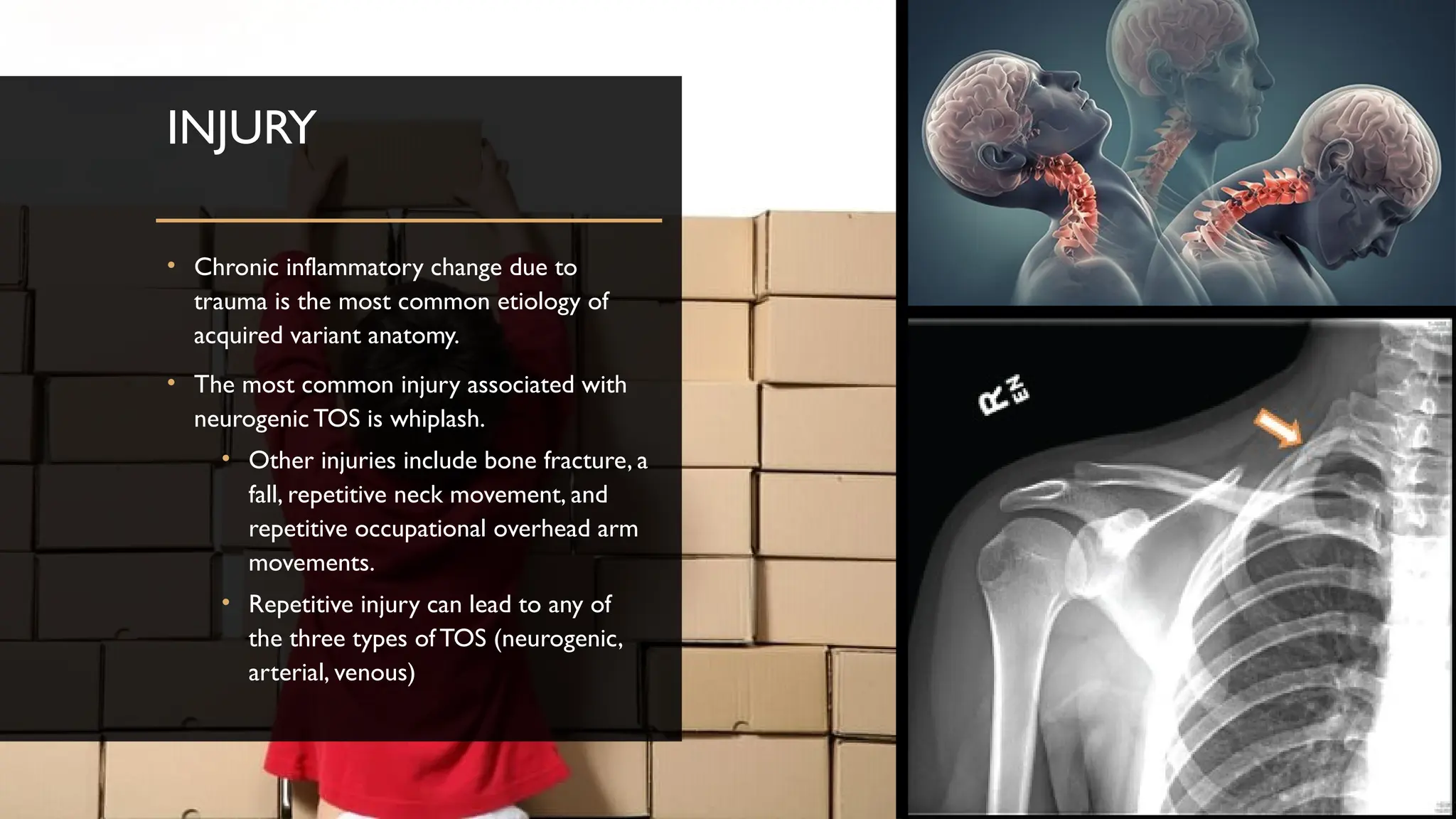
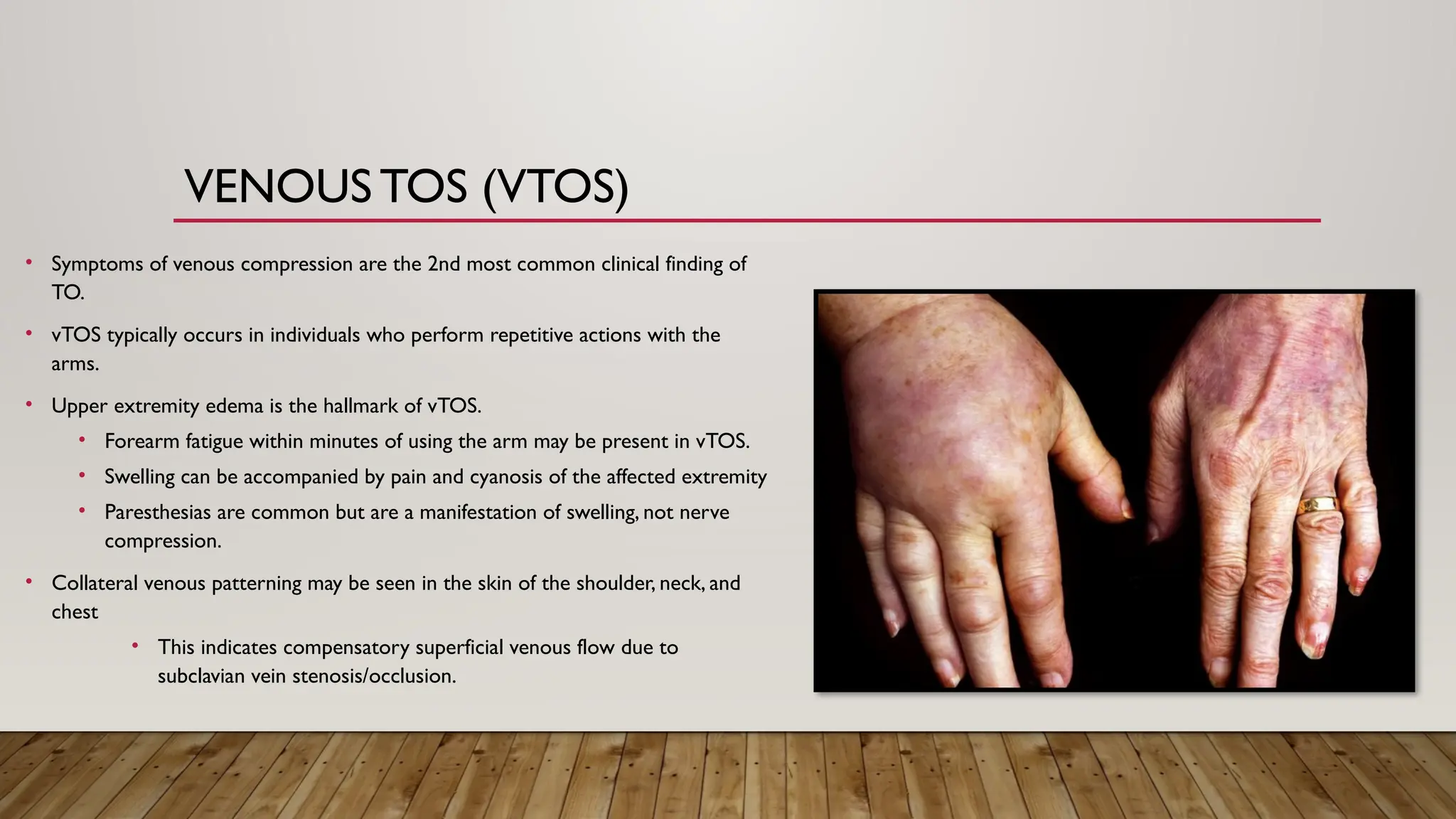
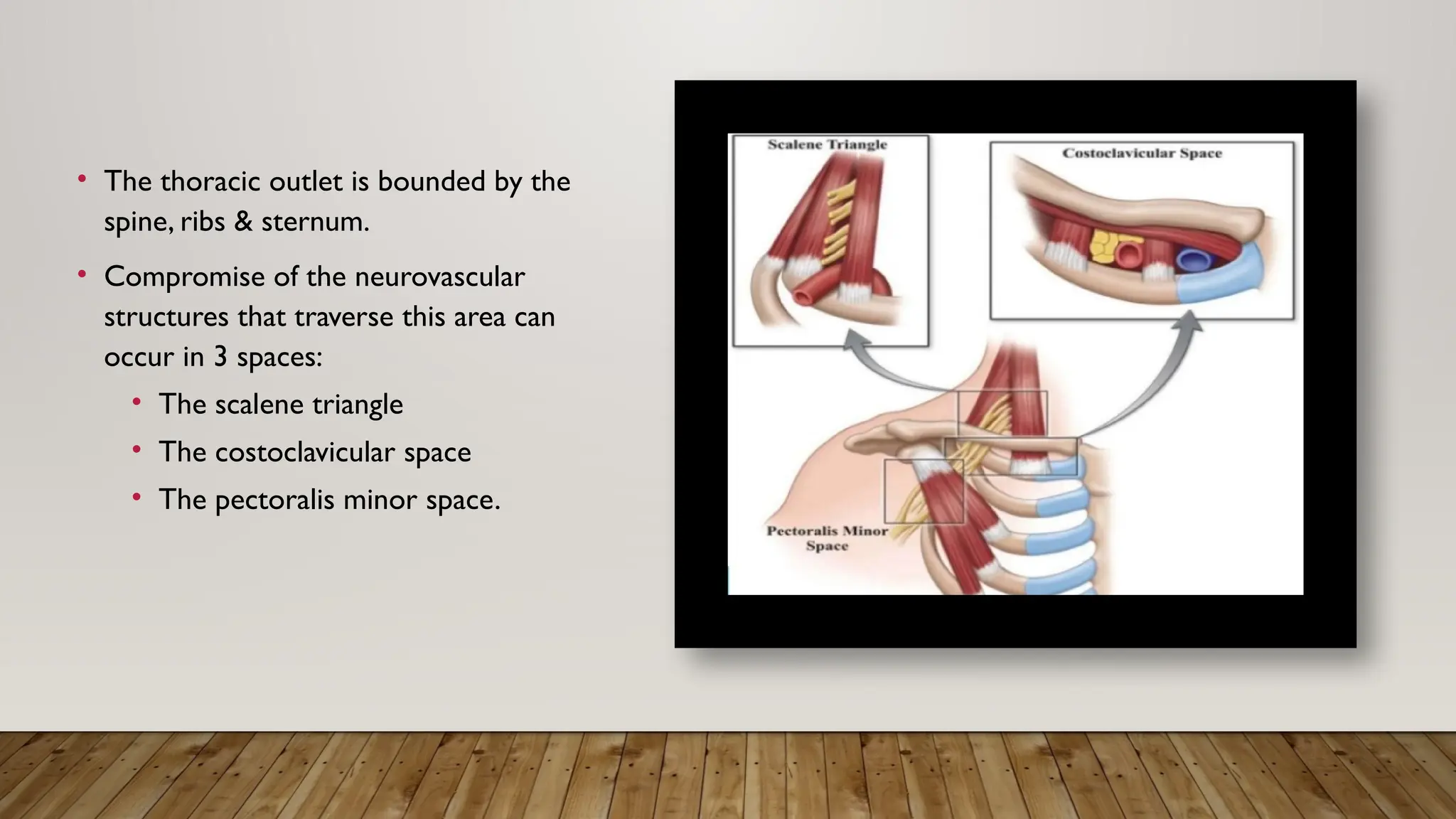
Thoracic outlet syndrome (TOS) involves compression of neurovascular structures in three main spaces: the scalene triangle, costoclavicular space, and pectoralis minor space, with common symptoms varying by type (neurogenic, venous, arterial). Compression can arise from anatomical abnormalities, injuries, or physical activities, and diagnostic approaches include imaging and electrodiagnostic tests. Treatment often involves conservative measures like physical therapy, while surgical options may be necessary for symptomatic cases, particularly with vascular TOS.







![CONGENITAL CERVICAL FIBRO-CARTILAGINOUS BANDS associated with an incomplete
cervical rib have also been associated with TOS.
• The problem in true neurogenic TOS is NOT the cervical rib, but a radiolucent band that extends from
the tip of the cervical rib to the 1st thoracic rib, compressing the proximal lower trunk of the brachial
plexus [22].](https://image.slidesharecdn.com/thoracicoutletsyndrome-240814010029-d7686f47/75/Thoracic-Outlet-Syndrome-Review-and-Guidelines-10-2048.jpg)