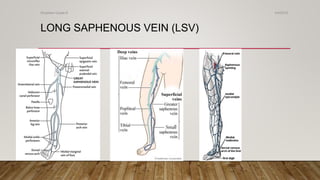
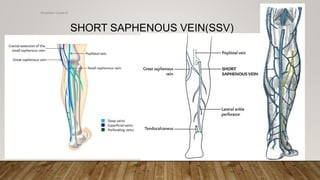
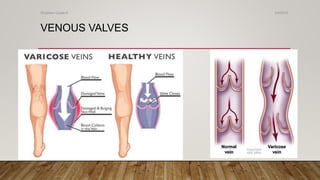
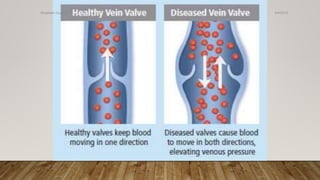
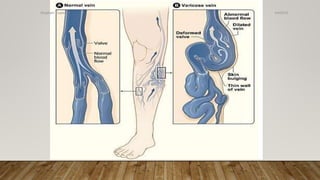
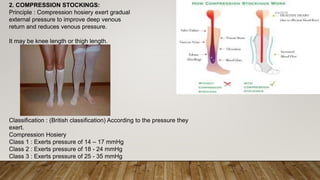
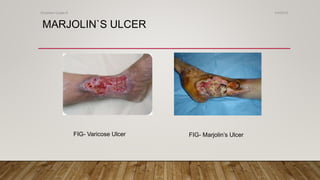
Varicose veins are dilated, swollen leg veins caused by incompetent valves in the veins. This allows blood to flow backward and pool in the veins. Varicose veins most commonly affect the saphenous vein and its branches in the legs. A duplex ultrasound scan is often used to examine the veins and identify areas of reflux or blockage. Treatment options depend on the severity and location of the varicose veins.