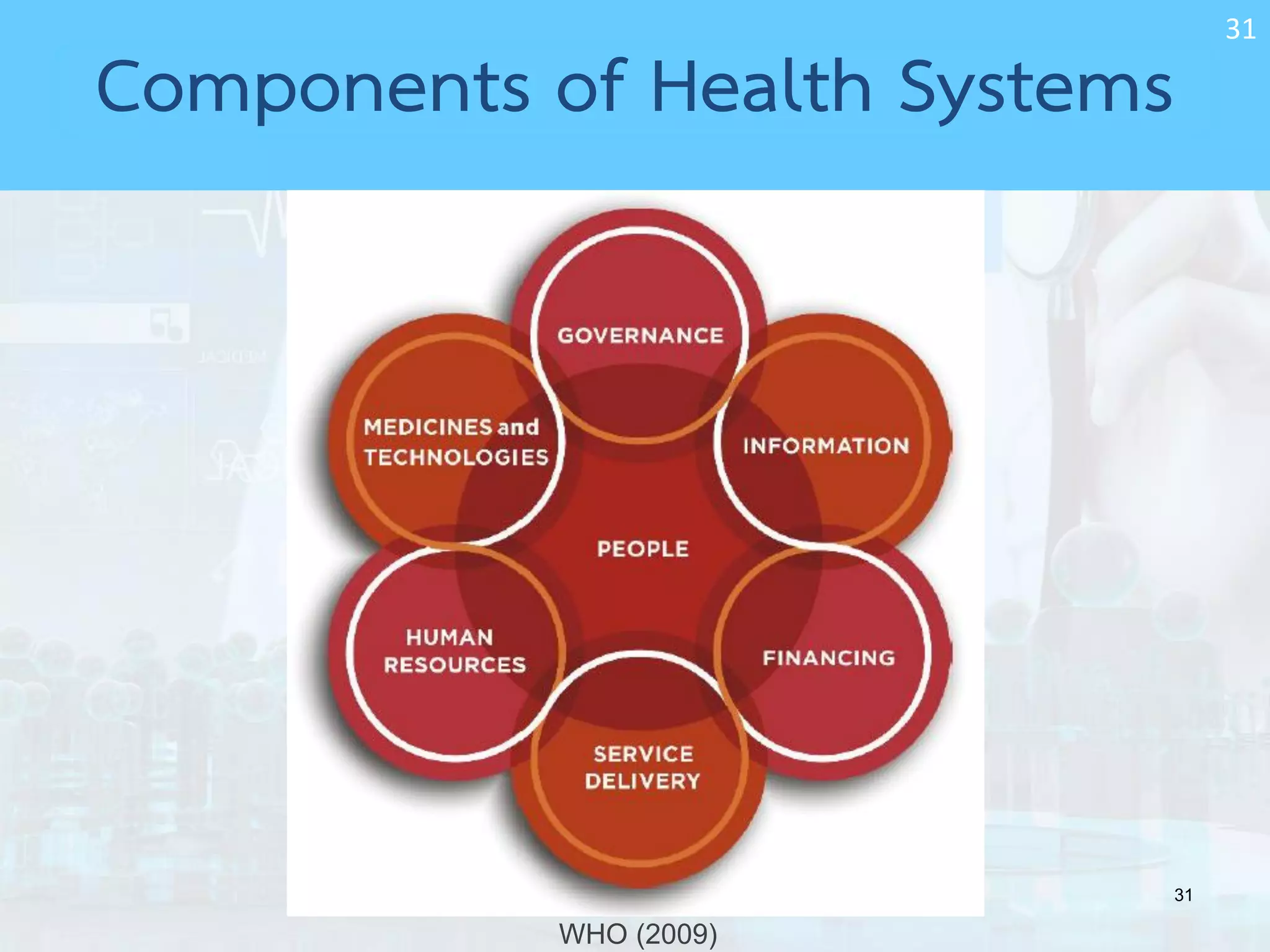
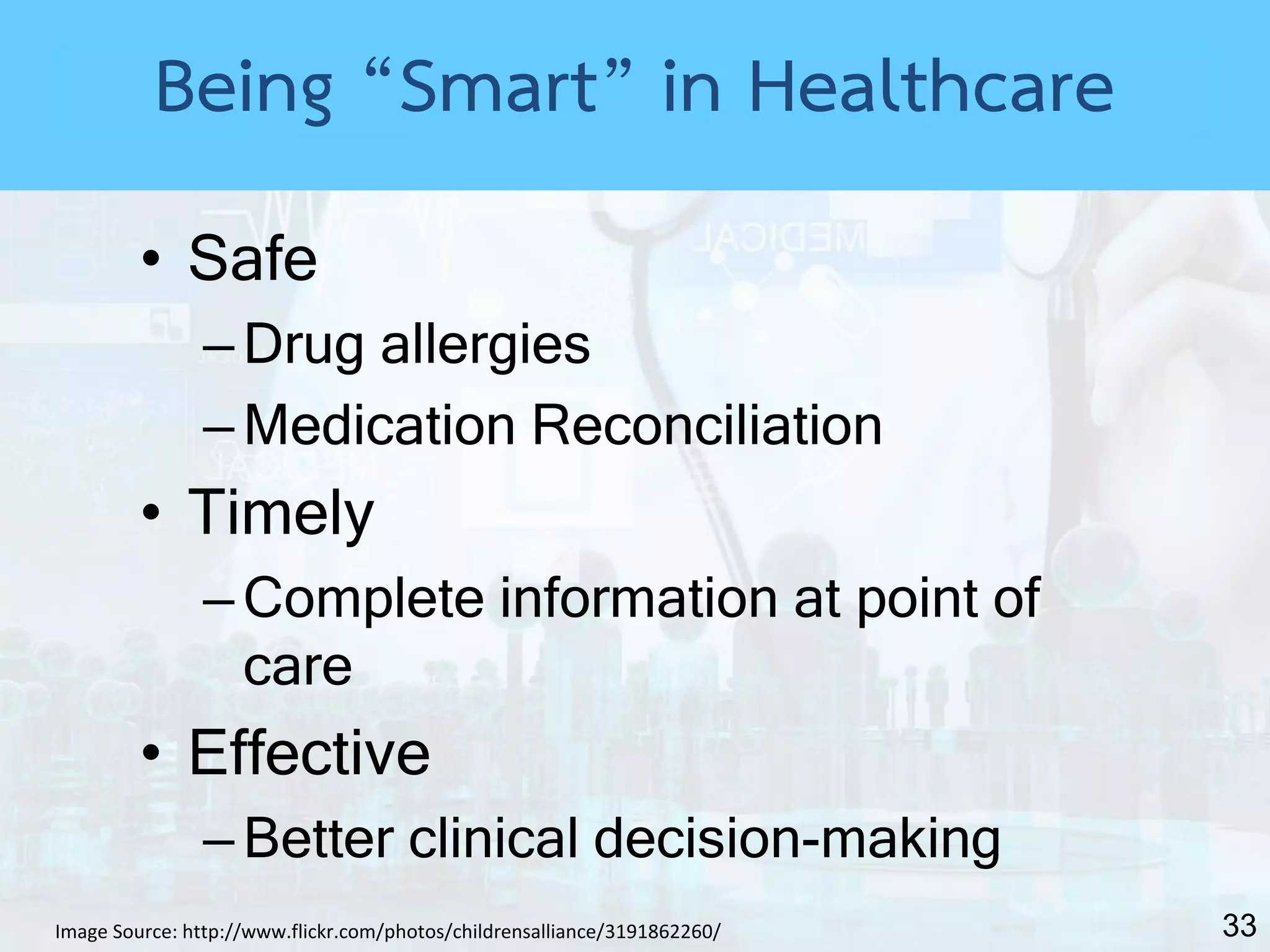
A document discusses introducing information technology systems into healthcare services. It begins by introducing the speaker, Dr. Nawanan Theeramamphorn, who has a PhD in health informatics. The presentation then outlines the topics to be covered, including the road to digitizing healthcare, what a "smart hospital" is, and how to move toward a smart hospital.