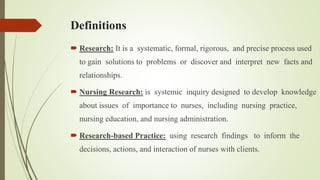
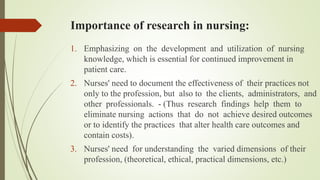
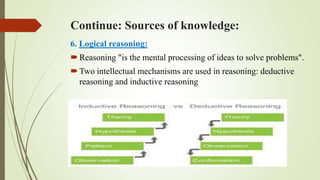
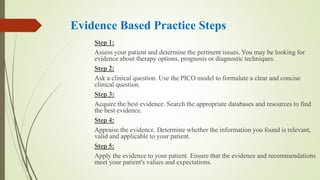
The document introduces nursing research, detailing its significance in improving nursing practice, education, and administration. It outlines the roles of nurses in research, emphasizing both indirect and direct participation, and discusses various sources of knowledge that inform nursing practices. Additionally, it explains the concept of evidence-based practice (EBP), its steps, and its critical role in enhancing patient care through informed decision-making.