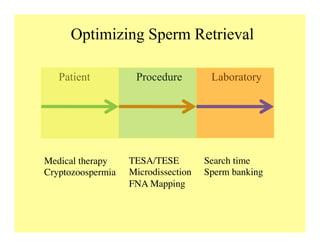
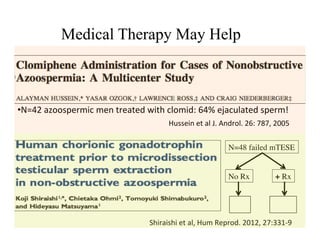
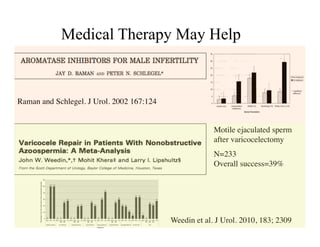
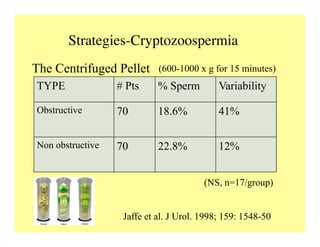
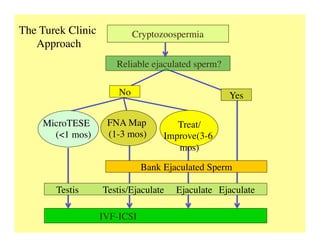
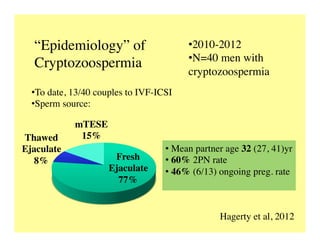
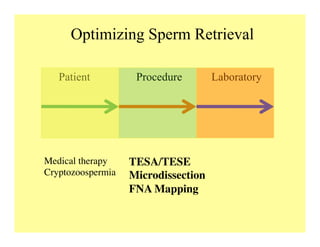
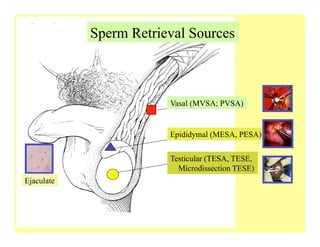
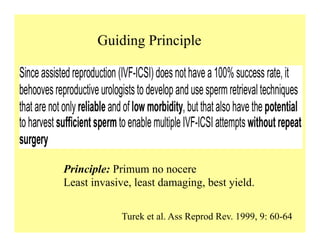
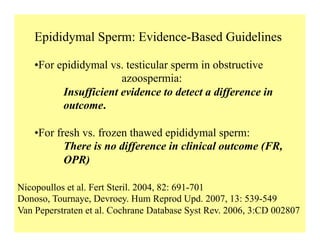
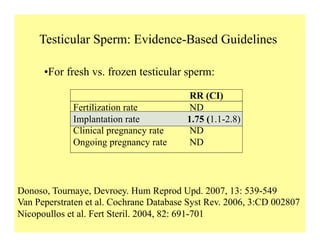
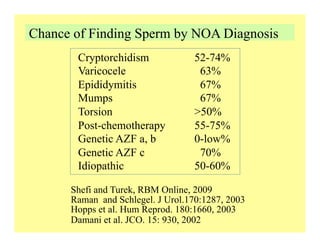
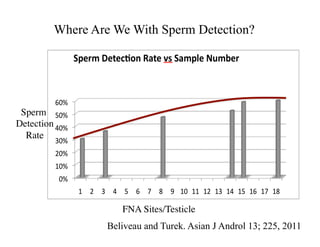
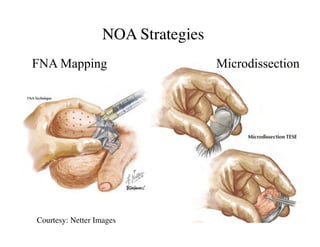
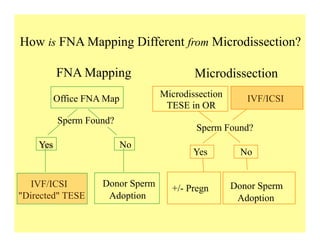
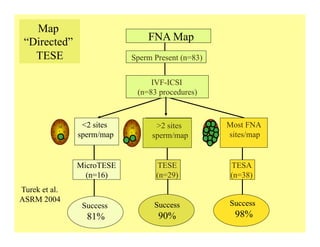
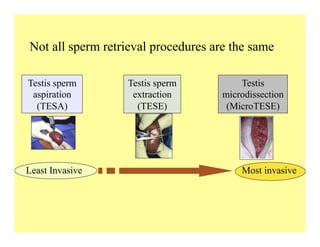
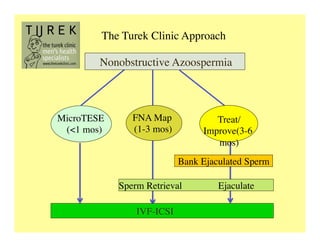
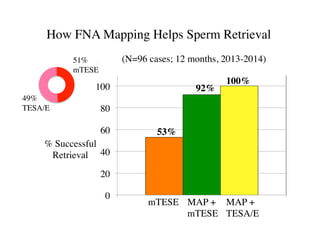
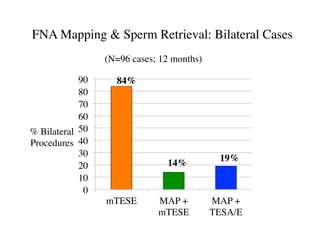
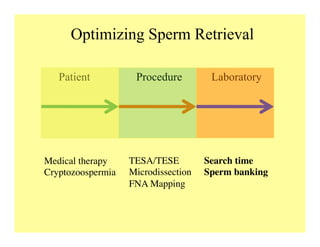
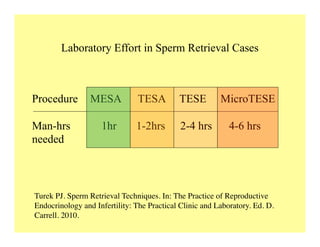
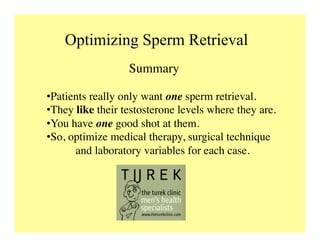
The document discusses optimizing sperm retrieval techniques for men with nonobstructive azoospermia, focusing on medical therapy, sperm search strategies, and laboratory methods. It highlights various research findings on sperm retrieval success rates, the effectiveness of different techniques like microdissection and FNA mapping, and the importance of adapting approaches to individual patient needs. The overarching goal is to maximize the chances of successful sperm retrieval for IVF purposes while minimizing invasiveness and preserving testosterone levels.