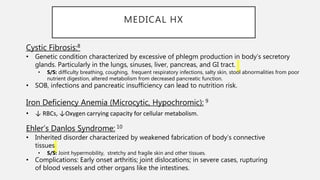
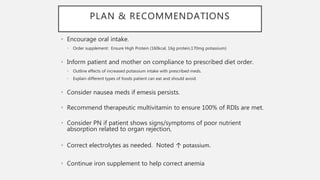
The document presents a clinical case study of a 30-year-old female patient, Madison Lupul, admitted for multivisceral transplantation at the University of Alabama at Birmingham. It details her medical history, clinical course, nutritional assessment, medication implications, and post-transplant dietary recommendations, emphasizing the importance of monitoring and managing her nutritional status and medication interactions. The care plan includes dietary education and strategies to address nutrient deficiencies and prevent complications post-surgery.