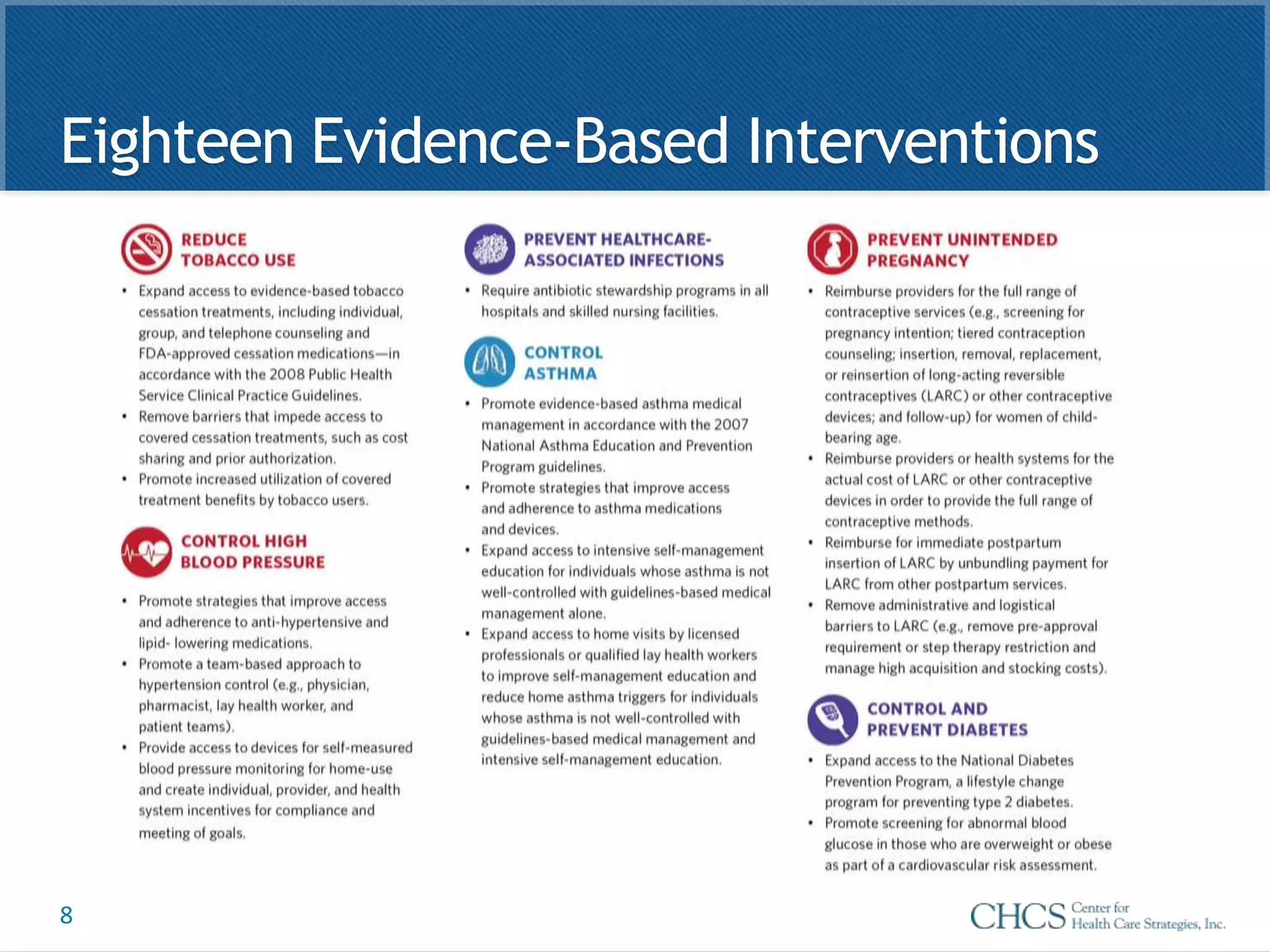
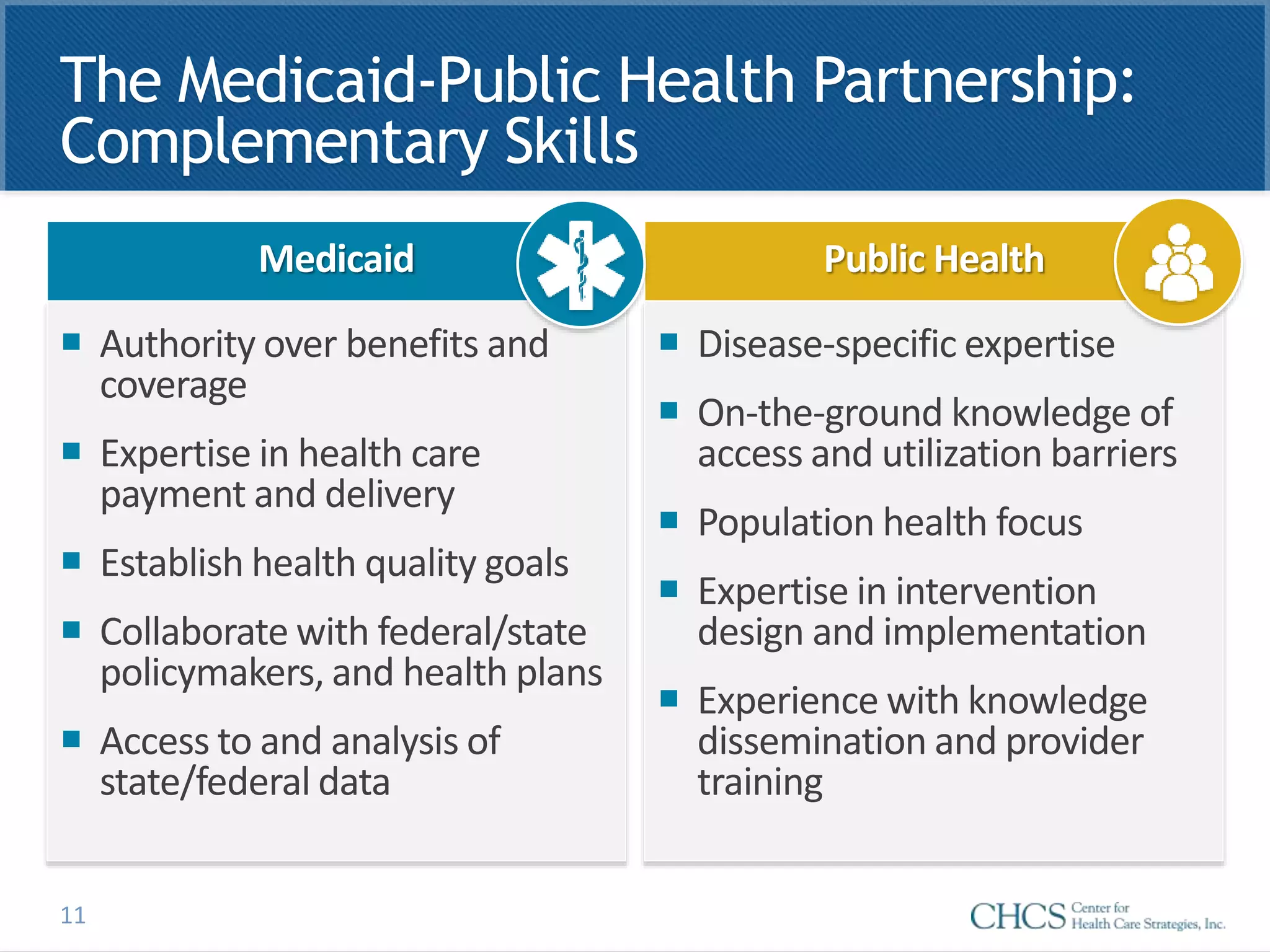
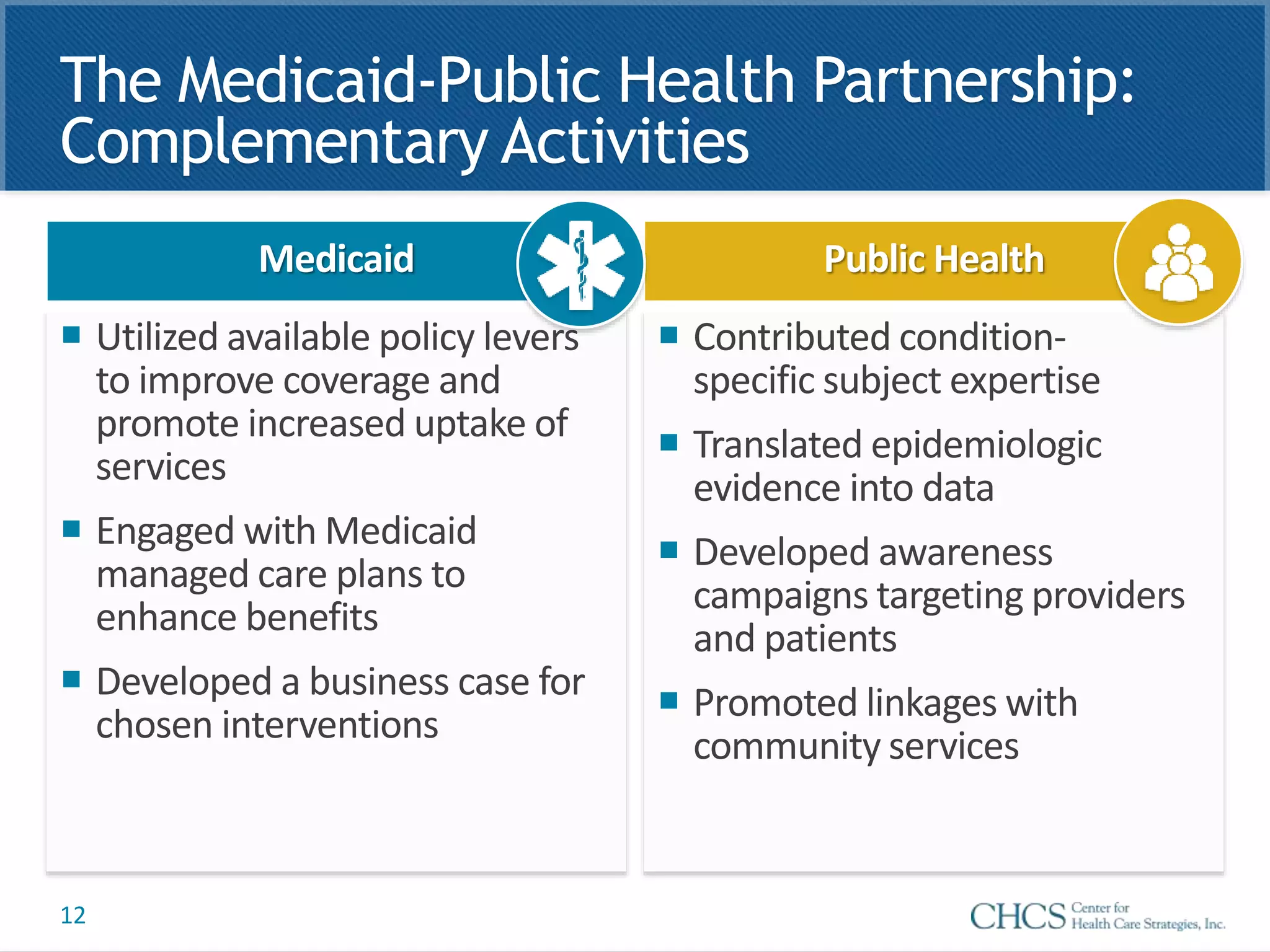
This document discusses a collaboration between Medicaid agencies and public health departments called the 6|18 Initiative. The initiative aims to improve health outcomes and lower costs for six high-burden health conditions using eighteen evidence-based interventions. Through the initiative, Medicaid agencies utilized policy levers to improve coverage and promote service uptake, while public health departments contributed disease-specific expertise, helped translate evidence into data, and developed awareness campaigns. Key factors in the successful collaboration included early leadership buy-in, a joint work plan, and monthly coordination calls between the partners.