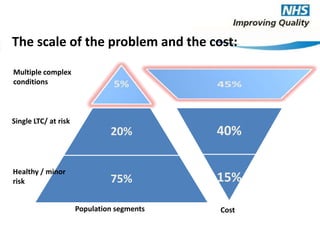
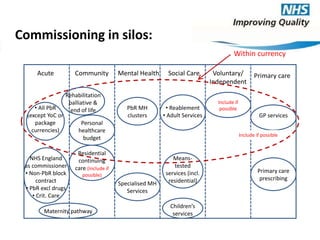
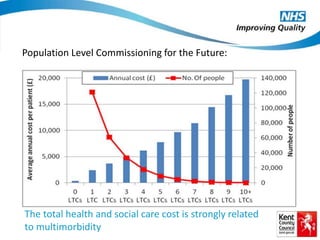
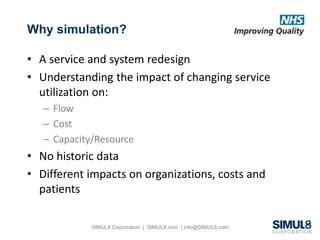
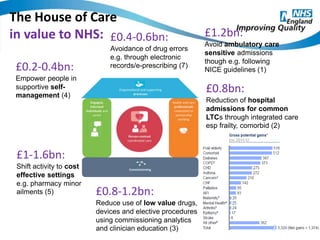
The document outlines the development of integrated care networks for managing long-term conditions in England, highlighting the importance of person-centered care and risk stratification. It emphasizes the significant healthcare costs associated with multimorbidity and advocates for population-level commissioning to improve service delivery. The 'House of Care' framework is introduced as a model for providing coordinated care, aiming to enhance patient outcomes and reduce overall healthcare expenditures.