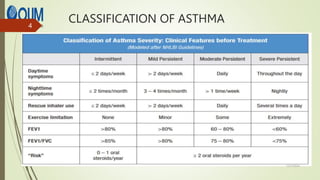
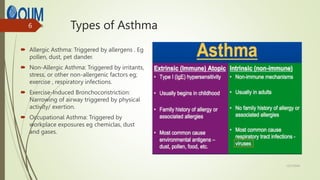
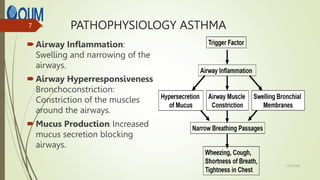
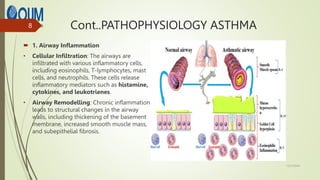
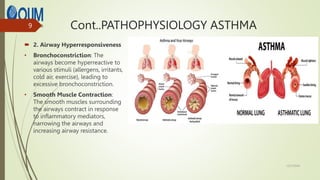
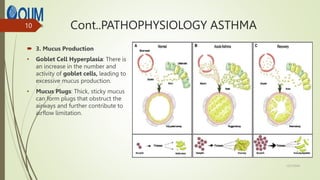
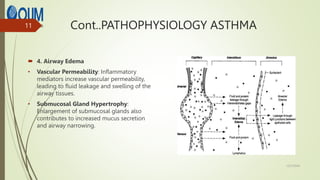
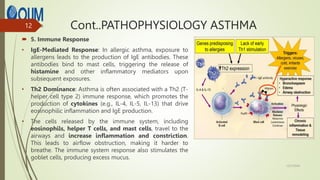
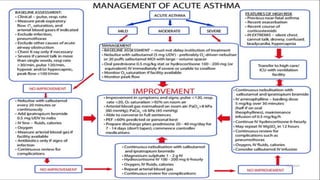
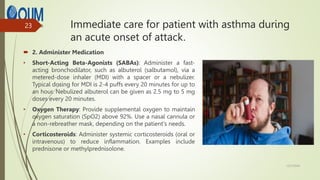
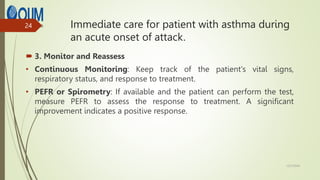
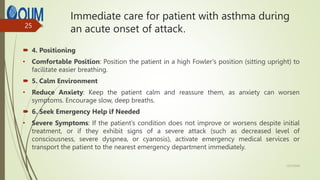
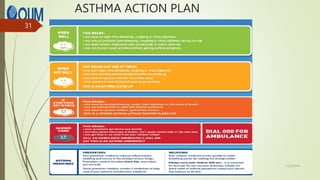
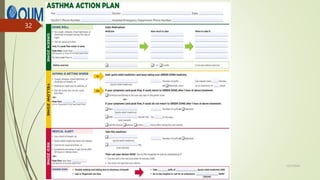
This document provides a comprehensive overview of asthma, detailing its pathophysiology, types, symptoms, and respiratory assessments necessary for effective management. It emphasizes the importance of an individualized asthma action plan and immediate care strategies during acute attacks to improve patient outcomes. The role of health beliefs in managing asthma and enhancing adherence to treatments is also discussed.