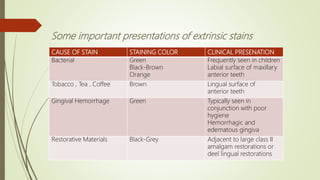
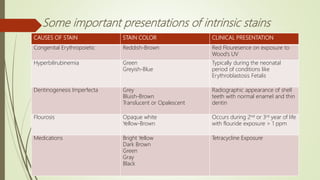
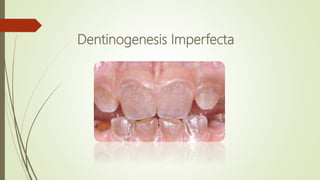
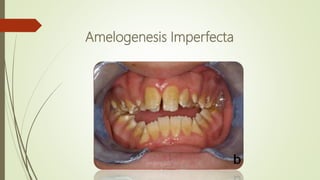
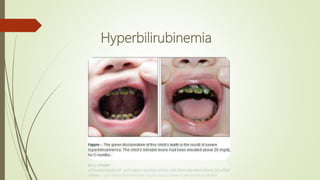
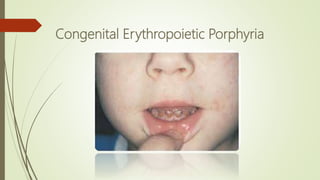
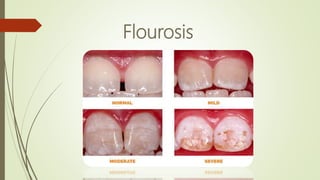
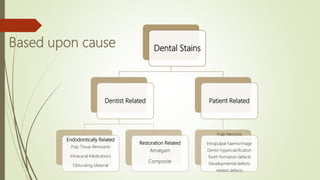
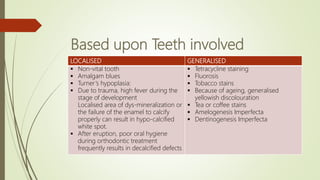
This document provides information on tooth staining and discoloration. It begins by defining tooth discoloration and classifying it based on origin (intrinsic vs extrinsic), cause, and teeth involved (localized vs generalized). Extrinsic staining is on the outer tooth surface and can result from factors like poor oral hygiene or chromogenic bacteria. Intrinsic staining is internal and can be caused by things like tetracycline use, fluorosis, or hereditary disorders. Treatment options discussed include scaling, microabrasion, bleaching, veneers, and crowns. Bleaching involves the use of peroxide compounds like hydrogen peroxide or carbamide peroxide to lighten teeth through oxidation of organic pigments.