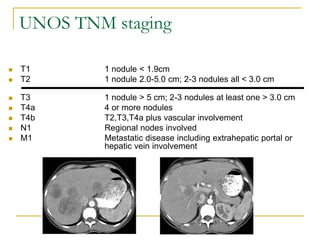
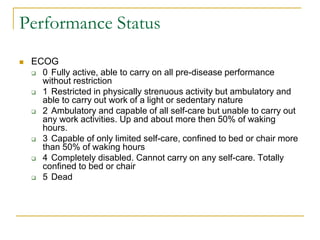
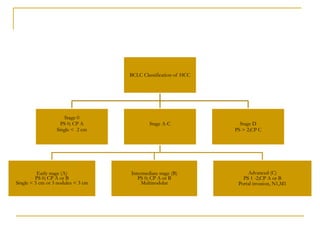
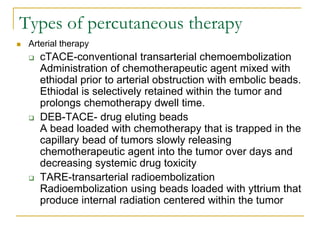
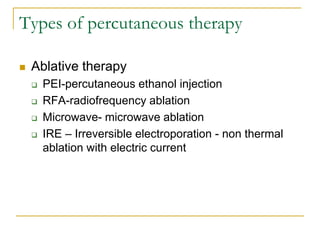
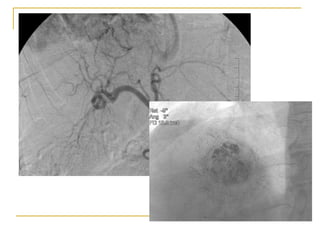
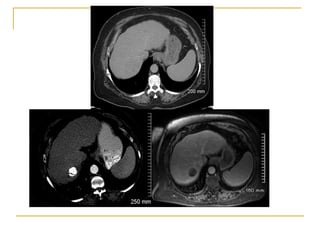
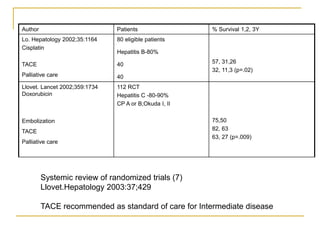
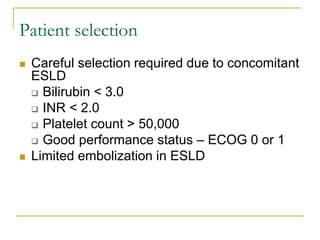
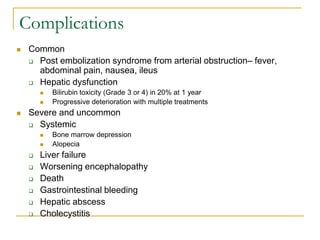
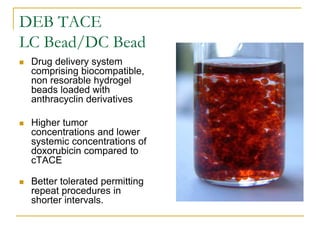
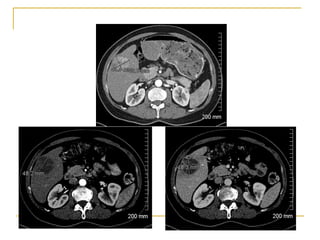
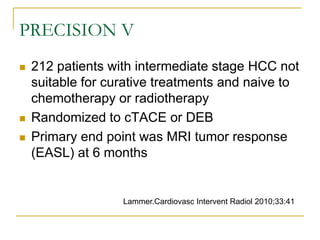
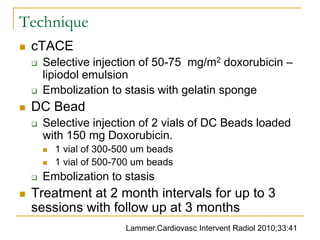
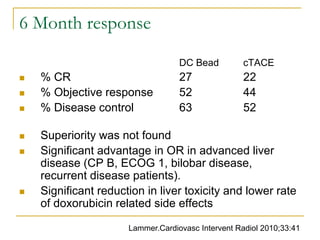
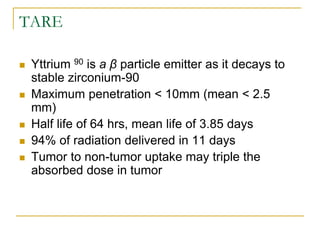
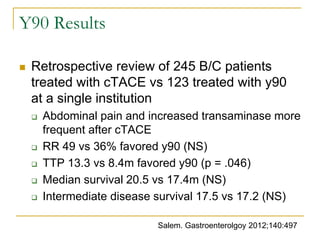
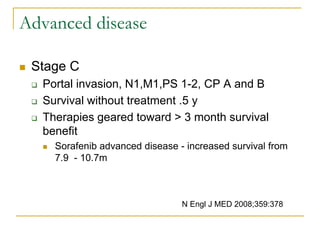
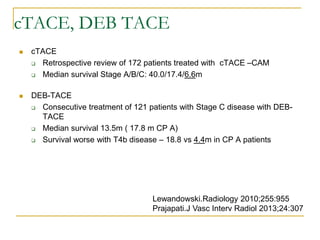
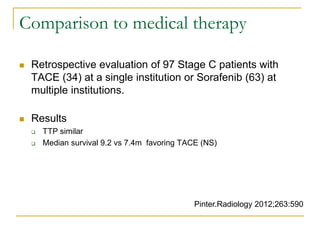
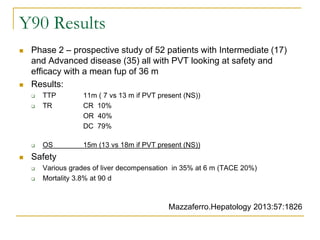
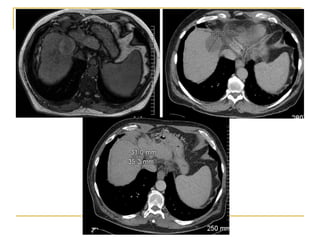
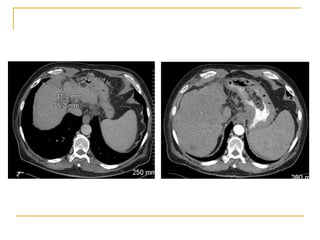
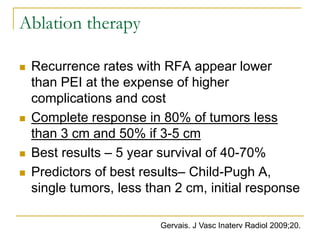
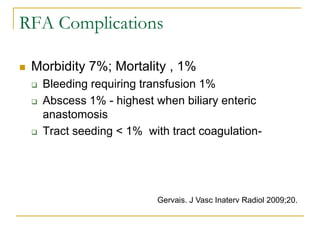
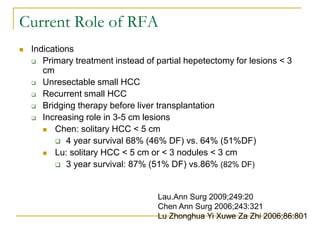
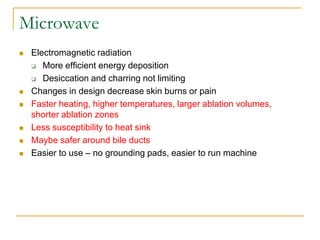
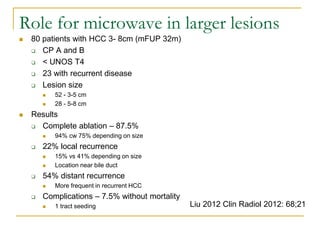
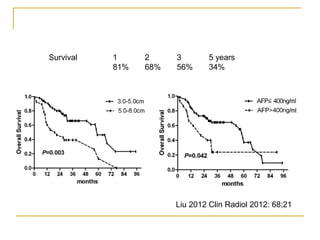
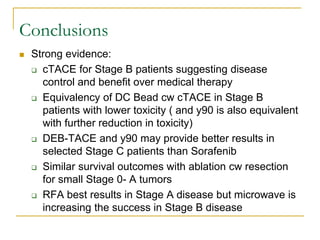
This document discusses treatment options for hepatocellular carcinoma (HCC), focusing on transarterial chemoembolization (TACE) and radiofrequency ablation (RFA). It stratifies HCC using the Barcelona criteria and examines prognostic factors. For intermediate stage HCC, TACE is the standard treatment and can provide 1, 2, and 3 year survival rates of 57%, 31%, and 26% respectively. Newer techniques like drug-eluting bead TACE may have fewer side effects than conventional TACE. RFA provides the best results for tumors under 3cm, with a 5 year survival of 40-70% for eligible patients. The document compares various locoregional therapies and their roles based on