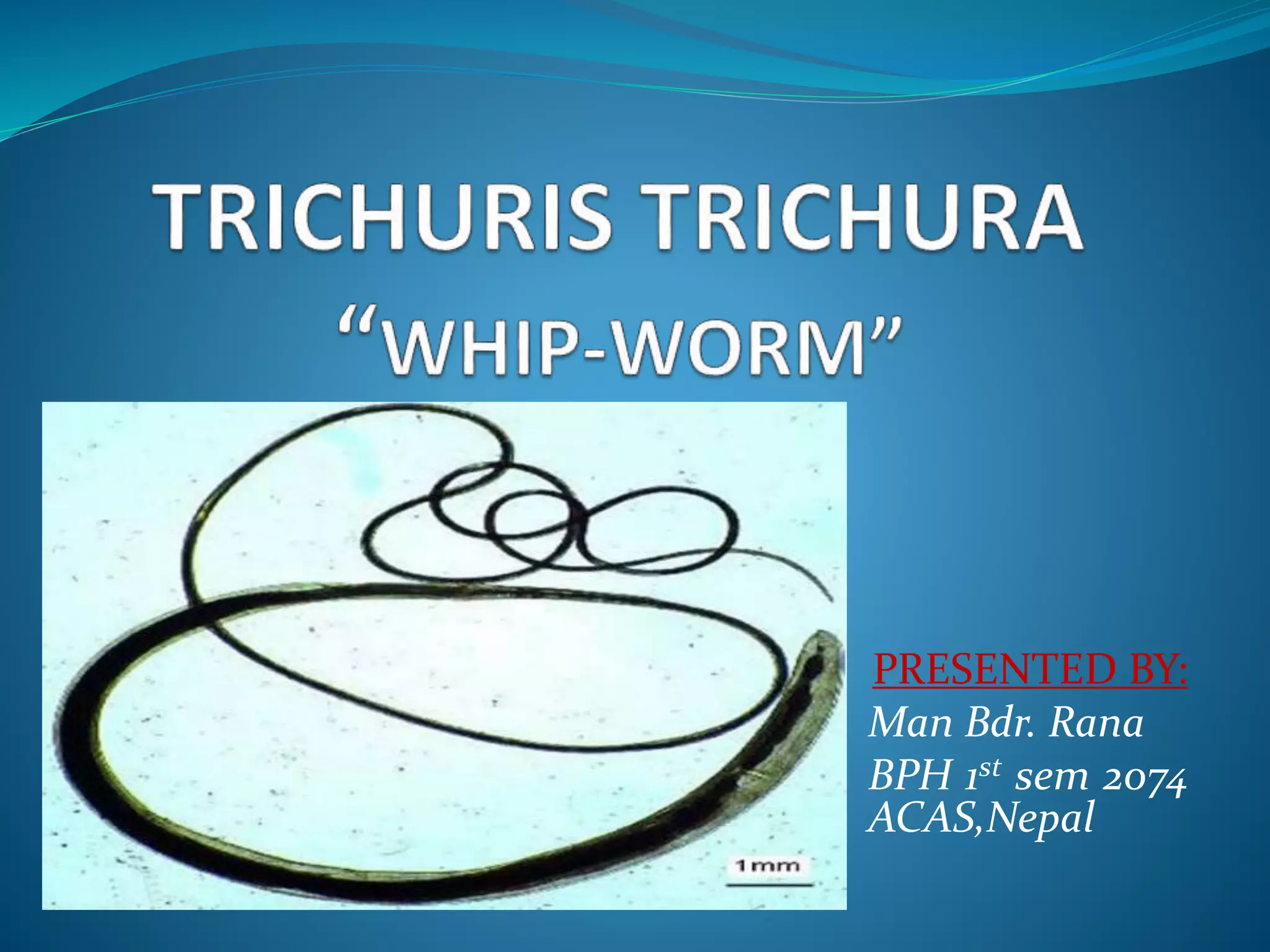
This document summarizes information about the whipworm (Trichuris trichura) including its morphology, life cycle, pathogenesis, clinical features, diagnosis, treatment and prevention. It notes that the adult worm is 50mm long with a thicker posterior end. Eggs measure 50-54 by 22-23 micrometers and contain unembryonated eggs that are passed in stool. The life cycle involves ingestion of eggs which hatch and develop into adults in the intestines. Clinical features range from asymptomatic to digestive disturbances depending on worm burden. Diagnosis involves examining stool for eggs using iodine or histopathology of intestinal mucosa. Treatment involves albendazole or mebendazole.