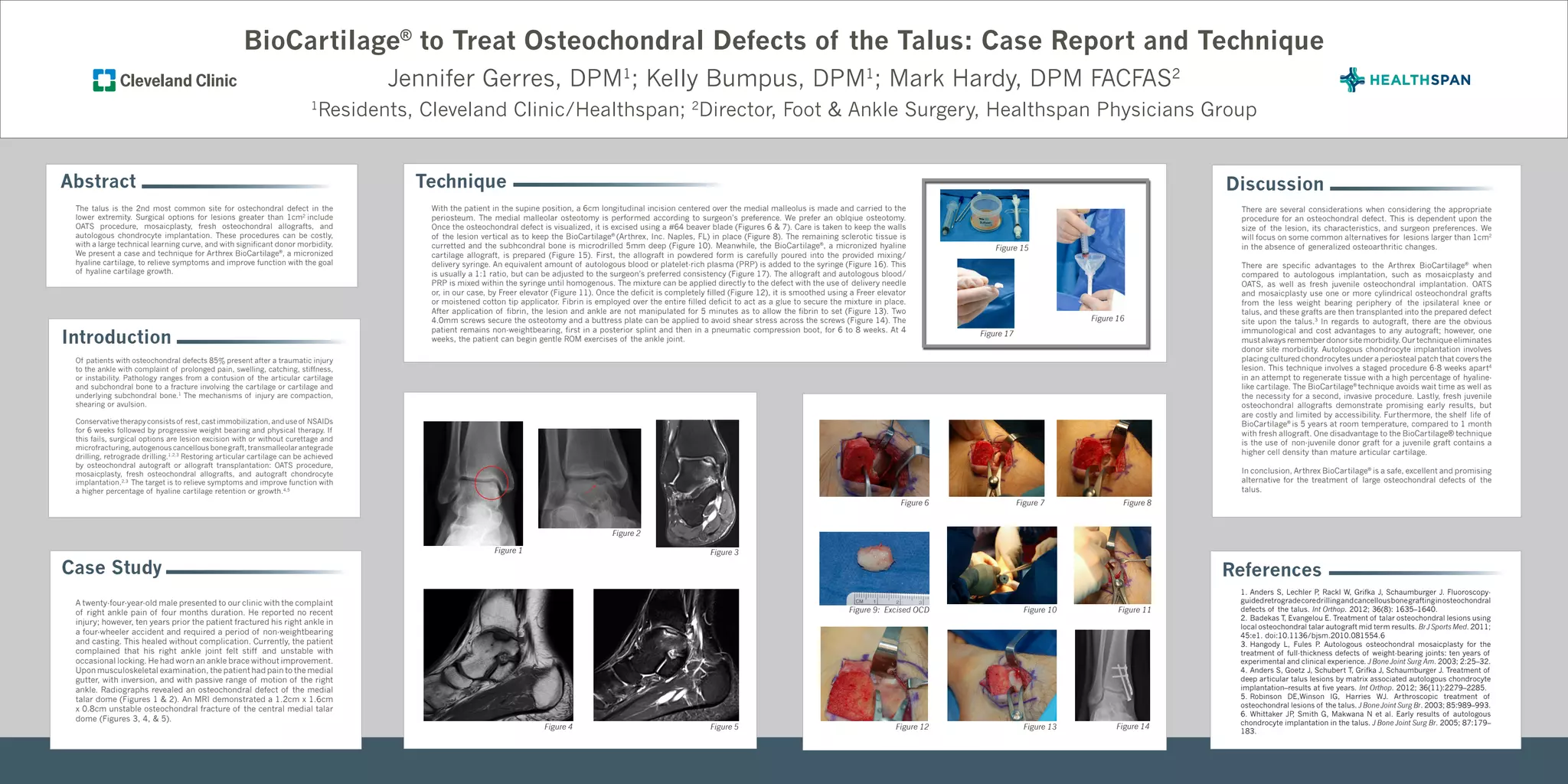
The document describes a case study and technique using BioCartilage to treat a large osteochondral defect of the talus. The key points are:
1) A 24-year old male presented with ankle pain and imaging revealed a 1.2cm x 1.6cm osteochondral defect of the talus.
2) The defect was excised and microdrilled. BioCartilage, a micronized hyaline cartilage allograft, mixed with blood or PRP was used to fill the defect.
3) BioCartilage offers advantages over other techniques like autografts in eliminating donor site morbidity and over ACI in being a single-stage procedure without wait time.