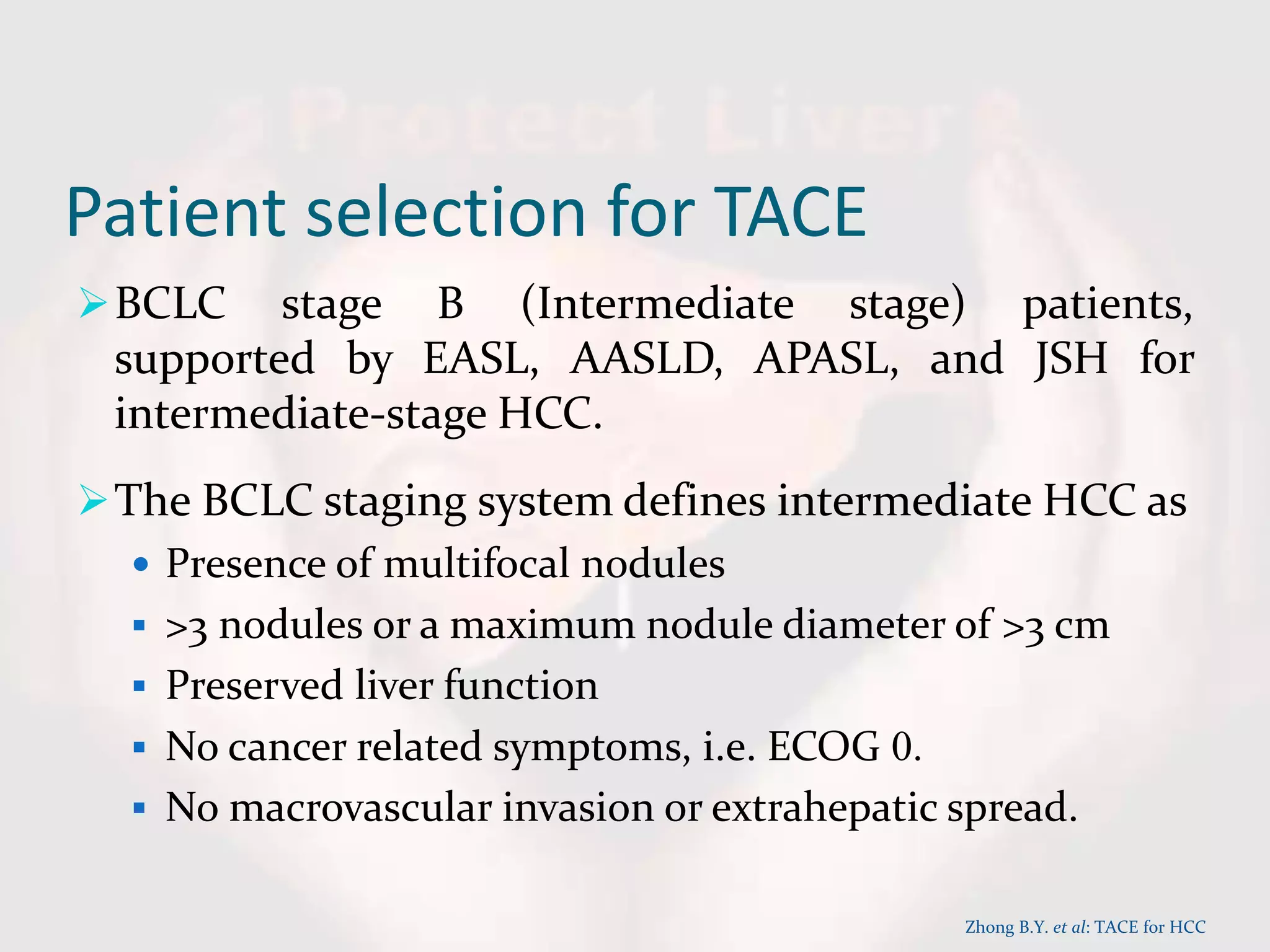
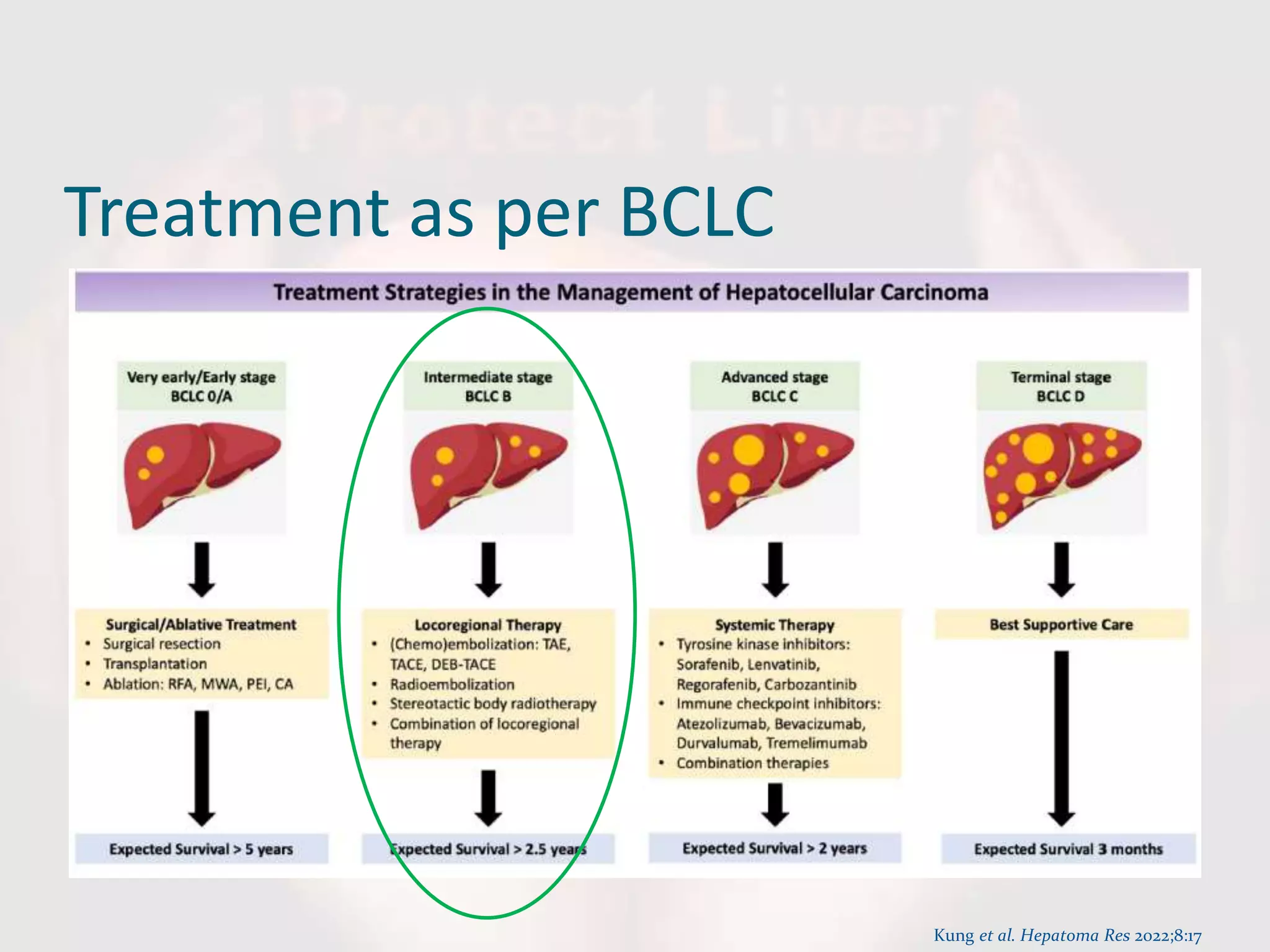
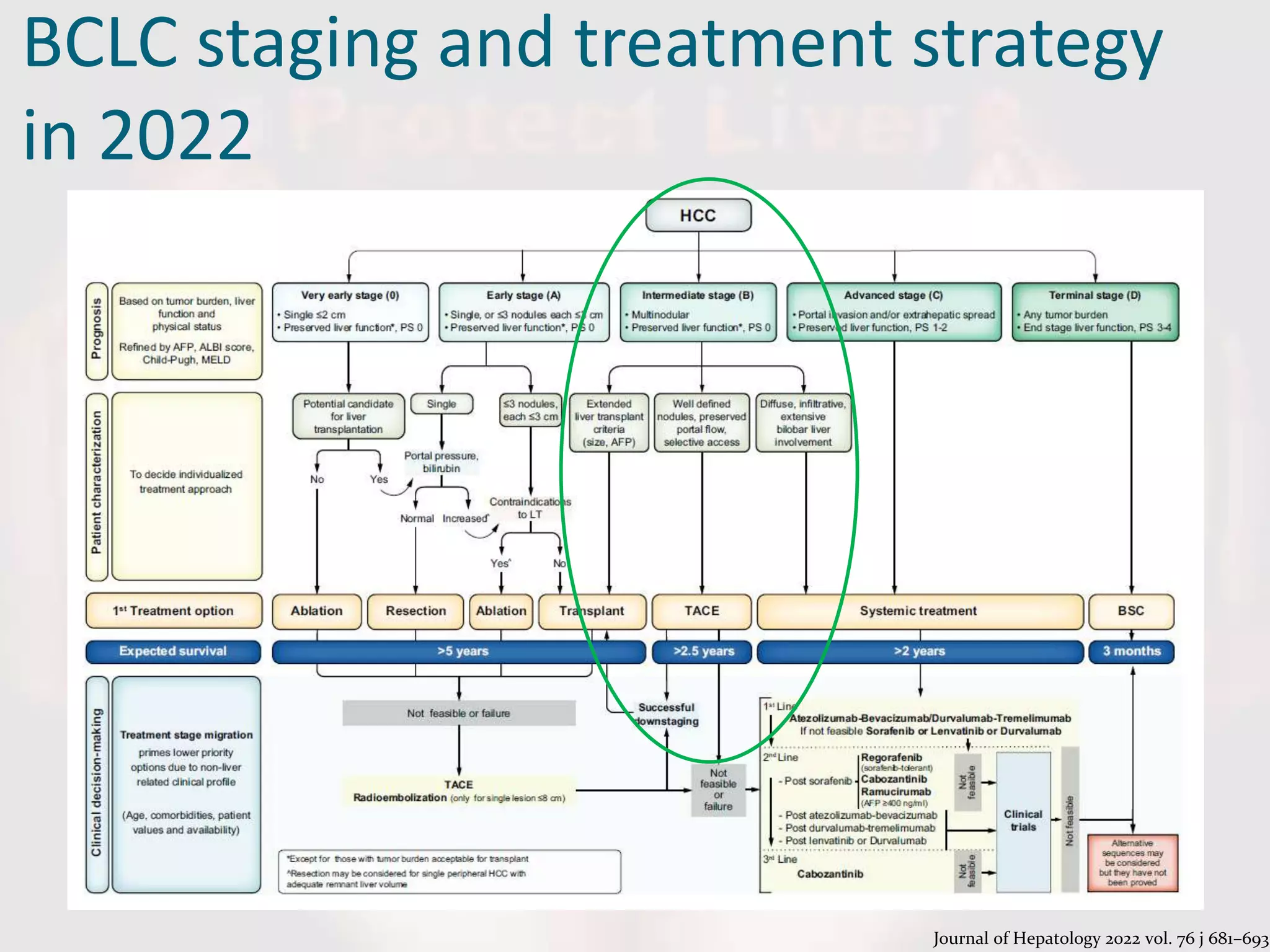
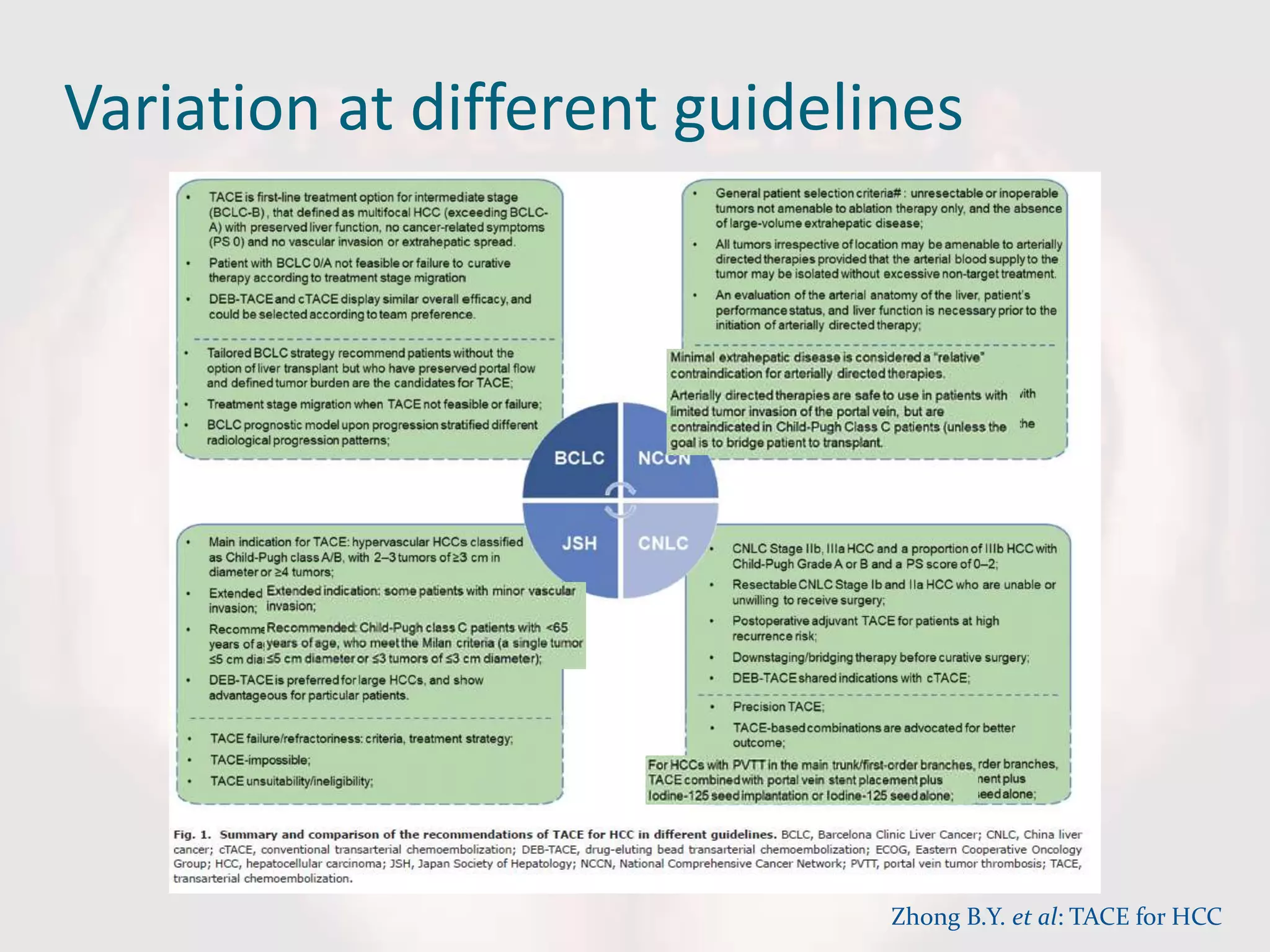
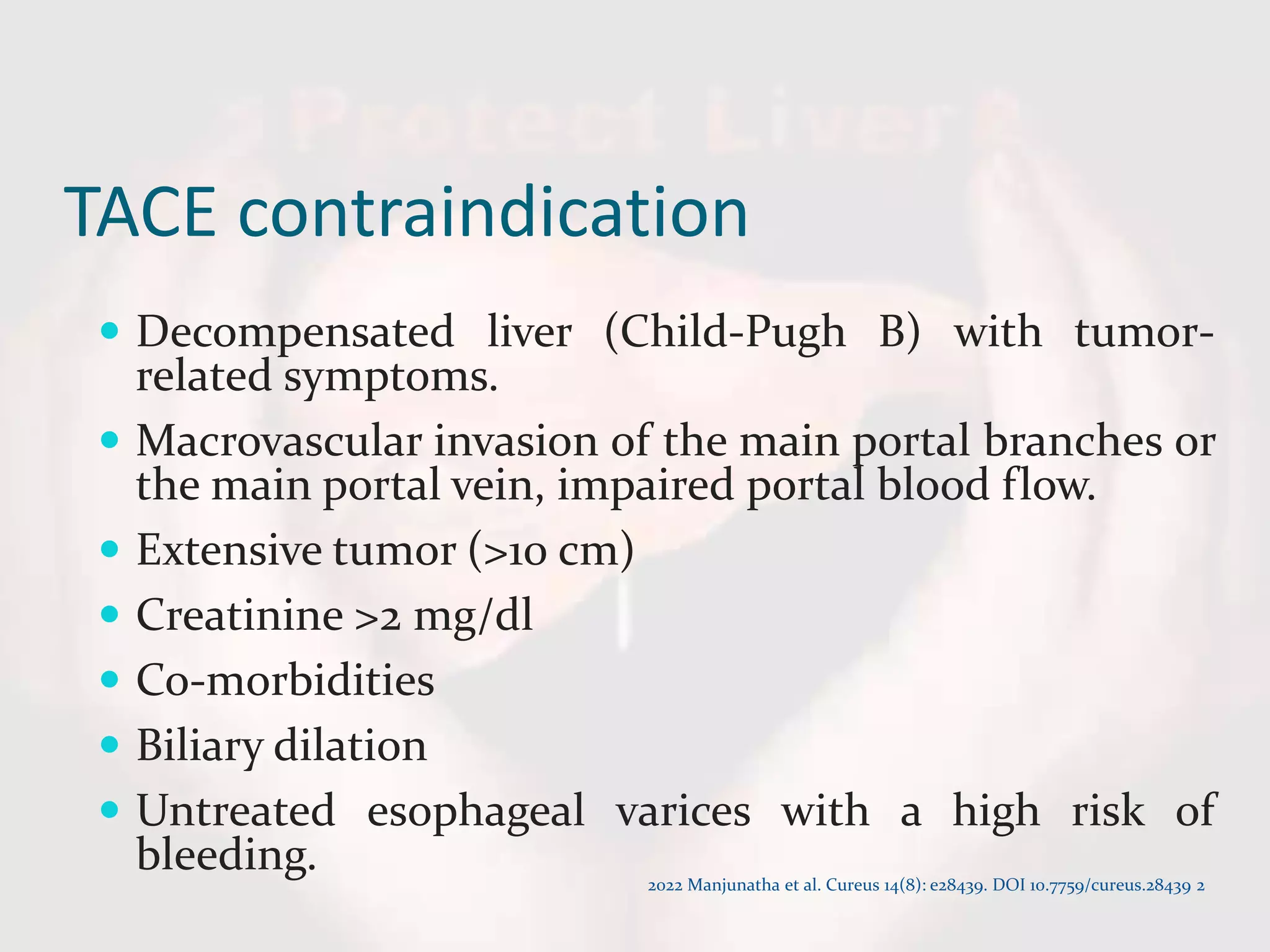
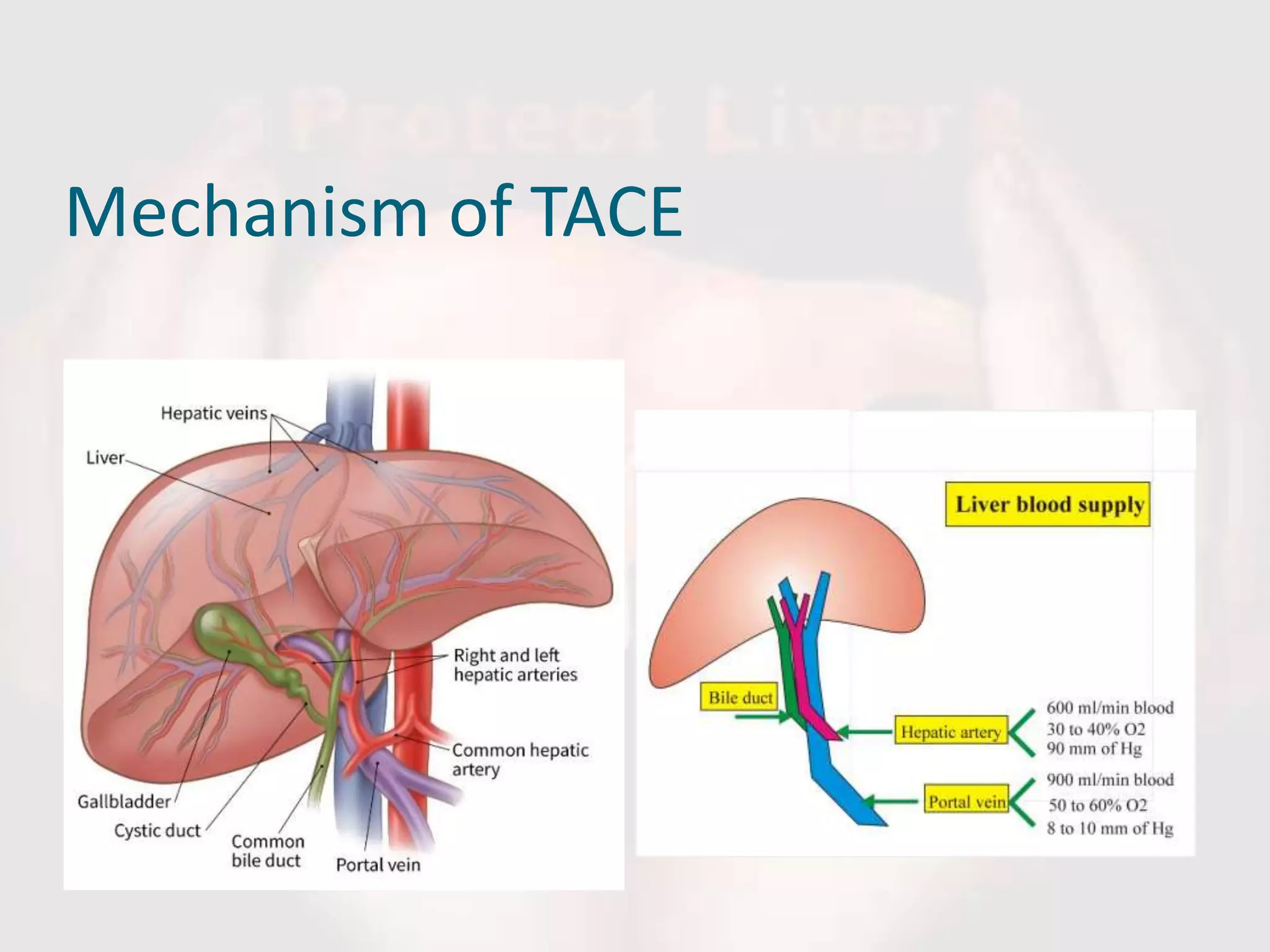
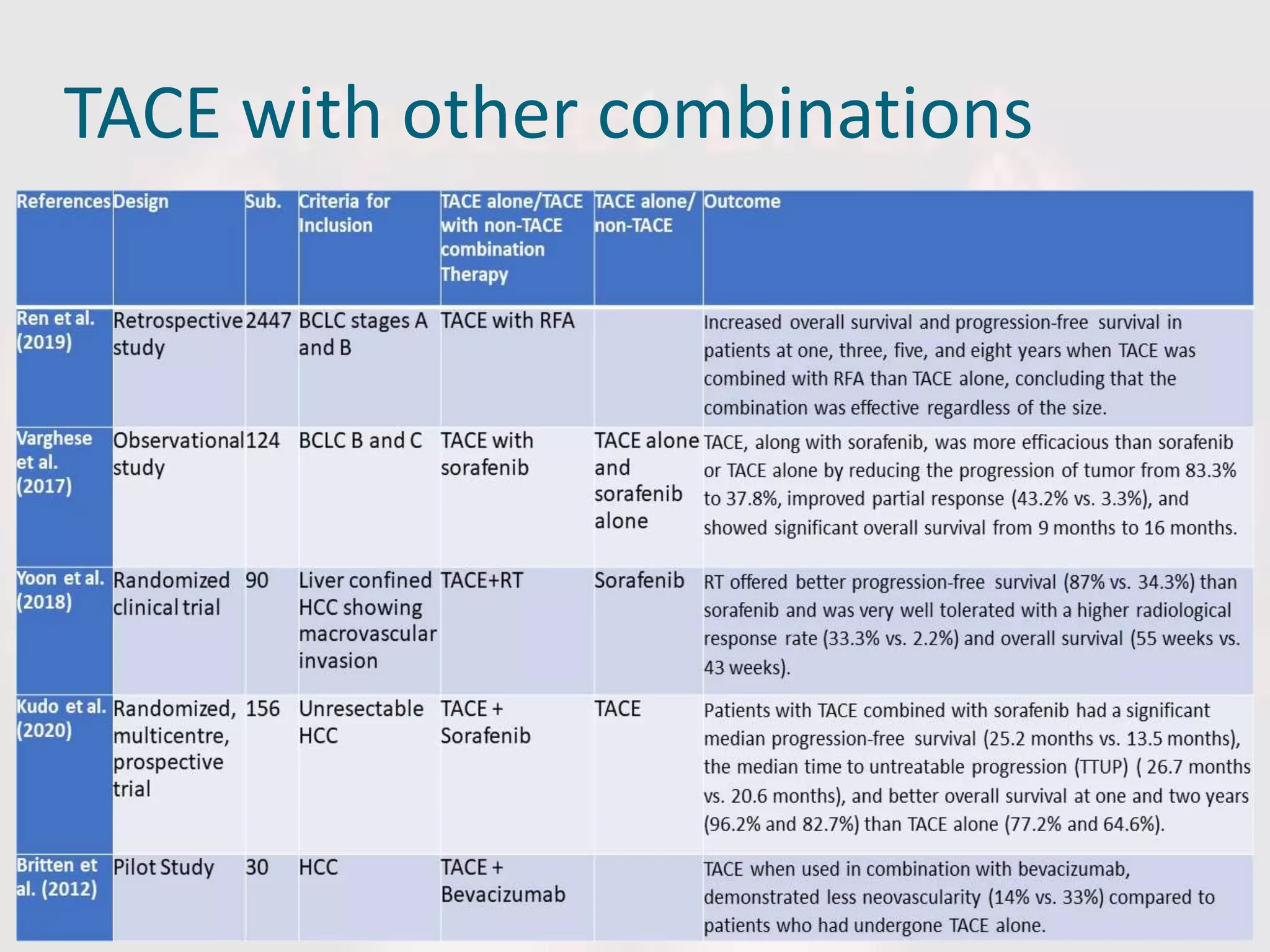
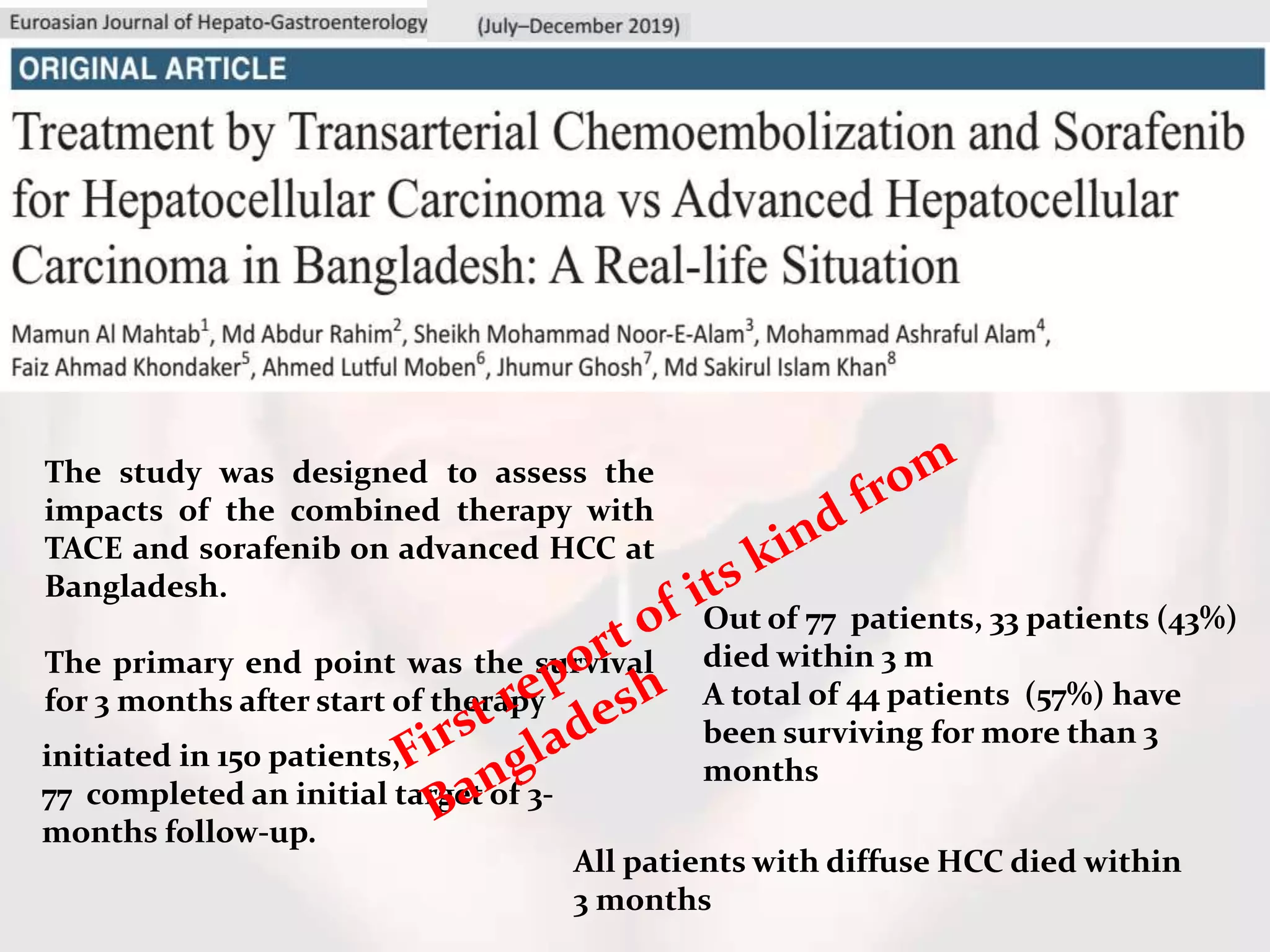
This document provides an overview of transarterial chemoembolization (TACE) for the treatment of hepatocellular carcinoma (HCC). It discusses patient selection criteria for TACE, the mechanism by which it works, details of the procedure, potential adverse effects and treatment schedules. TACE selectively cuts off the arterial blood supply to tumors while preserving liver function. The document also reviews experiences with TACE at hospitals in Bangladesh and combinations of TACE with other therapies. Proper patient selection and further study of combination approaches are emphasized as important areas for improving HCC management.