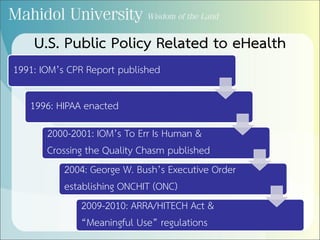
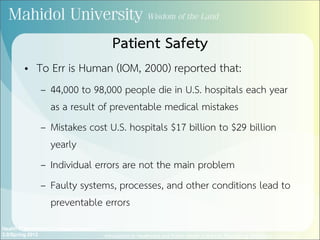
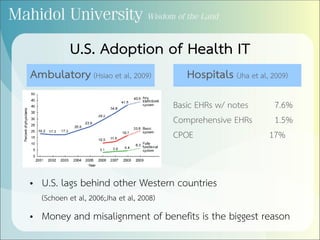
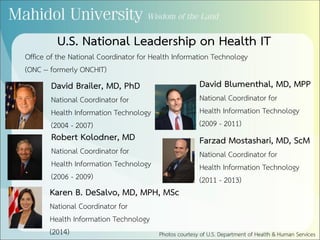
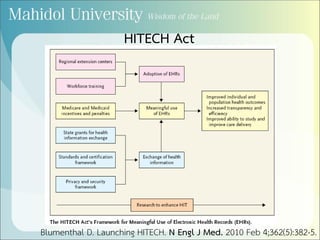
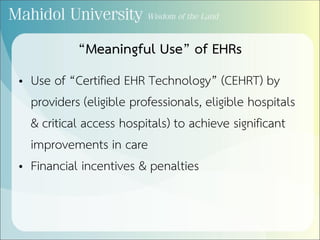
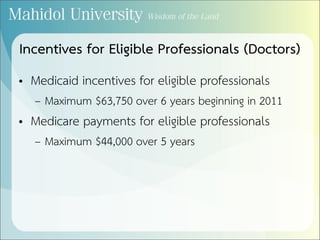
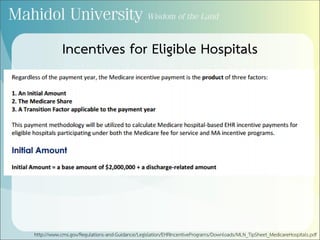
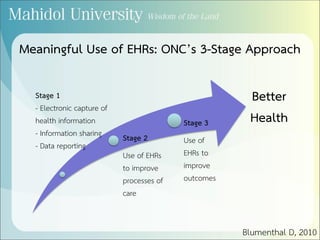
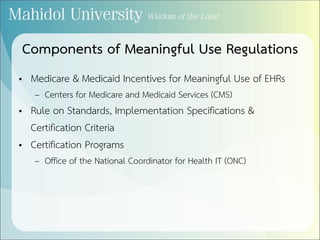
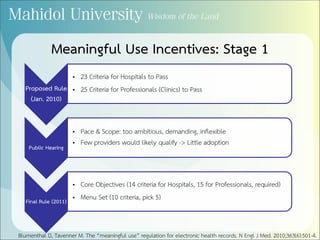
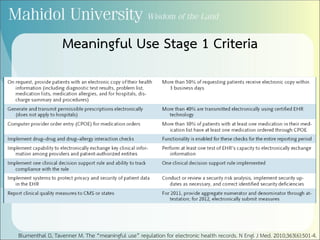
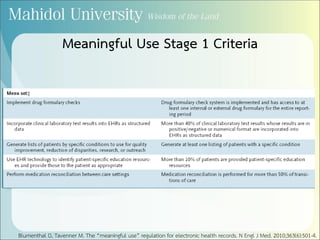
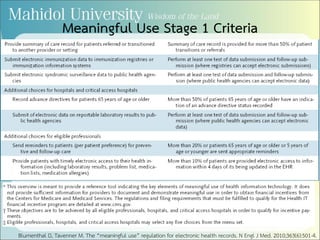
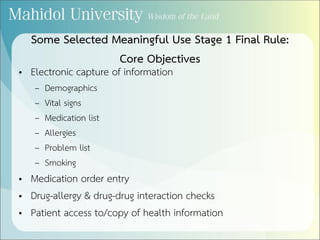
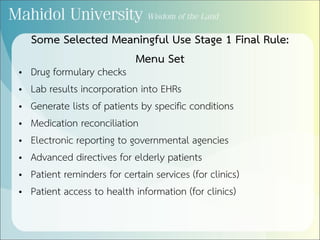
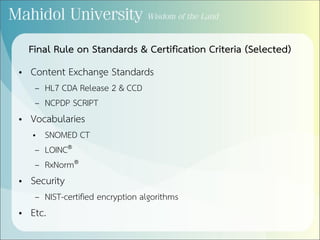
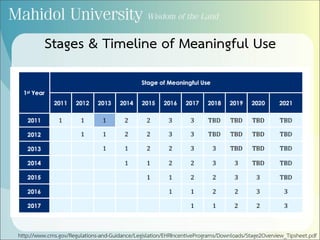
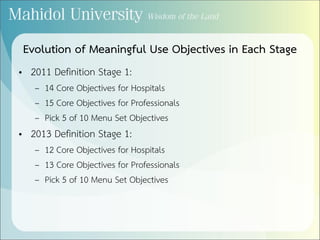
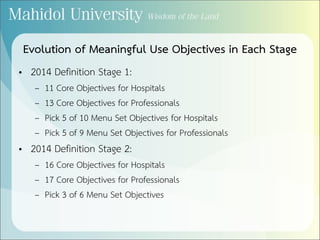
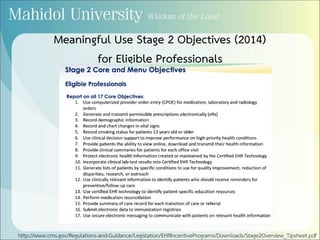
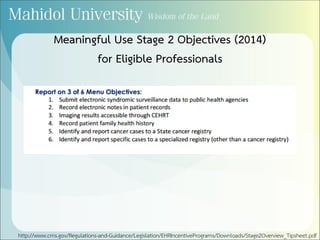
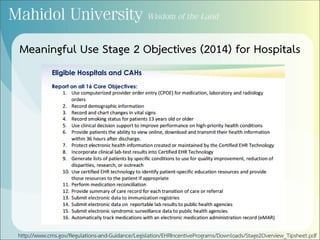
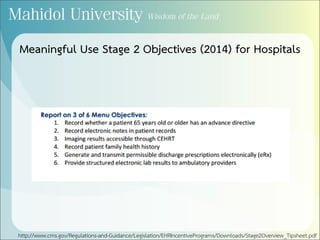
This document summarizes key events and policies related to the meaningful use of electronic health records (EHRs) in the United States. It discusses landmark reports that highlighted issues with patient safety and quality of care. Major legislation like HIPAA, ARRA, and the HITECH Act provided funding and incentives to promote EHR adoption. The Office of the National Coordinator for Health IT established criteria for meaningful use in three stages to gradually increase EHR functionality and use. Regulations specify objectives and standards that providers must meet to receive incentive payments through Medicare and Medicaid.

![References
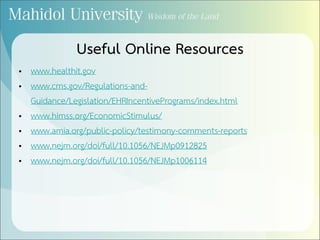
• Blumenthal D. Launching HITECH. N Engl J Med. 2010 Feb 4;362(5):382-5.
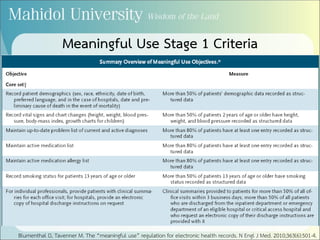
• Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J
Med. 2010 Aug 5;363(6):501-4.
• Hsiao C, Beatty PC, Hing ES, Woodwell DA. Electronic medical record/electronic health record use
by office-based physicians: United States, 2008 and preliminary 2009 [Internet]. 2009 [cited 2010
Apr 12]; Available from: http://www.cdc.gov/nchs/data/hestat/emr_ehr/emr_ehr.pdf
• Jha AK, DesRoches CM, Campbell EG, Donelan K, Rao SR, Ferris TG, Shields A, Rosenbaum S,
Blumenthal D. Use of electronic health records in U.S. hospitals. N Engl J Med. 2009;360(16):1628-
38.
• Jha AK, Doolan D, Grandt D, Scott T, Bates DW. The use of health information technology in seven
nations. Int J Med Inform. 2008;77(12):848-54.
• Schoen C, Osborn R, Huynh PT, Doty M, Puegh J, Zapert K. On the front lines of care: primary care
doctors’ office systems, experiences, and views in seven countries. Health Aff (Millwood).
2006;25(6):w555-71.](https://image.slidesharecdn.com/meaningfuluse-161019014330/85/Meaningful-Use-of-Electronic-Health-Records-October-16-2016-49-320.jpg)