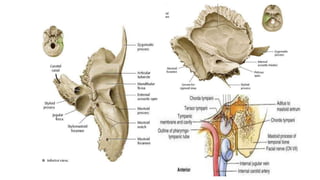
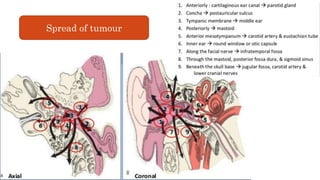
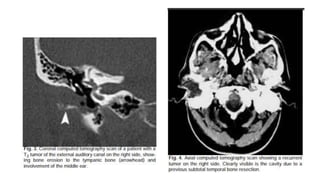
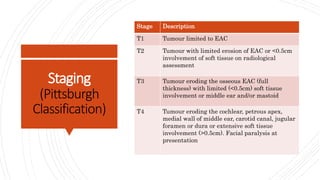
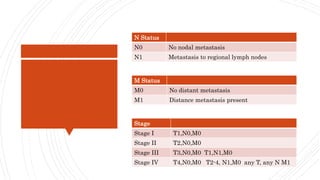
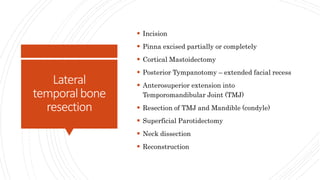
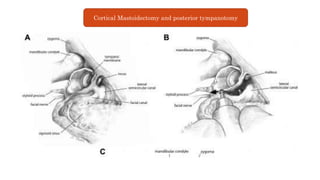
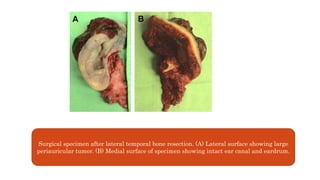
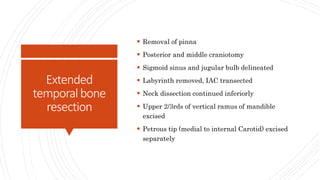
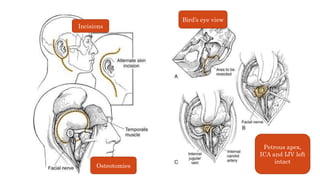
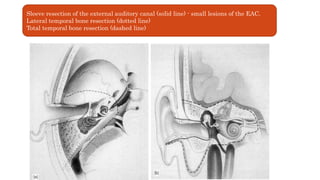
The document discusses carcinoma of the temporal bone, highlighting its rarity, rapid progression, and limited treatment success, particularly in females. It details relevant anatomy, etiology including chronic otitis media and HPV, clinical presentations, diagnostic methods, staging classifications, treatment options like resection and adjuvant therapy, as well as complications and outcomes with survival rates. The prognosis diminishes significantly with advanced stages, emphasizing the importance of early detection and intervention.