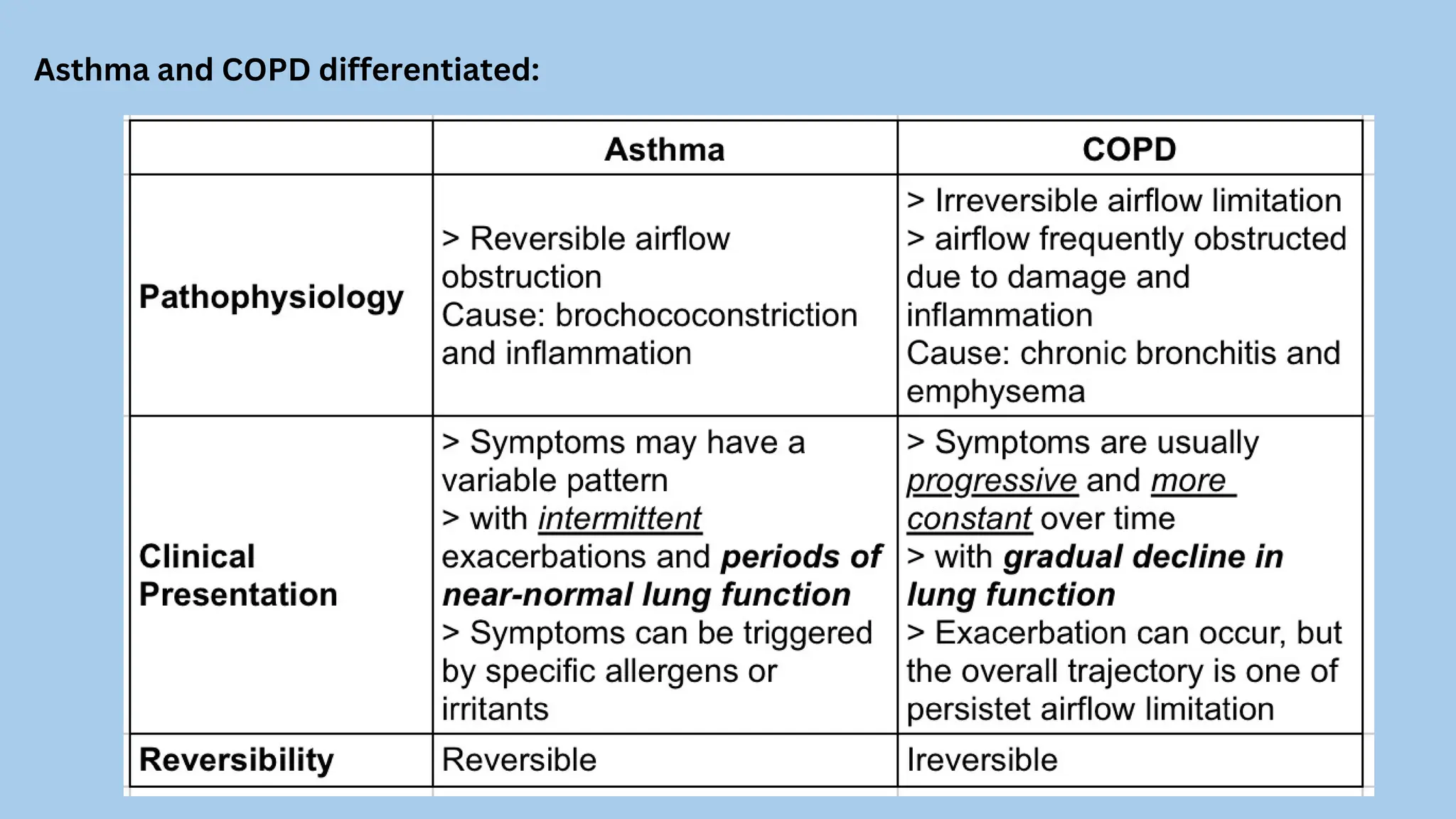
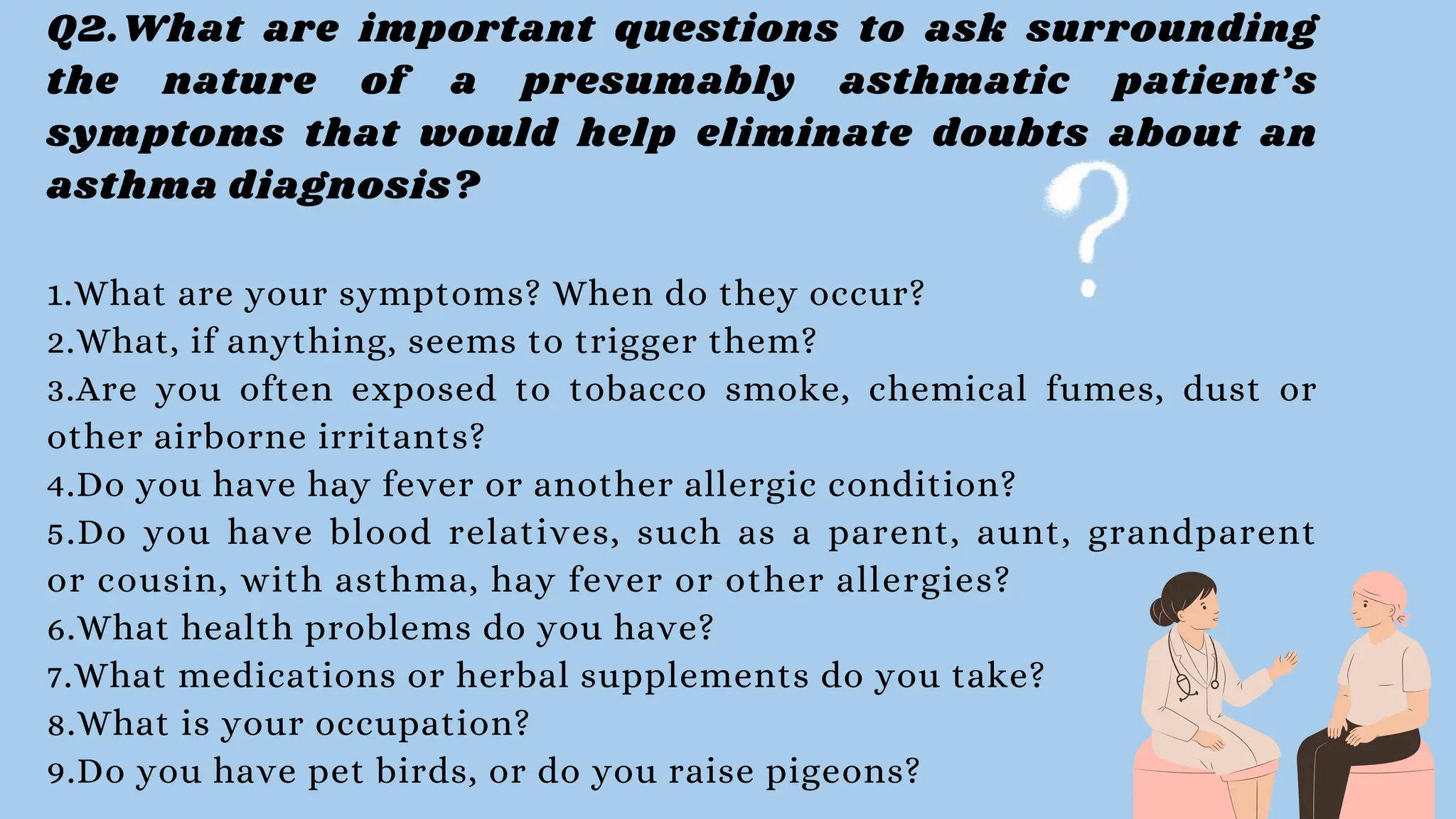
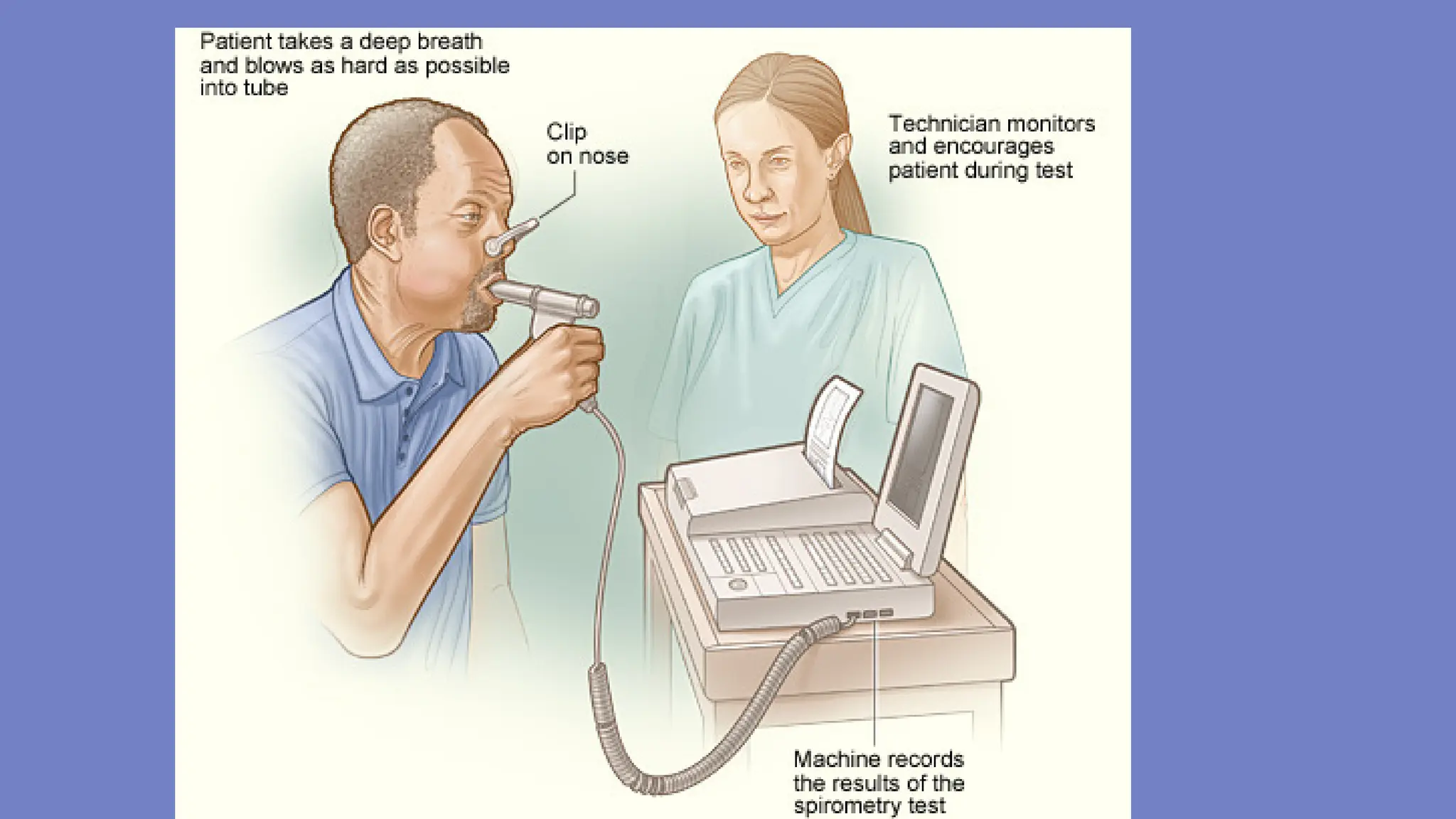
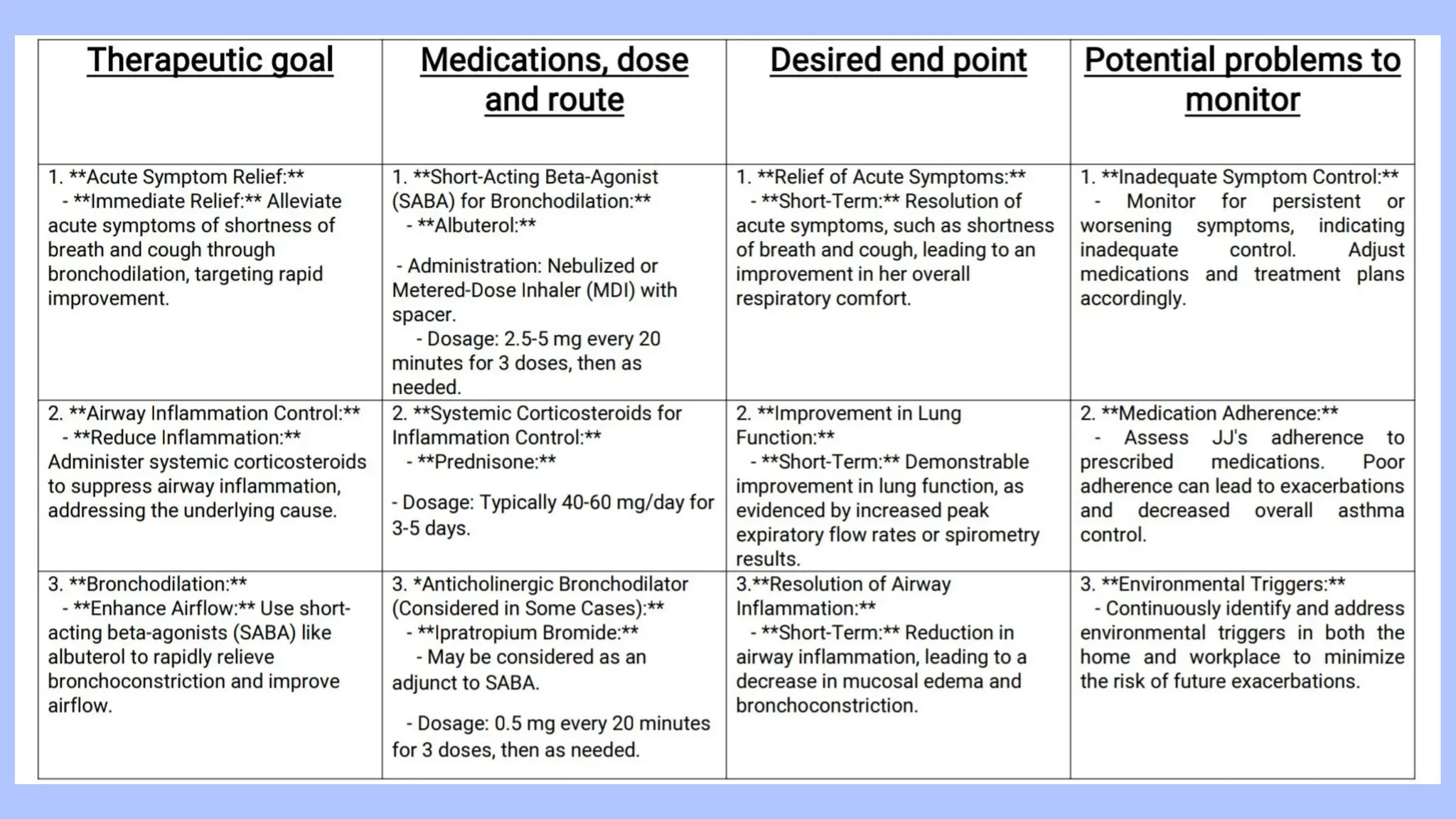
The document discusses a case of a 23-year-old female presenting with shortness of breath and cough after exposure to a cat, detailing her medical history and vital signs. It explains asthma's pathophysiology, diagnosis, and differentiation from COPD, emphasizing the importance of spirometry for diagnosis and inhaled corticosteroids as first-line treatment. The therapeutic plan includes trigger avoidance, asthma education, and regular follow-ups to enhance asthma management and reduce exacerbations.