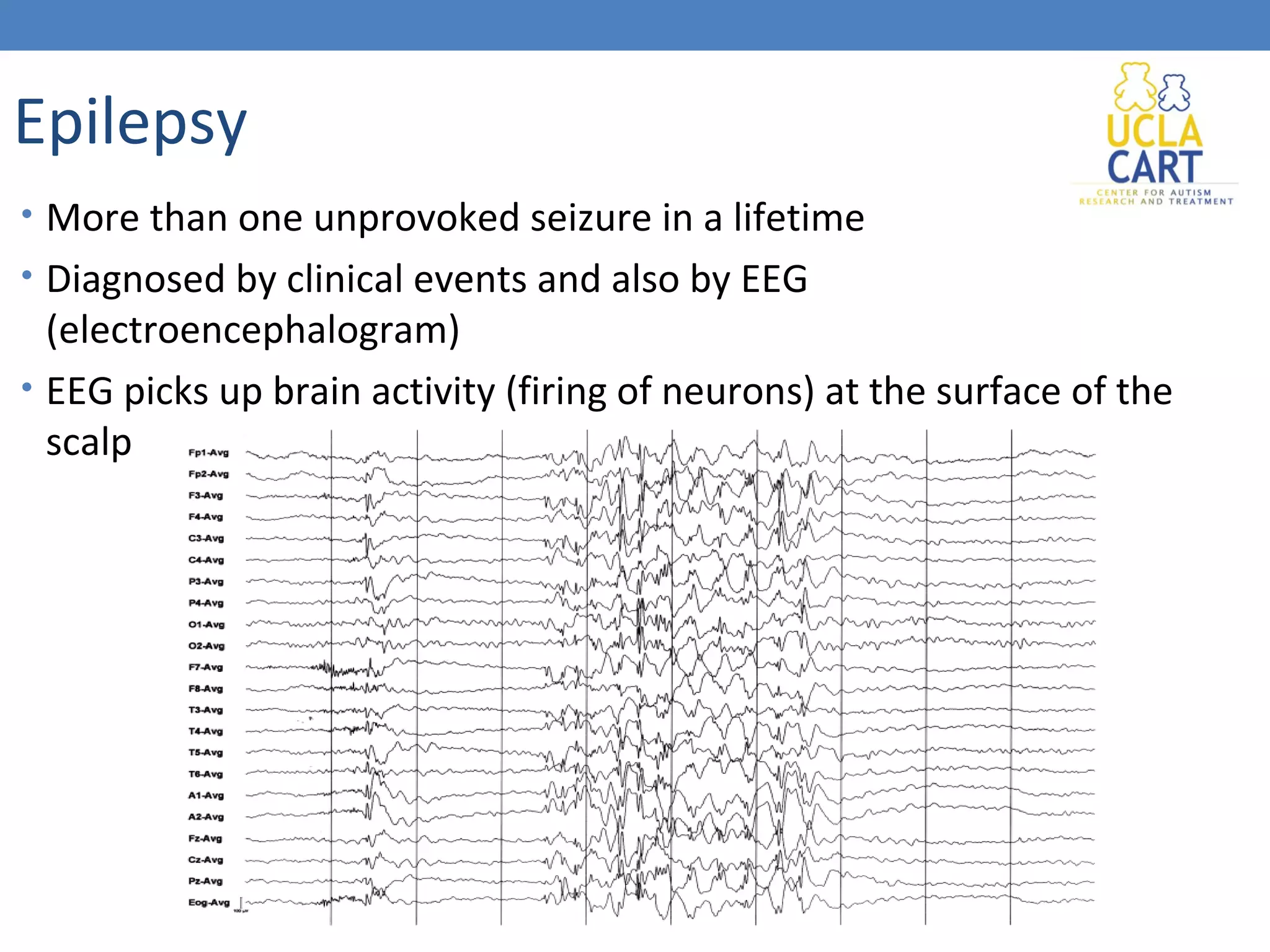
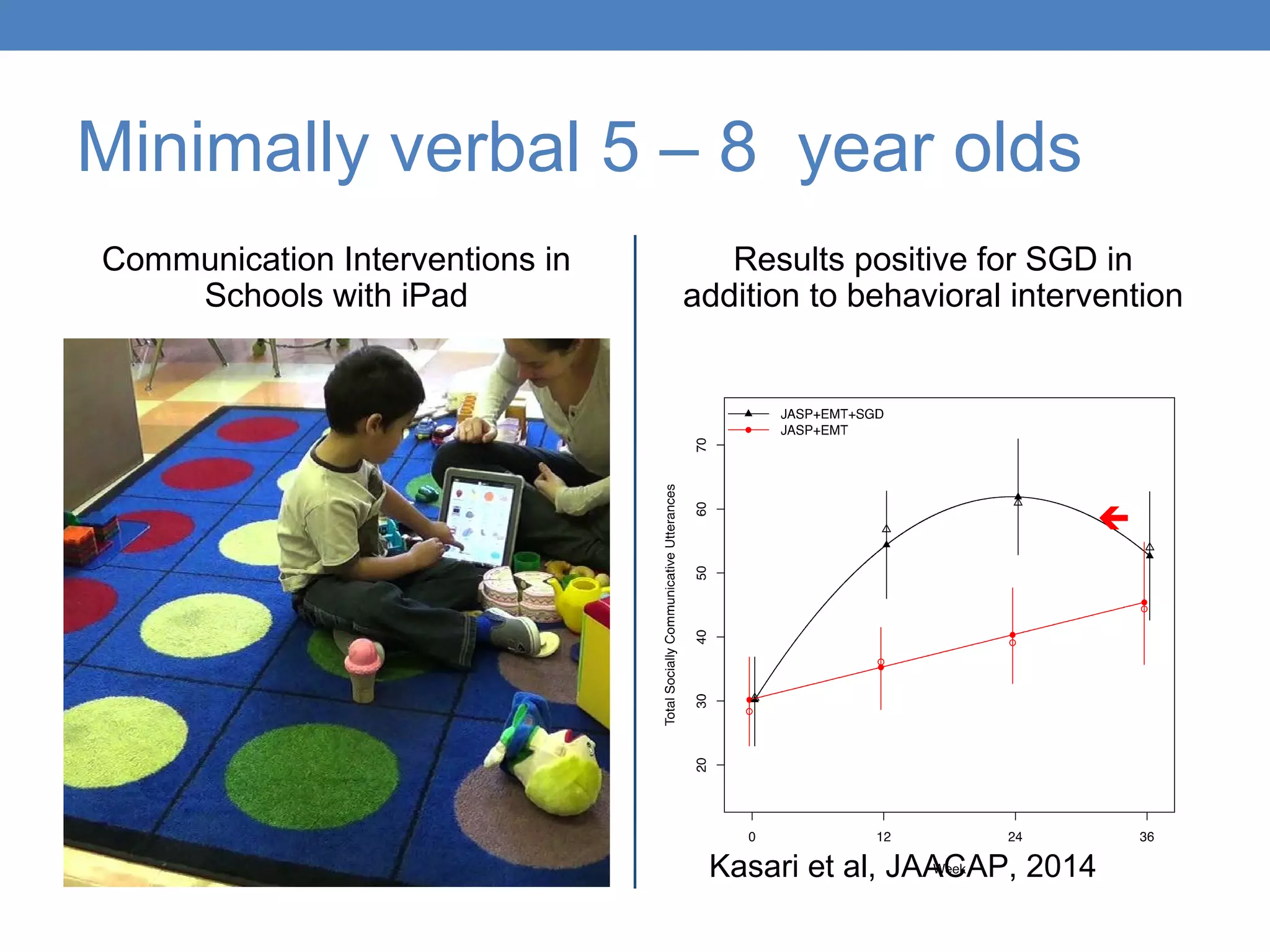
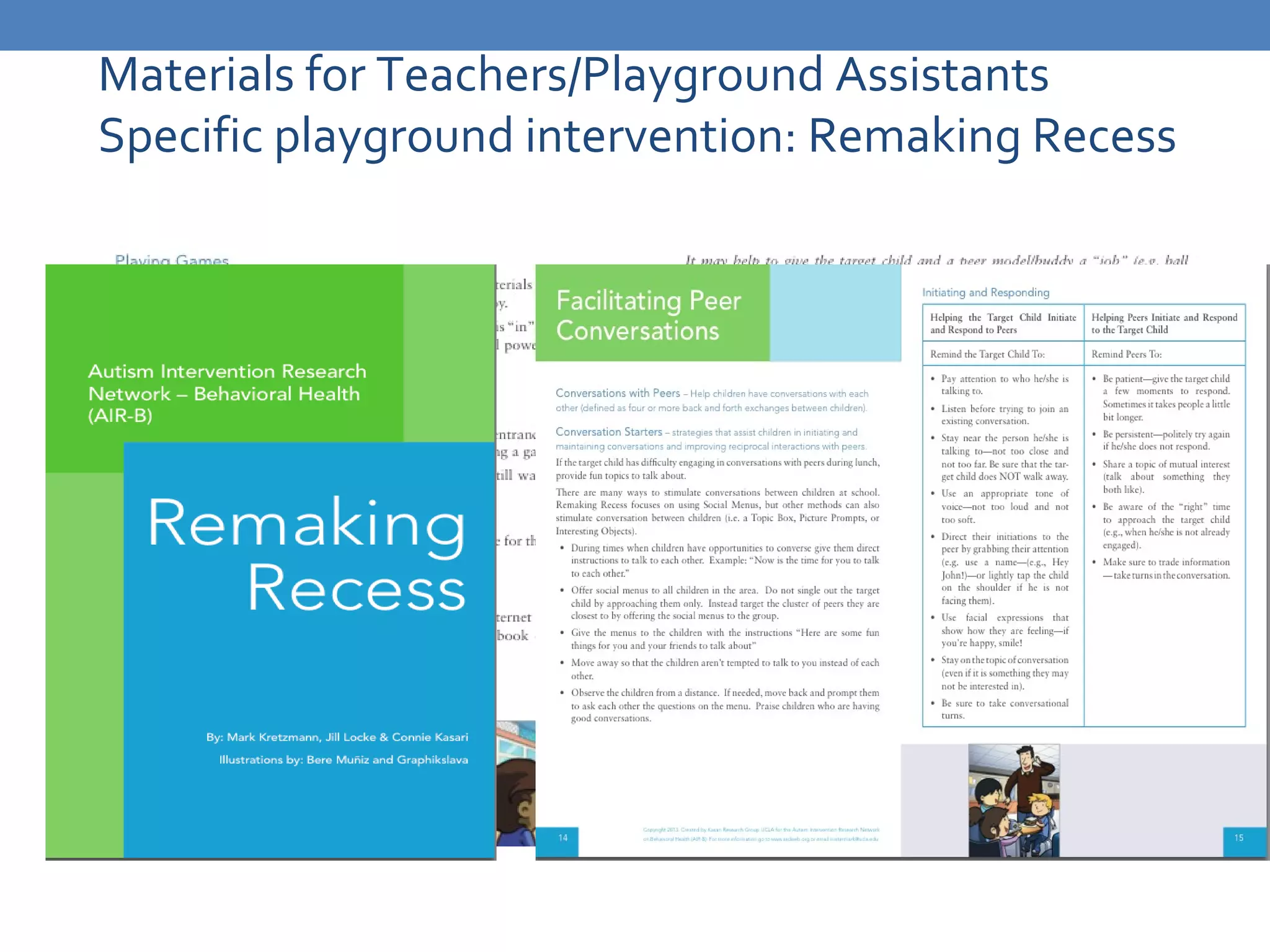
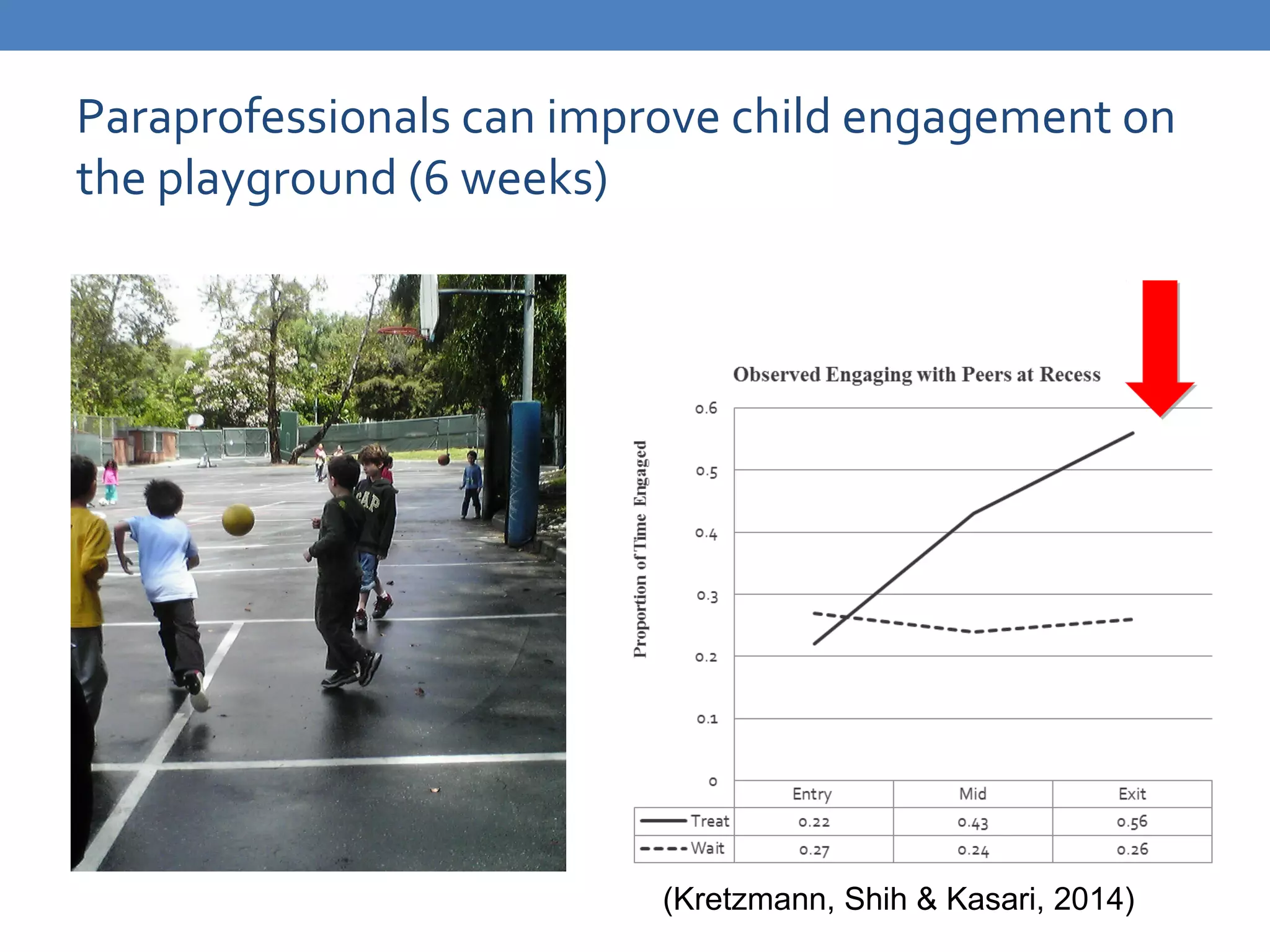
The document discusses autism spectrum disorders and the multidisciplinary team approach utilized by the UCLA Center for Autism Research and Treatment, focusing on understanding origins, diagnostics, and effective treatments. It highlights the importance of early identification and intervention, detailing diagnostic criteria, screening methods, medical evaluations, and psychiatric co-morbidities associated with autism. Additionally, it outlines various interventions tailored for children, adolescents, and adults with ASD to improve social skills, communication, and overall quality of life.