This document provides an overview of urinalysis, including specimen collection, types of urine samples, physical and chemical examination, and microscopic examination. It discusses examining urine color, clarity, and specific gravity. Common tests including urine dipstick are outlined. Normal findings and discrepancies are highlighted. The microscopic examination section describes cells, casts, and crystals that may be observed, along with their clinical significance. In summary, the document is a comprehensive review of the various components of a urinalysis and their clinical relevance.









![• 10 to 15 mL (12ml) Centrifuged at 400 – 450 g (RCF), 1500 – 2000
(1600) (RPM) for 5 mins hold the test tube upside down and count to
3, then turn the test tube again and stand it upright mix drop (20
μL) in a slide + glass cover slip (carefully to avoid air bubbles) examine.
• Report RBCs/WBCs using high-power magnification (i.e., high-power field [hpf]),
report casts and crystals using low-power magnification (i.e., low-power field [lpf]).
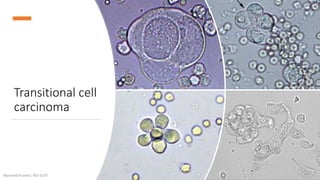
• Normal Urines: Contain 0-4 RBCs (hpf), 0-3 WBCs (hpf), 0-2 hyaline casts (lpf), several
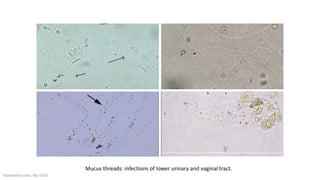
epithelial cells (hpf), some types of crystals, and mucus.
• Casts have a tendency to locate near the edges of the cover slip (LPF scanning around
the cover slip).
Microscopic examination
Alyazeed hussein, BSc-SUST](https://image.slidesharecdn.com/urinalysis-acomprehensivereview-200710143630/85/Urinalysis-a-comprehensive-review-11-320.jpg)